Ewha Med J.
2024 Oct;47(4):e49. 10.12771/emj.2024.e49.
Challenges and opportunities to integrate artificial intelligence in radiation oncology: a narrative review
- Affiliations
-
- 1Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2561405
- DOI: http://doi.org/10.12771/emj.2024.e49
Abstract
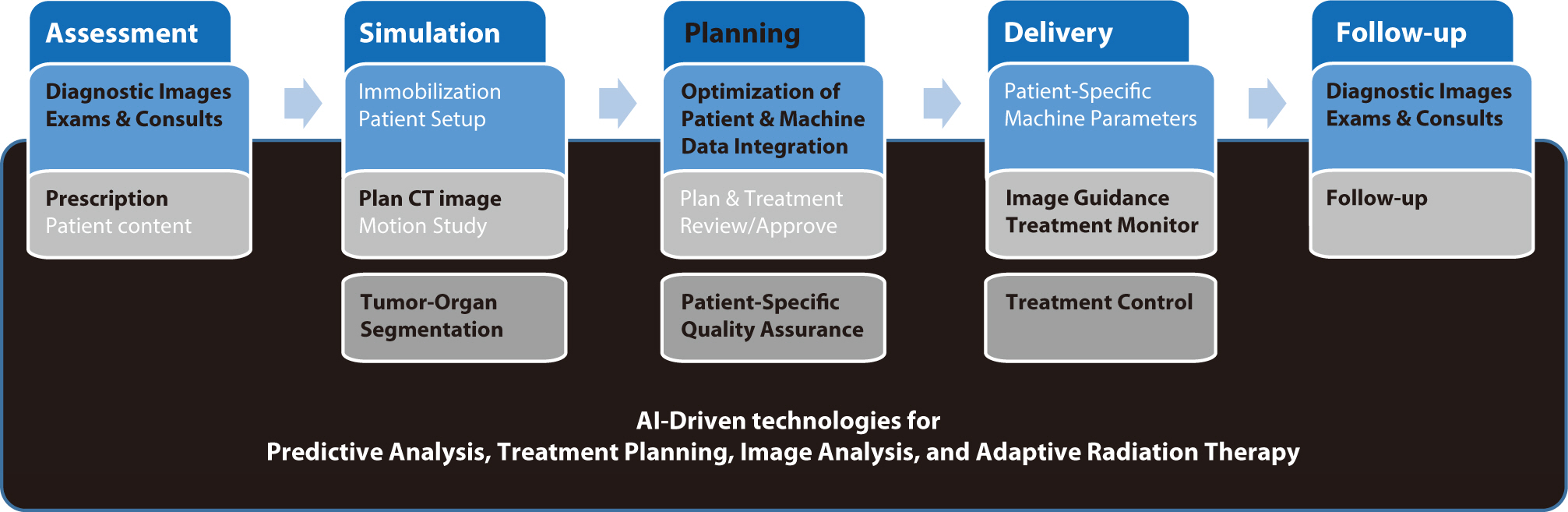
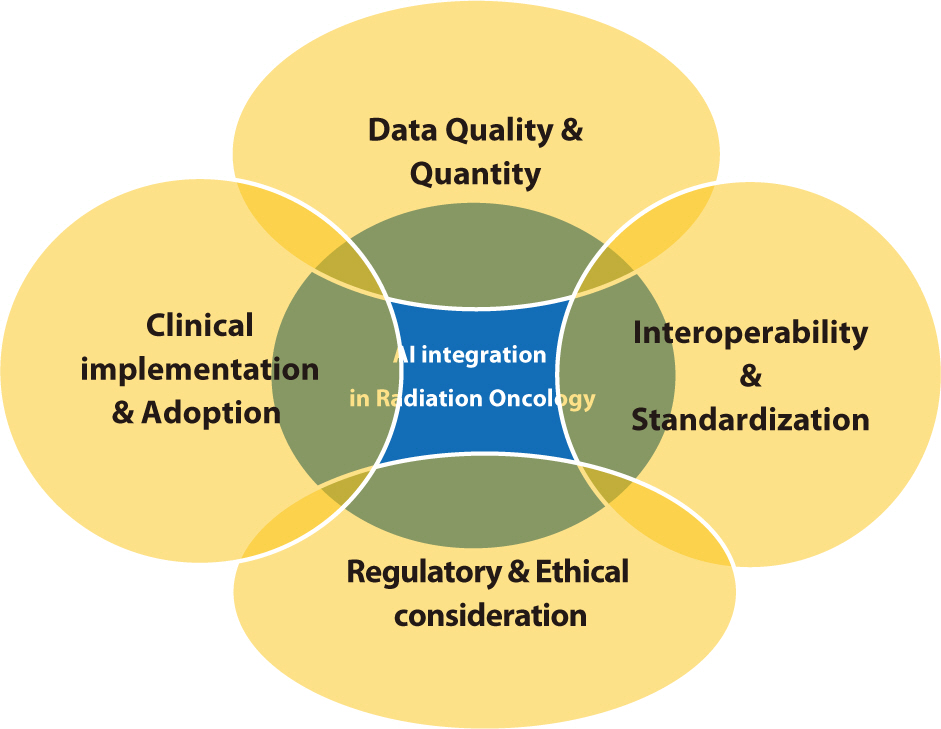
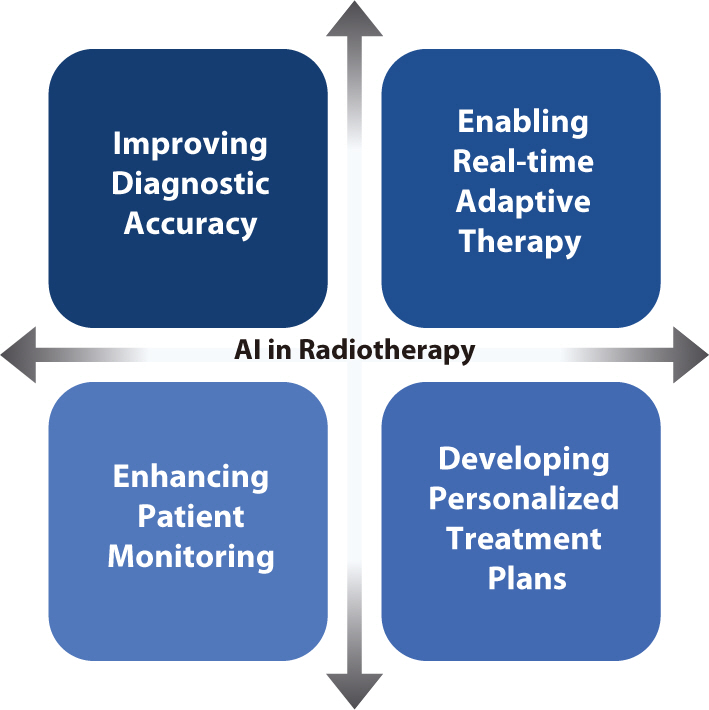
- Artificial intelligence (AI) is rapidly transforming various medical fields, including radiation oncology. This review explores the integration of AI into radiation oncology, highlighting both challenges and opportunities. AI can improve the precision, efficiency, and outcomes of radiation therapy by optimizing treatment planning, enhancing image analysis, facilitating adaptive radiation therapy, and enabling predictive analytics. Through the analysis of large datasets to identify optimal treatment parameters, AI can automate complex tasks, reduce planning time, and improve accuracy. In image analysis, AI-driven techniques enhance tumor detection and segmentation by processing data from CT, MRI, and PET scans to enable precise tumor delineation. In adaptive radiation therapy, AI is beneficial because it allows real-time adjustments to treatment plans based on changes in patient anatomy and tumor size, thereby improving treatment accuracy and effectiveness. Predictive analytics using historical patient data can predict treatment outcomes and potential complications, guiding clinical decision-making and enabling more personalized treatment strategies. Challenges to AI adoption in radiation oncology include ensuring data quality and quantity, achieving interoperability and standardization, addressing regulatory and