Ewha Med J.
2024 Oct;47(4):e52. 10.12771/emj.2024.e52.
Update on sexually transmitted infections in Korea: a narrative review
- Affiliations
-
- 1Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Ewha Womans University Seoul Hospital, Seoul, Korea
- KMID: 2561410
- DOI: http://doi.org/10.12771/emj.2024.e52
Abstract
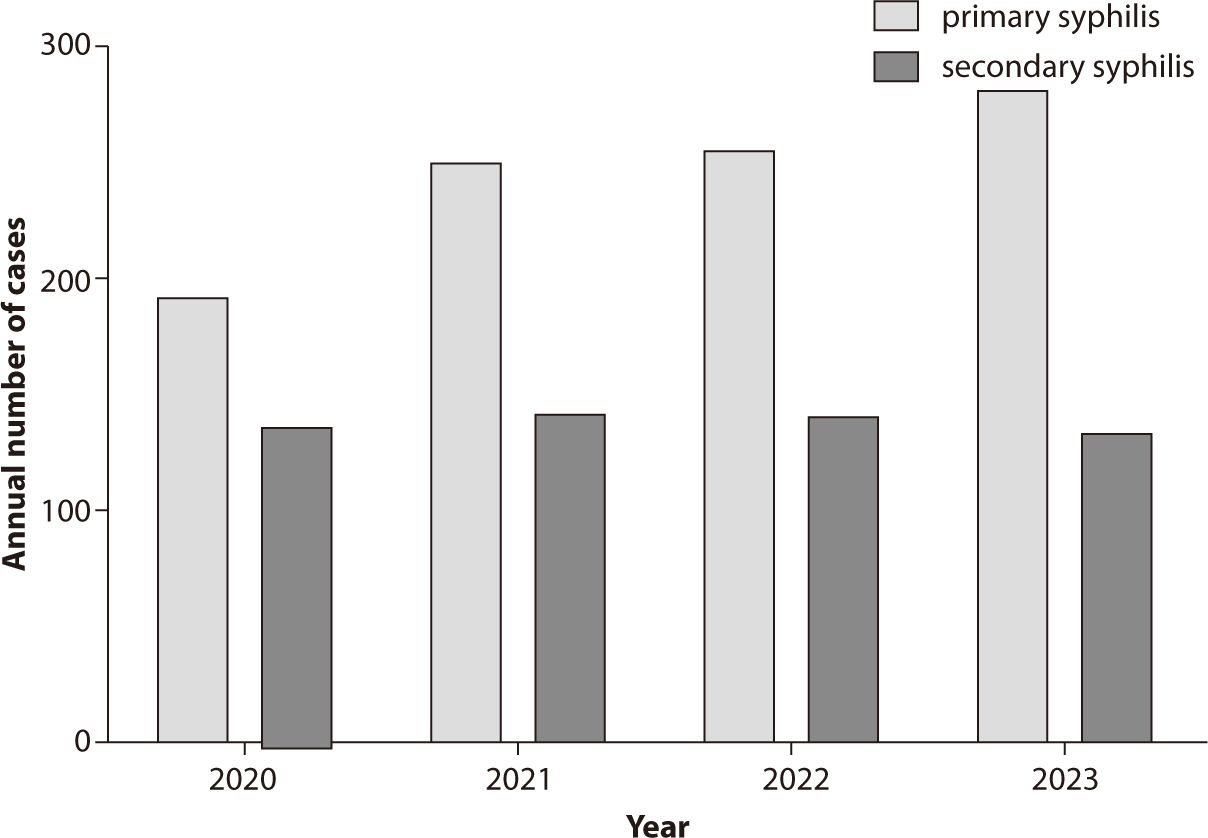
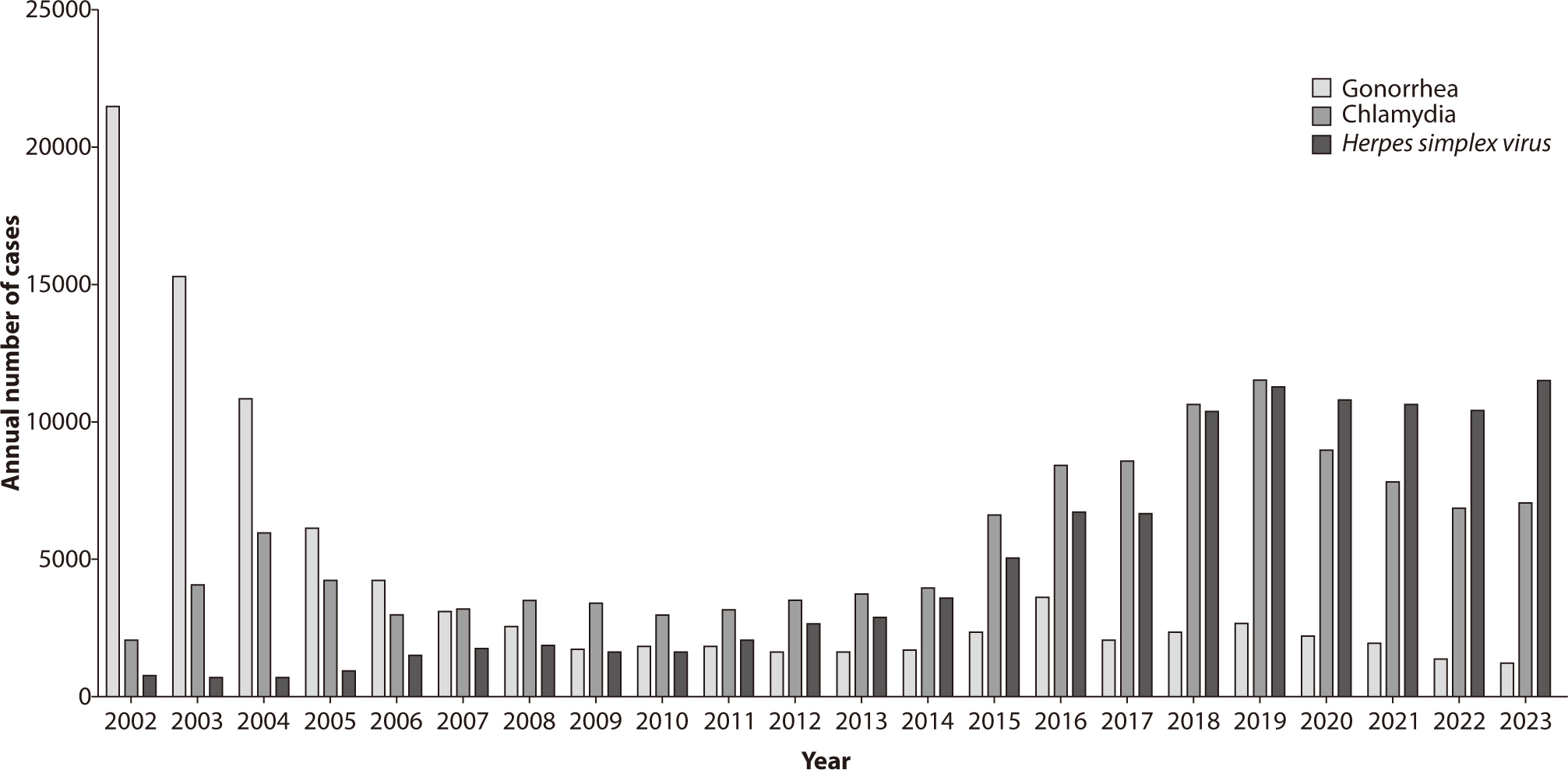
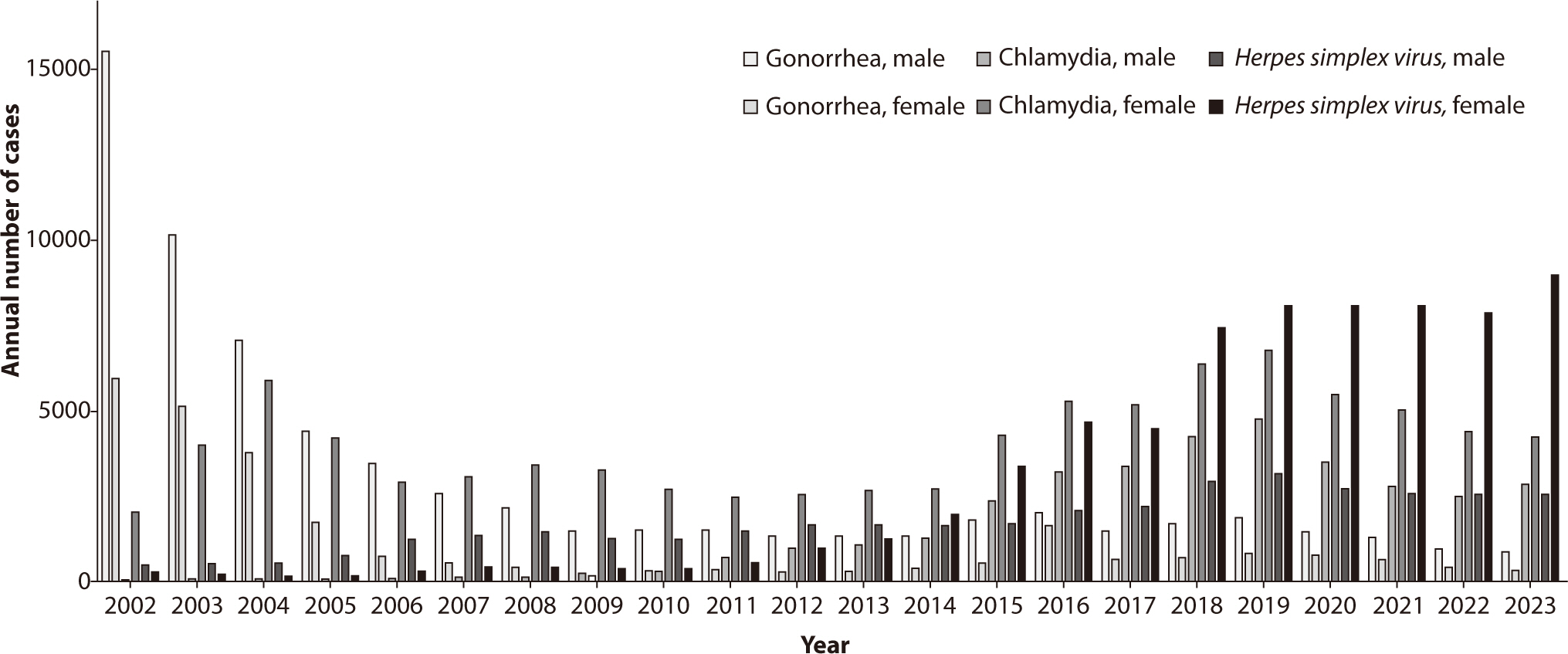
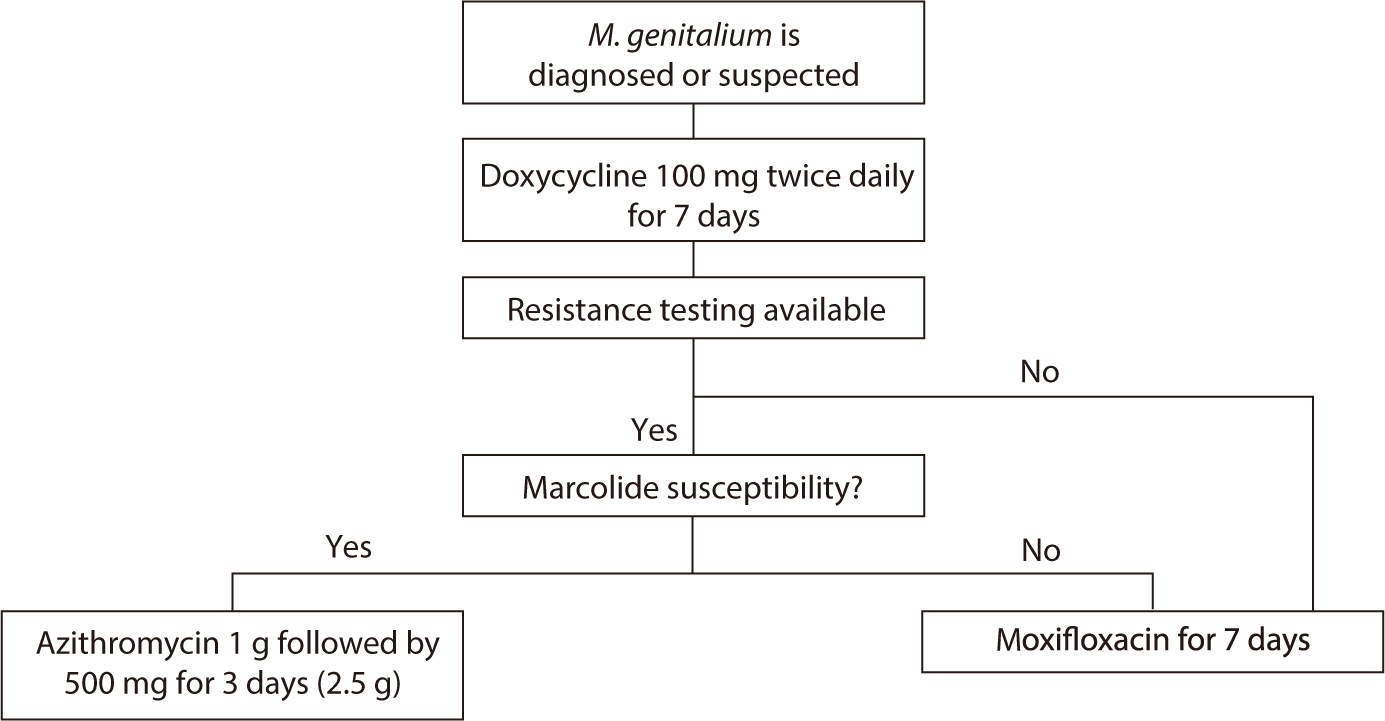
- Sexually transmitted infections (STIs) continue to pose significant public health challenges in Korea, with