J Korean Med Sci.
2024 Oct;39(41):e265. 10.3346/jkms.2024.39.e265.
Association of Preoperative Opioid and Glucocorticoid Use With Mortality and Complication After Total Knee or Hip Arthroplasty
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, College of Medicine, Seoul National University, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2560595
- DOI: http://doi.org/10.3346/jkms.2024.39.e265
Abstract
- Background
The association between preoperative opioid or glucocorticoid (GC) use and clinical outcomes, such as postoperative mortality after total joint arthroplasty (TJA), is unclear.
Methods
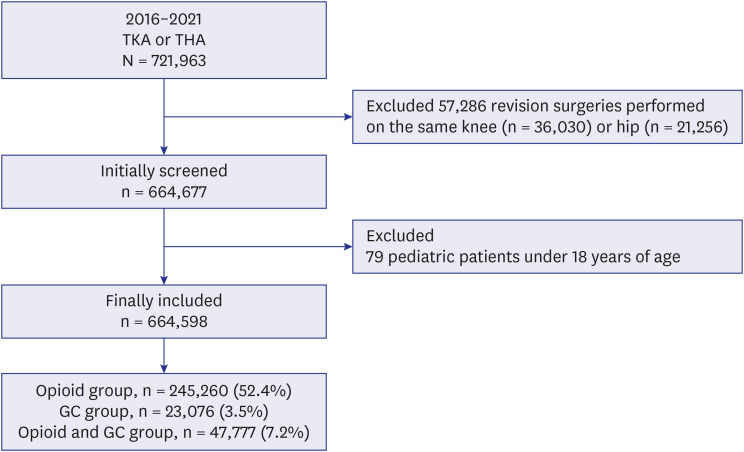
A population-based retrospective cohort study was conducted. Data were obtained from the National Health Insurance Service of South Korea. Patients who underwent TJA (total knee or total hip arthroplasty) between January 1, 2016, and December 31, 2021, were included. We examined whether the patients had been prescribed opioids or oral GC for > 90 days prior to TJA.
Results
In total, 664,598 patients who underwent TJA were included, among whom 245,260 (52.4%), 23,076 (3.5%), and 47,777 (7.2%) were classified into the opioid, GC, and opioid and GC groups, respectively. Compared to the non-user group, the opioid and GC user groups showed 53% (odds ratio [OR], 1.53; 95% confidence interval [CI], 1.12–2.30; P = 0.010) higher odds of in-hospital mortality. Compared to non-users, GC users (hazard ratio [HR], 1.24; 95% CI, 1.15–1.34; P < 0.001) and opioid and GC users (HR, 1.24; 95% CI, 1.14–1.35; P < 0.001) showed a higher risk of 1-year all-cause mortality. Compared to the non-user group, GC users (OR, 1.09; 95% CI, 1.04–1.15; P < 0.001) and opioid and GC users (OR, 1.06; 95% CI, 1.01–1.11; P = 0.014) showed higher odds of postoperative complications.
Conclusion
Preoperative GC use and concomitant use of opioid analgesics with GC were associated with increased postoperative mortality and morbidity after TJA. However, preoperative chronic opioid analgesic use alone did not affect postoperative mortality or morbidity.
Keyword
Figure
Reference
-
1. Madry H. Surgical therapy in osteoarthritis. Osteoarthritis Cartilage. 2022; 30(8):1019–1034. PMID: 35183776.2. Choi HJ, Yoon HK, Oh HC, Yoo JH, Choi CH, Lee JH, et al. Incidence and risk factors analysis for mortality after total knee arthroplasty based on a large national database in Korea. Sci Rep. 2021; 11(1):15772. PMID: 34349179.3. Wood AM, Brock TM, Heil K, Holmes R, Weusten A. A review on the management of hip and knee osteoarthritis. Int J Chronic Dis. 2013; 2013:845015. PMID: 26464847.4. Pugely AJ, Martin CT, Gao Y, Belatti DA, Callaghan JJ. Comorbidities in patients undergoing total knee arthroplasty: do they influence hospital costs and length of stay? Clin Orthop Relat Res. 2014; 472(12):3943–3950. PMID: 25190193.5. Kim SJ, Sung IH, Song SY, Jo YH. The epidemiology and trends of primary total ankle arthroplasty and revision procedure in Korea between 2007 and 2017. J Korean Med Sci. 2020; 35(22):e169. PMID: 32508066.6. Park JW, Won SH, Moon SY, Lee YK, Ha YC, Koo KH. Burden and future projection of revision total hip arthroplasty in South Korea. BMC Musculoskelet Disord. 2021; 22(1):375. PMID: 33888097.7. Halawi MJ, Vovos TJ, Green CL, Wellman SS, Attarian DE, Bolognesi MP. Preoperative pain level and patient expectation predict hospital length of stay after total hip arthroplasty. J Arthroplasty. 2015; 30(4):555–558. PMID: 25433645.8. Nguyen UD, Ayers DC, Li W, Harrold LR, Franklin PD. Preoperative pain and function: profiles of patients selected for total knee arthroplasty. J Arthroplasty. 2016; 31(11):2402–2407.e2. PMID: 27259392.9. Gibofsky A, Barkin RL. Chronic pain of osteoarthritis: considerations for selecting an extended-release opioid analgesic. Am J Ther. 2008; 15(3):241–255. PMID: 18496262.10. Conaghan PG, Cook AD, Hamilton JA, Tak PP. Therapeutic options for targeting inflammatory osteoarthritis pain. Nat Rev Rheumatol. 2019; 15(6):355–363. PMID: 31068673.11. Klein NC, Go CH, Cunha BA. Infections associated with steroid use. Infect Dis Clin North Am. 2001; 15(2):423–432. PMID: 11447704.12. Roy S, Loh HH. Effects of opioids on the immune system. Neurochem Res. 1996; 21(11):1375–1386. PMID: 8947928.13. Oh TK, Kim S, Song IA, Jeon YT. Pre-operative chronic opioid or glucocorticoid use and mortality after noncardiac surgery: a retrospective cohort study. Eur J Anaesthesiol. 