ethical considerations, and overcoming resistance to clinical implementation. Collaboration among researchers, clinicians, data scientists, and industry stakeholders is crucial to overcoming these obstacles. By addressing these challenges, AI can drive advancements in radiation therapy, improving patient care and operational efficiencies. This review presents an overview of the current state of AI integration in radiation oncology and insights into future directions for research and clinical practice.
Keyword
Figure
Cited by 1 articles
-
Cutting-edge technologies in external radiation therapy
Jun Won Kim
Ewha Med J. 2024;47(4):e59. doi: 10.12771/emj.2024.e59.
Reference
-
References
1. Chun SG, Hu C, Komaki RU, Timmerman RD, Schild SE, Bogart JA, et al. Long-term prospective outcomes of intensity modulated radiotherapy for locally advanced lung cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2024; 10(8):1111–1115. DOI: 10.1001/jamaoncol.2024.1841. PMID: 38935373.
Article2. Fathy MM, Hassan BZ, El-Gebaly RH, Mokhtar MH. Dosimetric evaluation study of IMRT and VMAT techniques for prostate cancer based on different multileaf collimator designs. Radiat Environ Biophys. 2023; 62(1):97–106. DOI: 10.1007/s00411-022-01011-2. PMID: 36576578. PMCID: PMC9950215.
Article3. Mohan G, Ayisha Hamna TP, Jijo AJ, Saradha Devi KM, Narayanasamy A, Vellingiri B. Recent advances in radiotherapy and its associated side effects in cancer: a review. J Basic Appl Zool. 2019; 80(1):1–10. DOI: 10.1186/s41936-019-0083-5.4. Zaorsky NG, Harrison AS, Trabulsi EJ, Gomella LG, Showalter TN, Hurwitz MD, et al. Evolution of advanced technologies in prostate cancer radiotherapy. Nat Rev Urol. 2013; 10(10):565–579. DOI: 10.1038/nrurol.2013.185. PMID: 24018567.