syphilis, gonorrhea, chlamydia, Mycoplasma genitalium, and herpes simplex virus (HSV) being the most prevalent. This review provides an updated overview of the epidemiology, diagnosis, and treatment of these significant STIs in Korea, highlighting recent trends and concerns. Syphilis incidence rates have fluctuated due to changes in surveillance systems. Starting in 2024, syphilis will be reclassified as a nationally notifiable infectious disease (category 2). Gonorrhea remains a concern due to increasing antibiotic resistance, including the emergence of extensively drug-resistant Neisseria gonorrhoeae strains, underscoring the need for vigilant antimicrobial stewardship. Chlamydia continues to be the most commonly reported STI, although its incidence has declined during the COVID-19 pandemic. M. genitalium has gained attention as a significant STI with rising antibiotic resistance issues, necessitating updated treatment guidelines and consideration of resistance testing. HSV-2 remains a common cause of genital herpes, with steady incidence rates reported. Updated diagnostic methods, including nucleic acid amplification tests, and revised treatment guidelines are presented to effectively address these infections. The impact of the COVID-19 pandemic on other STIs within Korea remains unclear, necessitating further research. Changes in treatment guidelines, such as the recommendation of doxycycline as first-line therapy for chlamydia, reflect evolving evidence and resistance patterns. The importance of updated diagnostic tools, including resistance testing for M. genitalium , is emphasized to improve treatment outcomes. Continued efforts in education, prevention, and research are essential to manage and mitigate the impact of STIs on public health in Korea.