2020; 37(10):926–933. PMID: 32371829.14. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.15. Cho SK, Choi S, Kim H, Song YJ, Jung SY, Jang EJ, et al. COX-2 inhibitor use as an early treatment option for knee osteoarthritis patients in Korea: a population-based cross-sectional study. J Korean Med Sci. 2022; 37(18):e148. PMID: 35535375.16. Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015; 350:h1225. PMID: 25828856.17. Seo KH. Perioperative glucocorticoid management based on current evidence. Anesth Pain Med. 2021; 16(1):8–15.18. Savvidou O, Milonaki M, Goumenos S, Flevas D, Papagelopoulos P, Moutsatsou P. Glucocorticoid signaling and osteoarthritis. Mol Cell Endocrinol. 2019; 480:153–166. PMID: 30445185.19. Hung YT, Hung WK, Chi CC. Effects of preoperative chronic steroid use on postoperative outcomes in orthopedic surgery: a systematic review and meta-analysis. Pharmaceuticals (Basel). 2023; 16(9):1328. PMID: 37765136.20. Costantini D, Marasco V, Møller AP. A meta-analysis of glucocorticoids as modulators of oxidative stress in vertebrates. J Comp Physiol B. 2011; 181(4):447–456. PMID: 21416253.21. Toro-Pérez J, Rodrigo R. Contribution of oxidative stress in the mechanisms of postoperative complications and multiple organ dysfunction syndrome. Redox Rep. 2021; 26(1):35–44. PMID: 33622196.22. Ayala JC, Grismaldo A, Sequeda-Castañeda LG, Aristizábal-Pachón AF, Morales L. Oxidative stress in ICU patients: ROS as mortality long-term predictor. Antioxidants. 2021; 10(12):1912. PMID: 34943015.23. Kücükakin B, Gögenur I, Reiter RJ, Rosenberg J. Oxidative stress in relation to surgery: is there a role for the antioxidant melatonin? J Surg Res. 2009; 152(2):338–347. PMID: 18262562.24. Oray M, Abu Samra K, Ebrahimiadib N, Meese H, Foster CS. Long-term side effects of glucocorticoids. Expert Opin Drug Saf. 2016; 15(4):457–465. PMID: 26789102.25. O’Brien WJ, Gupta K, Itani KM. Association of postoperative infection with risk of long-term infection and mortality. JAMA Surg. 2020; 155(1):61–68. PMID: 31693076.26. Shahi A, Tan TL, Chen AF, Maltenfort MG, Parvizi J. In-hospital mortality in patients with periprosthetic joint infection. J Arthroplasty. 2017; 32(3):948–952.e1. PMID: 27816369.27. Muffly BT, Ayeni AM, Jones CA, Heo KY, Guild GN, Premkumar A. Periprosthetic joint infection risk after primary total knee arthroplasty: Are all preoperative corticosteroid injections the same? J Arthroplasty. 2024; 39(5):1312–1316.e7. PMID: 37924991.28. Kittle H, Ormseth A, Patetta MJ, Sood A, Gonzalez MH. Chronic corticosteroid use as a risk factor for perioperative complications in patients undergoing total joint arthroplasty. J Am Acad Orthop Surg Glob Res Rev. 2020; 4(7):e2000001. PMID: 32672719.29. Quinlan J, Levy N, Lobo DN, Macintyre PE. Preoperative opioid use: a modifiable risk factor for poor postoperative outcomes. Br J Anaesth. 2021; 127(3):327–331. PMID: 34090682.30. Oh TK, Song IA. Opioid prescription and long-term survival outcomes in adults: a nationwide cohort study in Korea. J Korean Med Sci. 2024; 39(9):e82. PMID: 38469961.31. Cha Y, Jang SY, Yoo JI, Choi HG, Hwang JW, Choy W. Effect of opioids on all-cause mortality and opioid addiction in total hip arthroplasty: a Korea nationwide cohort study. J Korean Med Sci. 2021; 36(13):e87. PMID: 33821594.32. Page GG, Ben-Eliyahu S. The immune-suppressive nature of pain. Semin Oncol Nurs. 1997; 13(1):10–15. PMID: 9048431.33. Totsch SK, Sorge RE. Immune system involvement in specific pain conditions. Mol Pain. 2017; 13:1744806917724559. PMID: 28741433.34. Madsen HJ, Henderson WG, Bronsert MR, Dyas AR, Colborn KL, Lambert-Kerzner A, et al. Associations between preoperative risk, postoperative complications, and 30-day mortality. World J Surg. 2022; 46(10):2365–2376. PMID: 35778512.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repeated Periprosthethic Femoral Fracture in a Below Knee Amputee with Ipsilateral Cementless Total Hip Arthroplasty: A Case Report
- Geometric Total Knee Arthroplasty: A Case Report
- Total Hip Arthroplasty for Ankylosed Hip
- Three Concurrent Periprosthetic Joint Infections: A Case Report and Literature Review
- Popliteal Artery Occlusion after Total Knee Arthroplasty: A Case Report