Article5. Lim DH. Localized intracranial germinoma: is it time to re-define target volume for whole ventricular irradiation? Radiat Oncol J. 2023; 41(2):59–60. DOI: 10.3857/roj.2023.00423. PMID: 37403347. PMCID: PMC10326506.
Article6. Yu JI. Myxoid liposarcoma: a well-defined clinical target variant in radiotherapy for soft tissue sarcoma. Radiat Oncol J. 2022; 40(4):213–215. DOI: 10.3857/roj.2022.00598. PMID: 36606298. PMCID: PMC9830037.
Article7. Teh BS, Woo SY, Butler EB. Intensity modulated radiation therapy (IMRT): a new promising technology in radiation oncology. Oncol. 1999; 4(6):433–442. DOI: 10.1634/theoncologist.4-6-433.
Article8. Scaringi C, Agolli L, Minniti G. Technical advances in radiation therapy for brain tumors. Anticancer Res. 2018; 38(11):6041–6045. DOI: 10.21873/anticanres.12954. PMID: 30396918.
Article9. Park SY, Kim J, Chun M, Ahn H, Park JM. Assessment of the modulation degrees of intensity-modulated radiation therapy plans. Radiat Oncol. 2018; 13:1–8. DOI: 10.1186/s13014-018-1193-9. PMID: 30545396. PMCID: PMC6293636.10. Tanaka Y, Hashimoto M, Ishigami M, Nakano M, Hasegawa T. Development of a novel delivery quality assurance system based on simultaneous verification of dose distribution and binary multi-leaf collimator opening in helical tomotherapy. Radiat Oncol. 2023; 18(1):180. DOI: 10.1186/s13014-023-02366-6. PMID: 37919745. PMCID: PMC10621123.11. Mandava A, Koppula V, Kandati M, Raju KVVN. Synchronous radiation-induced enterovesical and enterocervical fistulas in carcinoma of the uterine cervix. Radiat Oncol J. 2023; 41(4):297–300. DOI: 10.3857/roj.2023.00500. PMID: 38185935. PMCID: PMC10772593.
Article12. Kavanagh BD, Timmerman RD. Stereotactic radiosurgery and stereotactic body radiation therapy: an overview of technical considerations and clinical applications. Hematol Oncol Clin. 2006; 20(1):87–95. DOI: 10.1016/j.hoc.2006.01.009. PMID: 16580558.
Article13. Jia-Mahasap B, Madla C, Sripan P, Chitapanarux I, Tharavichitkul E, Chakrabandhu S, et al. Stereotactic radiosurgery for limited brain metastasis using three different techniques: helical tomotherapy, volumetric modulated arc therapy, and cone-based LINAC radiosurgery. Radiat Oncol J. 2022; 40(4):232–241. DOI: 10.3857/roj.2022.00136. PMID: 36606300. PMCID: PMC9830036.
Article14. Jaffray DA, Siewerdsen JH. Cone-beam computed tomography with a flat-panel imager: initial performance characterization. Med Phys. 2000; 27(6):1311–1323. DOI: 10.1118/1.599009. PMID: 10902561.
Article15. Balter JM, Kessler ML. Imaging and alignment for image-guided radiation therapy. J Clin Oncol. 2007; 25(8):931–937. DOI: 10.1200/JCO.2006.09.7998. PMID: 17350941.16. Kim J, Lee H, Wu HG, Chie EK, Kang HC, Park JM. Development of patient-controlled respiratory gating system based on visual guidance for magnetic-resonance image-guided radiation therapy. Med Phys. 2017; 44(9):4838–4846. DOI: 10.1002/mp.12447. PMID: 28675492.
Article17. Korreman S, Eriksen JG, Grau C. The changing role of radiation oncology professionals in a world of AI–just jobs lost–or a solution to the under-provision of radiotherapy? Clin Transl Radiat Oncol. 2021; 26:104–107. DOI: 10.1016/j.ctro.2020.04.012. PMID: 33364449. PMCID: PMC7752957.
Article18. Yang W, Williams JH, Hogan PF, Bruinooge SS, Rodriguez GI, Kosty MP, et al. Projected supply of and demand for oncologists and radiation oncologists through 2025: an aging, better-insured population will result in shortage. J Oncol Pract. 2014; 10(1):39–45. DOI: 10.1200/JOP.2013.001319. PMID: 24443733.
Article19. Kim TH. Has the growing evidence of radiotherapy for hepatocellular carcinoma increased the use of radiotherapy in elderly patients? Radiat Oncol J. 2023; 41(3):141–143. DOI: 10.3857/roj.2023.00710. PMID: 37793622. PMCID: PMC10556838.
Article20. Orszag PR. US health care reform: cost containment and improvement in quality. JAMA. 2016; 316(5):493–495. DOI: 10.1001/jama.2016.9876. PMID: 27400156.21. Sheng K. Artificial intelligence in radiotherapy: a technological review. Front Med. 2020; 14(4):431–449. DOI: 10.1007/s11684-020-0761-1. PMID: 32728877.22. Chakravarty K, Antontsev V, Bundey Y, Varshney J. Driving success in personalized medicine through AI-enabled computational modeling. Drug Discov Today. 2021; 26(6):1459–1465. DOI: 10.1016/j.drudis.2021.02.007. PMID: 33609781.