Keyword
Figure
Reference
-
References
1. U.S. Department of Health and Human Services. Sexually transmitted infections national strategic plan for the United States: 2021–2025. Washington: U.S. Department of Health and Human Services;2020.2. Workowski KA. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021; 70(4):1–187. DOI: 10.15585/mmwr.rr7004a1. PMID: 34292926. PMCID: PMC8344968.3. World Health Organization. Guidelines for the management of symptomatic sexually transmitted infections. Geneva: World Health Organization;2021.4. Gamoudi D, Flew S, Cusini M, Benardon S, Poder A, Radcliffe K. 2018 European guideline on the organization of a consultation for sexually transmitted infections. J Eur Acad Dermatol Venereol. 2019; 33(8):1452–1458. DOI: 10.1111/jdv.15577. PMID: 30968975.
Article5. Wood GE, Bradshaw CS, Manhart LE. Update in epidemiology and management of Mycoplasma genitalium infections. Infect Dis Clin North Am. 2023; 37(2):311–333. DOI: 10.1016/j.idc.2023.02.009. PMID: 37105645.
Article6. Lee J, Kim Y, Choi JY. Impact of the COVID-19 pandemic on HIV services in Korea: results from a cross-sectional online survey. Infect Chemother. 2021; 53(4):741–752. DOI: 10.3947/ic.2021.0112. PMID: 34979605. PMCID: PMC8731254.
Article7. Seong H, Choi Y, Ahn KH, Choi JY, Kim SW, Kim SI, et al. Assessment of disease burden and immunization rates for vaccine-preventable diseases in people living with HIV: the Korea HIV/AIDS cohort study. Infect Chemother. 2023; 55(4):441–450. DOI: 10.3947/ic.2023.0045. PMID: 37674339. PMCID: PMC10771952.
Article8. Lee M, Park WB, Kim ES, Kim Y, Park SW, Lee E, et al. Possibility of decreasing incidence of human immunodeficiency virus infection in Korea. Infect Chemother. 2023; 55(4):451–459. DOI: 10.3947/ic.2023.0056. PMID: 37674340. PMCID: PMC10771950.
Article9. Park JK, Shin YS. Risk factors for urethral condyloma among heterosexual young male patients with condyloma acuminatum of penile skin. Infect Chemother. 2016; 48(3):216–218. DOI: 10.3947/ic.2016.48.3.216. PMID: 27659432. PMCID: PMC5048003.
Article10. Rothschild BM. History of syphilis. Clin Infect Dis. 2005; 40(10):1454–1463. DOI: 10.1086/429626. PMID: 15844068.
Article11. Wang S, Kim S, Cho S, Kim HS, Min S. Introduction to the transition of mandatory surveillance system in the syphilis monitoring. Public Health Wkly Rep. 2023; 16(47):1620–1630. DOI: 10.56786/PHWR.2023.16.47.3.12. Ghanem KG, Ram S, Rice PA. The modern epidemic of syphilis. N Engl J Med. 2020; 382(9):845–854. DOI: 10.1056/NEJMra1901593. PMID: 32101666.
Article13. Tuddenham S, Hamill MM, Ghanem KG. Diagnosis and treatment of sexually transmitted infections: a review. JAMA. 2022; 327(2):161–172. DOI: 10.1001/jama.2021.23487. PMID: 35015033.
Article14. Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: a systematic review. JAMA. 2014; 312(18):1905–1917. DOI: 10.1001/jama.2014.13259. PMID: 25387188. PMCID: PMC6690208.15. Butler T. The Jarisch–Herxheimer reaction after antibiotic treatment of spirochetal infections: a review of recent cases and our understanding of pathogenesis. Am J Trop Med Hyg. 2017; 96(1):46–52. DOI: 10.4269/ajtmh.16-0434. PMID: 28077740. PMCID: PMC5239707.
Article16. Choi JK, Lee SJ, Yoo JH. History of syphilis and gonorrhea in Korea. Infect Chemother. 2019; 51(2):210–216. DOI: 10.3947/ic.2019.51.2.210. PMID: 31271002. PMCID: PMC6609744.