Article23. Weerarathna IN, Kamble AR, Luharia A. Artificial intelligence applications for biomedical cancer research: a review. Cureus. 2023; 15(11):e48307. DOI: 10.7759/cureus.48307.24. Yoo S, Sheng Y, Blitzblau R, McDuff S, Champ C, Morrison J, et al. Clinical experience with machine learning-based automated treatment planning for whole breast radiation therapy. Adv Radiat Oncol. 2021; 6(2):100656. DOI: 10.1016/j.adro.2021.100656. PMID: 33748540. PMCID: PMC7966969.25. Wang C, Zhu X, Hong JC, Zheng D. Artificial intelligence in radiotherapy treatment planning: present and future. Technol Cancer Res Treat. 2019; 18:1533033819873922. DOI: 10.1177/1533033819873922. PMID: 31495281. PMCID: PMC6732844.26. Kiser KJ, Fuller CD, Reed VK. Artificial intelligence in radiation oncology treatment planning: a brief overview. J Med Artif Intell. 2019; 2:9. DOI: 10.21037/jmai.2019.04.02.
Article27. Blumenfeld P, Arbit E, Den R, Salhab A, Falick Michaeli T, Wygoda M, et al. Real world clinical experience using daily intelligence-assisted online adaptive radiotherapy for head and neck cancer. Radiat Oncol. 2024; 19(1):43. DOI: 10.1186/s13014-024-02436-3. PMID: 38555453. PMCID: PMC10981810.28. Wang W, Sheng Y, Wang C, Zhang J, Li X, Palta M, et al. Fluence map prediction using deep learning models – direct plan generation for pancreas stereotactic body radiation therapy. Front Artif Intell. 2020; 3:68. DOI: 10.3389/frai.2020.00068. PMID: 33733185. PMCID: PMC7861344.29. Cai W, Ding S, Li H, Zhou X, Dou W, Zhou L, et al. Automatic IMRT treatment planning through fluence prediction and plan fine-tuning for nasopharyngeal carcinoma. Radiat Oncol. 2024; 19(1):39. DOI: 10.1186/s13014-024-02401-0. PMID: 38509540. PMCID: PMC10956235.30. Byrne M, Archibald-Heeren B, Hu Y, Teh A, Beserminji R, Cai E, et al. Varian ethos online adaptive radiotherapy for prostate cancer: early results of contouring accuracy, treatment plan quality, and treatment time. J Appl Clin Med Phys. 2022; 23(1):e13479. DOI: 10.1002/acm2.13479. PMID: 34846098. PMCID: PMC8803282.
Article31. Archambault Y, Boylan C, Bullock D, Morgas T, Peltola J, Ruokokoski E, et al. Making on-line adaptive radiotherapy possible using artificial intelligence and machine learning for efficient daily re-planning. Med Phys Int J. 2020; 8(2):77–86.32. Massat MB. Oncology EMRs: more than a patient record. Appl Radiat Oncol. 2016; (3):38–40. DOI: 10.37549/ARO1105.
Article33. Rayed ME, Islam SMS, Niha SI, Jim JR, Kabir MM, Mridha MF. Deep learning for medical image segmentation: state-of-the-art advancements and challenges. Inform Med Unlocked. 2024; 47:101504. DOI: 10.1016/j.imu.2024.101504.34. Hooshangnejad H, Feng X, Huang G, Zhang R, Kelly K, Chen Q, et al. EXACT-Net: EHR-guided lung tumor auto-segmentation for non-small cell lung cancer radiotherapy. arXiv: 2402.14099 [Preprint]. 2024.35. Atiya SU, Ramesh NVK. Enhancing non-small cell lung cancer radiotherapy planning: a deep learning-based multi-modal fusion approach for accurate GTV segmentation. Biomed Signal Process Control. 2024; 92:105987. DOI: 10.1016/j.bspc.2024.105987.36. Rai HM. Cancer detection and segmentation using machine learning and deep learning techniques: a review. Multimed Tools Appl. 2024; 83(9):27001–27035. DOI: 10.1007/s11042-023-16520-5.
Article37. Abo-El-Rejal A, Ayman SE, Aymen F. Advances in breast cancer segmentation: a comprehensive review. Acadlore Trans AI Mach Learn. 2024; 3(2):70–83. DOI: 10.56578/ataiml030201.38. Liu X, Qu L, Xie Z, Zhao J, Shi Y, Song Z. Towards more precise automatic analysis: a systematic review of deep learning-based multi-organ segmentation. BioMed Eng OnLine. 2024; 23(1):52. DOI: 10.1186/s12938-024-01238-8. PMID: 38851691. PMCID: PMC11162022.39. Zi Y, Wang Q, Gao Z, Cheng X, Mei T. Research on the application of deep learning in medical image segmentation and 3D reconstruction. Acad J Sci Technol. 2024; 10(2):8–12. DOI: 10.54097/0h77ge77.
Article40. Wang TW, Hong JS, Chiu HY, Chao HS, Chen YM, Wu YT. Standalone deep learning versus experts for diagnosis lung cancer on chest computed tomography: a systematic review. Eur Radiol. 2024; May. 22. [Epub]. DOI: 10.1007/s00330-024-10804-6. PMID: 38777902. PMCID: PMC11519296.41. Santhakumar G, Takale DG, Tyagi S, Anitha R, Tiwari M, Dhanraj JA. Analysis of multimodality fusion of medical image segmentation employing deep learning. In:. Joshi K, Kumar Gupta S, editors. editors. Human cancer diagnosis and detection using exascale computing. Beverly: Scrivener;2024. p. p. 171–183. DOI: 10.1002/9781394197705.ch11.
Article42. Wu Y, Luo X, Xu Z, Guo X, Ju L, Ge Z, et al. Diversified and personalized multi-rater medical image segmentation. arXiv: 2403.13417 [Preprint]. 2024; DOI: 10.1109/CVPR52733.2024.01090.43. Yu L, Min W, Wang S. Boundary-aware gradient operator network for medical image segmentation. IEEE J Biomed Health Inform. 2024; 28(8):4711–4723. DOI: 10.1109/JBHI.2024.3404273. PMID: 38776204.44. Eisenstein M. AI assistance for planning cancer treatment. Nature. 2024; 629(8014):S14–S16. DOI: 10.1038/d41586-024-01431-8. PMID: 38811703.
Article45. Kehayias CE, Yan Y, Bontempi D, Quirk S, Bitterman DS, Bredfeldt JS, et al. Prospective deployment of an automated implementation solution for artificial intelligence translation to clinical radiation oncology. Front Oncol. 2024; 13:1305511. DOI: 10.3389/fonc.2023.1305511. PMID: 38239639. PMCID: PMC10794768.46. Rayn K, Gokhroo G, Jeffers B, Gupta V, Chaudhari S, Clark R, et al. Multicenter study of pelvic nodal autosegmentation algorithm of Siemens Healthineers: comparison of male versus female pelvis. Adv Radiat Oncol. 2024; 9(2):101326. DOI: 10.1016/j.adro.2023.101326. PMID: 38405314. PMCID: PMC10885554.47. Schwartz DL, Dong L. Adaptive radiation therapy for head and neck cancer: can an old goal evolve into a new standard? J Oncol. 2011; 2011(1):690595. DOI: 10.1155/2011/690595. PMID: 20847944. PMCID: PMC2933914.48. Glide-Hurst CK, Lee P, Yock AD, Olsen JR, Cao M, Siddiqui F, et al. Adaptive radiation therapy (ART) strategies and technical considerations: a state of the ART review from NRG oncology. Int J Radiat Oncol Biol Phys. 2021; 109(4):1054–1075. DOI: 10.1016/j.ijrobp.2020.10.021. PMID: 33470210. PMCID: PMC8290862.
Article49. Liu H, Schaal D, Curry H, Clark R, Magliari A, Kupelian P, et al. Review of cone beam computed tomography based online adaptive radiotherapy: current trend and future direction. Radiat Oncol. 2023; 18(1):144. DOI: 10.1186/s13014-023-02340-2. PMID: 37660057. PMCID: PMC10475190.50. Wang YF, Price MJ, Elliston CD, Munbodh R, Spina CS, Horowitz DP, et al. Enhancing safety in AI-driven cone beam CT-based online adaptive radiation therapy: development and implementation of an interdisciplinary workflow. Adv Radiat Oncol. 2024; 9(3):101399. DOI: 10.1016/j.adro.2023.101399. PMID: 38292890. PMCID: PMC10823112.51. Sibolt P, Andersson LM, Calmels L, Sjöström D, Bjelkengren U, Geertsen P, et al. Clinical implementation of artificial intelligence-driven cone-beam computed tomography-guided online adaptive radiotherapy in the pelvic region. Phys Imaging Radiat Oncol. 2021; 17:1–7. DOI: 10.1016/j.phro.2020.12.004. PMID: 33898770. PMCID: PMC8057957.52. Winkel D, Bol GH, Kroon PS, van Asselen B, Hackett SS, Werensteijn-Honingh AM, et al. Adaptive radiotherapy: the Elekta Unity MR-linac concept. Clin Transl Radiat Oncol. 2019; 18:54–59. DOI: 10.1016/j.ctro.2019.04.001. PMID: 31341976. PMCID: PMC6630157.53. Badawy M, Ramadan N, Hefny HA. Healthcare predictive analytics using machine learning and deep learning techniques: a survey. J Electr Syst Inf Technol. 2023; 10(1):40. DOI: 10.1186/s43067-023-00108-y.54. Lee Y, Choi HJ, Kim H, Kim S, Kim MS, Cha H, et al. Feasibility of artificial intelligence-driven interfractional monitoring of organ changes by mega-voltage computed tomography in intensity-modulated radiotherapy of prostate cancer. Radiat Oncol J. 2023; 41(3):186–198. DOI: 10.3857/roj.2023.00444. PMID: 37793628. PMCID: PMC10556843.