Article17. Unemo M, Lahra MM, Escher M, Eremin S, Cole MJ, Galarza P, et al. WHO global antimicrobial resistance surveillance for Neisseria gonorrhoeae 2017–18: a retrospective observational study. Lancet Microbe. 2021; 2(11):E627–E636. DOI: 10.1016/S2666-5247(21)00171-3. PMID: 35544082.18. Kueakulpattana N, Wannigama DL, Luk-in S, Hongsing P, Hurst C, Badavath VN, et al. Multidrug-resistant Neisseria gonorrhoeae infection in heterosexual men with reduced susceptibility to ceftriaxone, first report in Thailand. Sci Rep. 2021; 11(1):21659. DOI: 10.1038/s41598-021-00675-y. PMID: 34737332. PMCID: PMC8569152.19. Pleininger S, Indra A, Golparian D, Heger F, Schindler S, Jacobsson S, et al. Extensively drug-resistant (XDR) Neisseria gonorrhoeae causing possible gonorrhoea treatment failure with ceftriaxone plus azithromycin in Austria, April 2022. Eurosurveill. 2022; 27(24):2200455. DOI: 10.2807/1560-7917.ES.2022.27.24.2200455. PMID: 35713023. PMCID: PMC9205165.20. Yun IJ, Park HJ, Chae J, Heo SJ, Kim YC, Kim B, et al. Nationwide analysis of antimicrobial prescription in Korean hospitals between 2018 and 2021: the 2023 KONAS report. Infect Chemother. 2024; 56(2):256–265. DOI: 10.3947/ic.2024.0013. PMID: 38960739. PMCID: PMC11224044.
Article21. Lee H, Hong SG, Soe Y, Yong D, Jeong SH, Lee K, et al. Trends in antimicrobial resistance of Neisseria gonorrhoeae isolated from Korean patients from 2000 to 2006. Sex Transm Dis. 2011; 38(11):1082–1086. DOI: 10.1097/OLQ.0b013e31822e60a4. PMID: 21992988.
Article22. Lee H, Unemo M, Kim HJ, Seo Y, Lee K, Chong Y. Emergence of decreased susceptibility and resistance to extended-spectrum cephalosporins in Neisseria gonorrhoeae in Korea. J Antimicrob Chemother. 2015; 70(9):2536–2542. DOI: 10.1093/jac/dkv146. PMID: 26084303. PMCID: PMC4539094.
Article23. Detels R, Green AM, Klausner JD, Katzenstein D, Gaydos C, Handsfield H, et al. The incidence and correlates of symptomatic and asymptomatic Chlamydia trachomatis and Neisseria gonorrhoeae infections in selected populations in five countries. Sex Transm Dis. 2011; 38(6):503–509. DOI: 10.1097/OLQ.0b013e318206c288. PMID: 22256336. PMCID: PMC3408314.
Article24. Lee MH, Byun J, Jung M, Yang JJ, Park KH, Moon S, et al. Disseminated gonococcal infection presenting as bacteremia and liver abscesses in a healthy adult. Infect Chemother. 2015; 47(1):60–63. DOI: 10.3947/ic.2015.47.1.60. PMID: 25844265. PMCID: PMC4384456.
Article25. Nettleton WD, Kent JB, Macomber K, Brandt MG, Jones K, Ridpath AD, et al. Notes from the field: ongoing cluster of highly related disseminated gonococcal infections: Southwest Michigan, 2019. Morb Mortal Wkly Rep. 2020; 69(12):353–354. DOI: 10.15585/mmwr.mm6912a5. PMID: 32214085. PMCID: PMC7725508.
Article26. Centers for Disease Control and Prevention. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae: 2014. MMWR Recomm Rep. 2014; 63(RR02):1–19.27. Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2018. Atlanta: U.S. Department of Health and Human Services;2019.28. Chan PA, Robinette A, Montgomery M, Almonte A, Cu-Uvin S, Lonks JR, et al. Extragenital infections caused by Chlamydia trachomatis and Neisseria gonorrhoeae: a review of the literature. Infect Dis Obstet Gynecol. 2016; 2016(1):5758387. DOI: 10.1155/2016/5758387. PMID: 27366021. PMCID: PMC4913006.29. Stoner BP, Cohen SE. Lymphogranuloma venereum 2015: clinical presentation, diagnosis, and treatment. Clin Infect Dis. 2015; 61(suppl_8):S865–S873. DOI: 10.1093/cid/civ756. PMID: 26602624.30. Geisler WM, Uniyal A, Lee JY, Lensing SY, Johnson S, Perry RCW, et al. Azithromycin versus doxycycline for urogenital chlamydia trachomatis infection. N Engl J Med. 2015; 373(26):2512–2521. DOI: 10.1056/NEJMoa1502599. PMID: 26699167. PMCID: PMC4708266.