Article55. Mijderwijk HJ, Steiger HJ. Predictive analytics in clinical practice: advantages and disadvantages. In:. Staartjes VE, Regli L, Serra C, editors. editors. Machine learning in clinical neuroscience: foundations and applications. Cham: Springer;2022. p. p. 263–268. DOI: 10.1007/978-3-030-85292-4_30. PMID: 34862550.56. Huang Y, Li J, Li M, Aparasu RR. Application of machine learning in predicting survival outcomes involving real-world data: a scoping review. BMC Med Res Methodol. 2023; 23(1):268. DOI: 10.1186/s12874-023-02078-1. PMID: 37957593. PMCID: PMC10641971.57. Somashekhar SP, Sepúlveda MJ, Puglielli S, Norden AD, Shortliffe EH, Kumar CR, et al. Watson for oncology and breast cancer treatment recommendations: agreement with an expert multidisciplinary tumor board. Ann Oncol. 2018; 29(2):418–423. DOI: 10.1093/annonc/mdx781. PMID: 29324970.
Article58. Tsang DS, Tsui G, Santiago AT, Keller H, Purdie T, Mcintosh C, et al. A prospective study of machine learning-assisted radiation therapy planning for patients receiving 54 Gy to the brain. Int J Radiat Oncol Biol Phys. 2024; 119(5):1429–1436. DOI: 10.1016/j.ijrobp.2024.02.022. PMID: 38432285.
Article59. Budach L, Feuerpfeil M, Ihde N, Nathansen A, Noack N, Patzlaff H, et al. The effects of data quality on machine learning performance. arXiv: 2207.14529 [Preprint]. 2022.60. Whang SE, Roh Y, Song H, Lee JG. Data collection and quality challenges in deep learning: a data-centric AI perspective. VLDB J. 2023; 32(4):791–813. DOI: 10.1007/s00778-022-00775-9.
Article61. Aldoseri A, Al-Khalifa KN, Hamouda AM. Re-thinking data strategy and integration for artificial intelligence: concepts, opportunities, and challenges. Appl Sci. 2023; 13(12):7082. DOI: 10.3390/app13127082.
Article62. Choi HS, Song JY, Shin KH, Chang JH, Jang BS. Developing prompts from large language model for extracting clinical information from pathology and ultrasound reports in breast cancer. Radiat Oncol J. 2023; 41(3):209–216. DOI: 10.3857/roj.2023.00633. PMID: 37793630. PMCID: PMC10556835.
Article63. Arasteh ST, Lotfinia M, Nolte T, Saehn M, Isfort P, Kuhl C, et al. Preserving privacy in domain transfer of medical AI models comes at no performance costs: the integral role of differential privacy. arXiv: 2306.06503 [Preprint]. 2023.64. Kessel KA, Combs SE. Data management, documentation and analysis systems in radiation oncology: a multi-institutional survey. Radiat Oncol. 2015; 10:1–6. DOI: 10.1186/s13014-015-0543-0. PMID: 26572494. PMCID: PMC4647666.65. Hughes N, Kalra D. Data standards and platform interoperability. In:. He W, Fang Y, Wang H, editors. editors. Real-world evidence in medical product development. Cham: Springer;2023. p. p. 79–107. DOI: 10.1007/978-3-031-26328-6_6. PMCID: PMC10098370.
Article66. Bukowski M, Farkas R, Beyan O, Moll L, Hahn H, Kiessling F, et al. Implementation of eHealth and AI integrated diagnostics with multidisciplinary digitized data: are we ready from an international perspective? Eur Radiol. 2020; 30:5510–5524. DOI: 10.1007/s00330-020-06874-x. PMID: 32377810. PMCID: PMC7476980.
Article67. Caffery LJ, Rotemberg V, Weber J, Soyer HP, Malvehy J, Clunie D. The role of DICOM in artificial intelligence for skin disease. Front Med. 2021; 7:619787. DOI: 10.3389/fmed.2020.619787. PMID: 33644087. PMCID: PMC7902872.68. Murdoch B. Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Med Ethics. 2021; 22:1–5. DOI: 10.1186/s12910-021-00687-3. PMID: 34525993. PMCID: PMC8442400.69. Pesapane F, Volonté C, Codari M, Sardanelli F. Artificial intelligence as a medical device in radiology: ethical and regulatory issues in Europe and the United States. Insights Imaging. 2018; 9:745–753. DOI: 10.1007/s13244-018-0645-y. PMID: 30112675. PMCID: PMC6206380.
Article70. Hasan HE, Jaber D, Khabour OF, Alzoubi KH. Ethical considerations and concerns in the implementation of AI in pharmacy practice: a cross-sectional study. BMC Med Ethics. 2024; 25(1):55. DOI: 10.1186/s12910-024-01062-8. PMID: 38750441. PMCID: PMC11096093.71. Mohammad Amini M, Jesus M, Fanaei Sheikholeslami D, Alves P, Hassanzadeh Benam A, Hariri F. Artificial intelligence ethics and challenges in healthcare applications: a comprehensive review in the context of the European GDPR mandate. Mach Learn Knowl Extr. 2023; 5(3):1023–1035. DOI: 10.3390/make5030053.
Article72. Duong MT, Rauschecker AM, Rudie JD, Chen PH, Cook TS, Bryan RN, et al. Artificial intelligence for precision education in radiology. Br J Radiol. 2019; 92(1103):20190389. DOI: 10.1259/bjr.20190389. PMID: 31322909. PMCID: PMC6849670.73. Talwar S, Dhir A, Islam N, Kaur P, Almusharraf A. Resistance of multiple stakeholders to e-health innovations: integration of fundamental insights and guiding research paths. J Bus Res. 2023; 166:114135. DOI: 10.1016/j.jbusres.2023.114135.74. van de Sande D, Van Genderen ME, Smit JM, Huiskens J, Visser JJ, Veen RER, et al. Developing, implementing and governing artificial intelligence in medicine: a step-by-step approach to prevent an artificial intelligence winter. BMJ Health Care Inform. 2022; 29(1):e100495. DOI: 10.1136/bmjhci-2021-100495. PMID: 35185012. PMCID: PMC8860016.75. Brady AP, Allen B, Chong J, Kotter E, Kottler N, Mongan J, et al. Developing, purchasing, implementing and monitoring AI tools in radiology: practical considerations. A multi-society statement from the ACR, CAR, ESR, RANZCR & RSNA. Can Assoc Radiol J. 2024; 75(2):226–244. DOI: 10.1177/08465371231222229. PMID: 38251882.
Article76. Huynh E, Hosny A, Guthier C, Bitterman DS, Petit SF, Haas-Kogan DA, et al. Artificial intelligence in radiation oncology. Nat Rev Clin Oncol. 2020; 17(12):771–781. DOI: 10.1038/s41571-020-0417-8. PMID: 32843739.
Article77. Kawamura M, Kamomae T, Yanagawa M, Kamagata K, Fujita S, Ueda D, et al. Revolutionizing radiation therapy: the role of AI in clinical practice. J Radiat Res. 2024; 65(1):1–9. DOI: 10.1093/jrr/rrad090. PMID: 37996085. PMCID: PMC10803173.78. Cui S, Ten Haken RK, El Naqa I. Integrating multiomics information in deep learning architectures for joint actuarial outcome prediction in non-small cell lung cancer patients after radiation therapy. Int J Radiat Oncol Biol Phys. 2021; 110(3):893–904. DOI: 10.1016/j.ijrobp.2021.01.042. PMID: 33539966. PMCID: PMC8180510.
Article79. Grass GD, Mills MN, Scott JG, Eschrich SA, Torres-Roca J. Genomics and radiomics: tools to see the unseen to personalize radiation therapy. Appl Radiat Oncol. 2019; 8:9–22. DOI: 10.37549/ARO1213.80. McGregor BA, Vidal GA, Shah SA, Mitchell JD, Hendifar AE. Remote oncology care: review of current technology and future directions. Cureus. 2020; 12(8):e10156. DOI: 10.7759/cureus.10156.81. Harvey H, Glocker B. A standardised approach for preparing imaging data for machine learning tasks in radiology. In:. Ranschaert ER, Morozov S, Algra PR, editors. editors. Artificial intelligence in medical imaging: opportunities, applications and risks. Cham: Springer;2019. p. p. 61–72. DOI: 10.1007/978-3-319-94878-2_6.
Article82. Wahid KA, Glerean E, Sahlsten J, Jaskari J, Kaski K, Naser MA, et al. Artificial intelligence for radiation oncology applications using public datasets. Semin Radiat Oncol. 2022; 32(4):400–414. DOI: 10.1016/j.semradonc.2022.06.009. PMID: 36202442. PMCID: PMC9587532.
Article83. Fraser AG, Biasin E, Bijnens B, Bruining N, Caiani EG, Cobbaert K, et al. Artificial intelligence in medical device software and high-risk medical devices: a review of definitions, expert recommendations and regulatory initiatives. Expert Rev Med Devices. 2023; 20(6):467–491. DOI: 10.1080/17434440.2023.2184685. PMID: 37157833.
Article84. Beckers R, Kwade Z, Zanca F. The EU medical device regulation: implications for artificial intelligence-based medical device software in medical physics. Phys Med. 2021; 83:1–8. DOI: 10.1016/j.ejmp.2021.02.011. PMID: 33657513.