Article31. Dombrowski JC, Wierzbicki MR, Newman LM, Powell JA, Miller A, Dithmer D, et al. Doxycycline versus azithromycin for the treatment of rectal chlamydia in men who have sex with men: a randomized controlled trial. Clin Infect Dis. 2021; 73(5):824–831. DOI: 10.1093/cid/ciab153. PMID: 33606009. PMCID: PMC8571563.
Article32. Lau A, Kong FYS, Fairley CK, Templeton DJ, Amin J, Phillips S, et al. Azithromycin or doxycycline for asymptomatic rectal Chlamydia trachomatis. N Engl J Med. 2021; 384(25):2418–2427. DOI: 10.1056/NEJMoa2031631. PMID: 34161706.
Article33. Suzuki S, Hoshi S, Sagara Y, Sekizawa A, Kinoshita K, Kitamura T. Antimicrobial resistance for Chlamydia trachomatis genital infection during pregnancy in Japan. Infect Chemother. 2022; 54(1):173–175. DOI: 10.3947/ic.2022.0030. PMID: 35384428. PMCID: PMC8987183.
Article34. Workowski KA. Centers for disease control and prevention sexually transmitted diseases treatment guidelines. Clin Infect Dis. 2015; 61(suppl_8):S759–S762. DOI: 10.1093/cid/civ771. PMID: 26602614.35. Kim HJ, Park JK, Park SC, Kim YG, Choi H, Ko JI, et al. The prevalence of causative organisms of community-acquired urethritis in an age group at high risk for sexually transmitted infections in Korean soldiers. BMJ Mil Health. 2017; 163(1):20–22. DOI: 10.1136/jramc-2015-000488. PMID: 26607860.
Article36. Oh EJ, Jang TS, Kim JK. Mycoplasma genitalium and Mycoplasma hominis infection in South Korea during 2018-2020. Iran J Microbiol. 2021; 13(5):602–607. DOI: 10.18502/ijm.v13i5.7423. PMID: 34900157. PMCID: PMC8629812.37. Seña AC, Lensing S, Rompalo A, Taylor SN, Martin DH, Lopez LM, et al. Chlamydia trachomatis, Mycoplasma genitalium, and Trichomonas vaginalis infections in men with nongonococcal urethritis: predictors and persistence after therapy. J Infect Dis. 2012; 206(3):357–365. DOI: 10.1093/infdis/jis356. PMID: 22615318. PMCID: PMC3490700.38. Soni S, Horner P, Rayment M, Pinto-Sander N, Naous N, Parkhouse A, et al. British Association for Sexual Health and HIV national guideline for the management of infection with Mycoplasma genitalium (2018). Int J STD AIDS. 2019; 30(10):938–950. DOI: 10.1177/0956462419825948. PMID: 31280688.
Article39. Gnann JW Jr, Whitley RJ. Genital herpes. N Engl J Med. 2016; 375(19):1906. DOI: 10.1056/NEJMc1611877.
Article40. Corey L, Adams HG, Brown ZA, Holmes KK. Genital herpes simplex virus infections: clinical manifestations, course, and complications. Ann Intern Med. 1983; 98(6):958–972. DOI: 10.7326/0003-4819-98-6-958. PMID: 6344712.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sexually Transmitted Diseases and the Role of Dermatologists
- Sexually transmitted diseases
- Guidelines for Medical Treatment of Sexually Transmitted Diseases in Gynecologic Clinics
- A survey on the clinical practice and the guidelines for sexually transmitted infections in Korea
- Sexually Transmitted Infections and Sexual Function in Relation to Male Fertility