Article85. Amann J, Blasimme A, Vayena E, Frey D, Madai VI. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak. 2020; 20:310. DOI: 10.1186/s12911-020-01332-6. PMID: 33256715. PMCID: PMC7706019.86. Dwivedi YK, Hughes L, Ismagilova E, Aarts G, Coombs C, Crick T, et al. Artificial intelligence (AI): multidisciplinary perspectives on emerging challenges, opportunities, and agenda for research, practice and policy. Int J Inf Manag. 2021; 57:101994. DOI: 10.1016/j.ijinfomgt.2019.08.002.87. Mauthner NS, Parry O. Open access digital data sharing: principles, policies and practices. Soc Epistemol. 2013; 27(1):47–67. DOI: 10.1080/02691728.2012.760663.88. Knapič S, Malhi A, Saluja R, Främling K. Explainable artificial intelligence for human decision support system in the medical domain. Mach Learn Knowl Extr. 2021; 3(3):740–770. DOI: 10.3390/make3030037.
Article89. Band SS, Yarahmadi A, Hsu CC, Biyari M, Sookhak M, Ameri R, et al. Application of explainable artificial intelligence in medical health: a systematic review of interpretability methods. Inform Med Unlocked. 2023; 40:101286. DOI: 10.1016/j.imu.2023.101286.90. Mensah GB. Artificial intelligence and ethics: a comprehensive review of bias mitigation, transparency, and accountability in AI Systems. ResearchGate. [Preprint]. 2023.91. Khanna S, Srivastava S. Patient-centric ethical frameworks for privacy, transparency, and bias awareness in deep learning-based medical systems. Appl Res Artif Intell Cloud Comput. 2020; 3(1):16–35.92. Vaassen F, Hazelaar C, Vaniqui A, Gooding M, van der Heyden B, Canters R, et al. Evaluation of measures for assessing time-saving of automatic organ-at-risk segmentation in radiotherapy. Phys Imaging Radiat Oncol. 2020; 13:1–6. DOI: 10.1016/j.phro.2019.12.001. PMID: 33458300. PMCID: PMC7807544.
Article93. Habuza T, Navaz AN, Hashim F, Alnajjar F, Zaki N, Serhani MA, et al. AI applications in robotics, diagnostic image analysis and precision medicine: current limitations, future trends, guidelines on CAD systems for medicine. Inform Med Unlocked. 2021; 24:100596. DOI: 10.1016/j.imu.2021.100596.94. Bates DW, Saria S, Ohno-Machado L, Shah A, Escobar G. Big data in health care: using analytics to identify and manage high-risk and high-cost patients. Health Aff. 2014; 33(7):1123–1131. DOI: 10.1377/hlthaff.2014.0041. PMID: 25006137.
Article95. Shah V. AI in mental health: predictive analytics and intervention strategies. J Environ Sci Technol. 2022; 1(2):55–74.96. Kim N, Chun J, Chang JS, Lee CG, Keum KC, Kim JS. Feasibility of continual deep learning-based segmentation for personalized adaptive radiation therapy in head and neck area. Cancers. 2021; 13(4):702. DOI: 10.3390/cancers13040702. PMID: 33572310. PMCID: PMC7915955.
Article97. van Leeuwen KG, de Rooij M, Schalekamp S, van Ginneken B, Rutten MJCM. How does artificial intelligence in radiology improve efficiency and health outcomes? Pediatr Radiol. 2022; 52:2087–2093. DOI: 10.1007/s00247-021-05114-8. PMID: 34117522. PMCID: PMC9537124.
Article98. Brock KK. Adaptive radiotherapy: moving into the future. Semin Radiat Oncol. 2019; 29(3):181–184. DOI: 10.1016/j.semradonc.2019.02.011. PMID: 31027635. PMCID: PMC7219982.
Article99. Kalweit G, Valiña LG, Mastroleo I, Klett A, Boedecker J, Mertelsmann R, et al. AI as an always-available oncologist: a vision for AI-optimized cancer therapy based on real-time adaptive dosing at the patient level. J Sci Humanit Arts. 2024; 11(1):1–12. DOI: 10.17160/josha.11.1.975.100. Ahmed A, Aziz S, Abd-alrazaq A, Farooq F, Sheikh J. Overview of artificial intelligence–driven wearable devices for diabetes: scoping review. J Med Internet Res. 2022; 24(8):e36010. DOI: 10.2196/36010. PMID: 35943772. PMCID: PMC9399882.101. Johnson KB, Wei-Qi W, Weeraratne D, Frisse ME, Misulis K, Rhee K, et al. Precision medicine, AI, and the future of personalized health care. Clin Transl Sci. 2021; 14(1):86–93. DOI: 10.1111/cts.12884. PMID: 32961010. PMCID: PMC7877825.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Future Perspectives of Artificial Intelligence in Mental Health Care: Challenges and Opportunities
- Advances and utility of digital twins in critical care and acute care medicine: a narrative review
- Concepts, Characteristics, and Clinical Validation of IBM Watson for Oncology
- Clinical Application of Artificial Intelligence in Digital Breast Tomosynthesis
- Artificial Intelligence for Autonomous Robotic Surgery in Urology: A Narrative Review