Healthc Inform Res.
2024 Oct;30(4):312-323. 10.4258/hir.2024.30.4.312.
Development and Usability Evaluation of COVID-Iran: A Mobile Application for Mitigating COVID-19 Misinformation
- Affiliations
-
- 1Poostchi Ophthalmology Research Center, Department of Ophthalmology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
- 2Faculty of Management and Medical Information Sciences, Kerman University of Medical Sciences, Kerman, Iran
- 3Business School, University of Queensland, Brisbane, Australia
- 4Department of Health Information Technology, School of Allied of Medical Sciences, Mazandaran University of Medical Sciences, Sari, Iran
- KMID: 2560534
- DOI: http://doi.org/10.4258/hir.2024.30.4.312
Abstract
Objectives
The spread of misinformation through the internet can lead to dangerous behavioral changes and erode trust in reliable sources, especially during public health crises like coronavirus disease 2019 (COVID-19). To combat this issue, innovative strategies that leverage information technology are essential. This study focused on developing and evaluating a mobile application (app), COVID-Iran, aimed at countering COVID-19 misinformation by delivering accurate, reliable, and credible information.
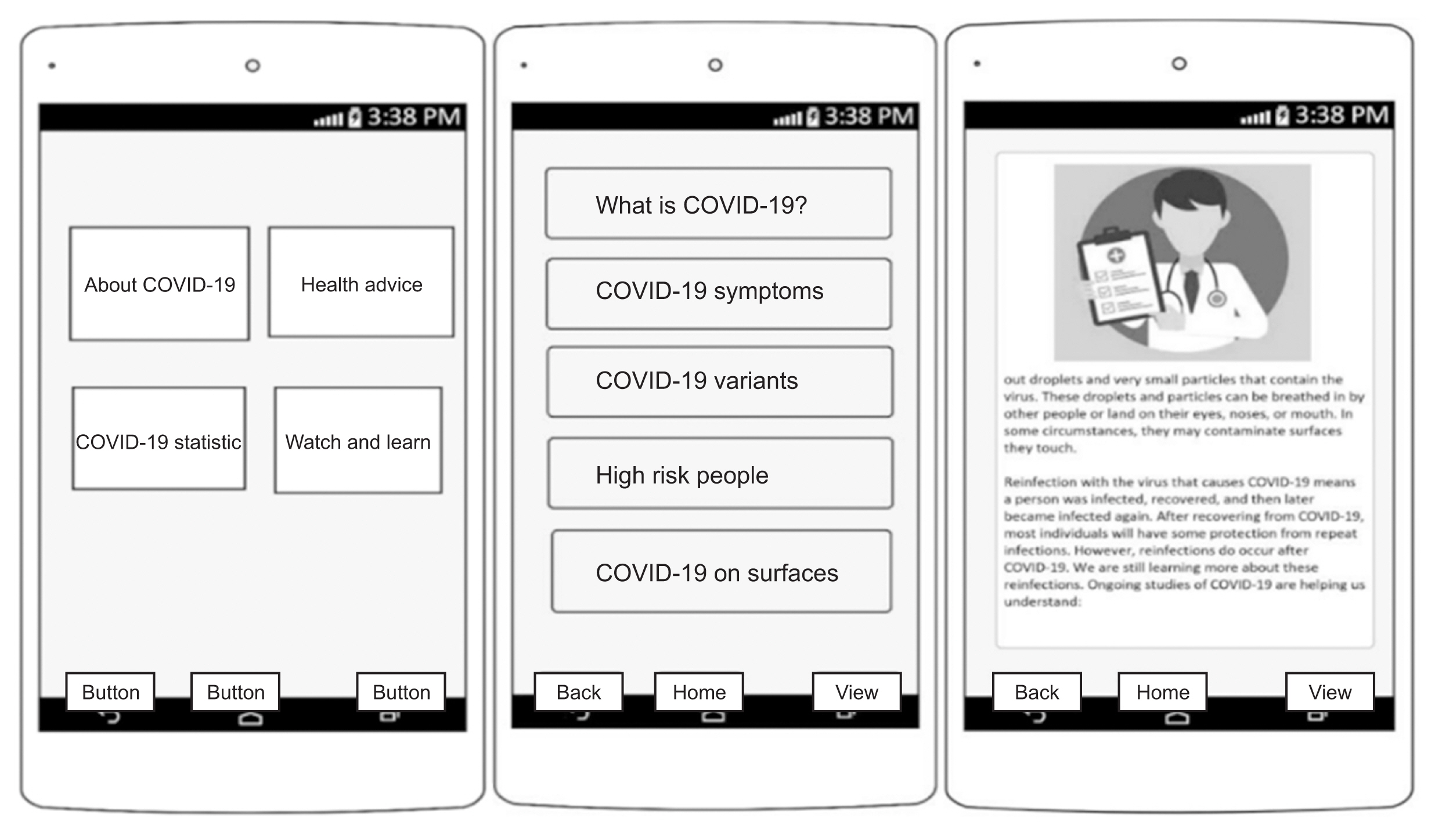
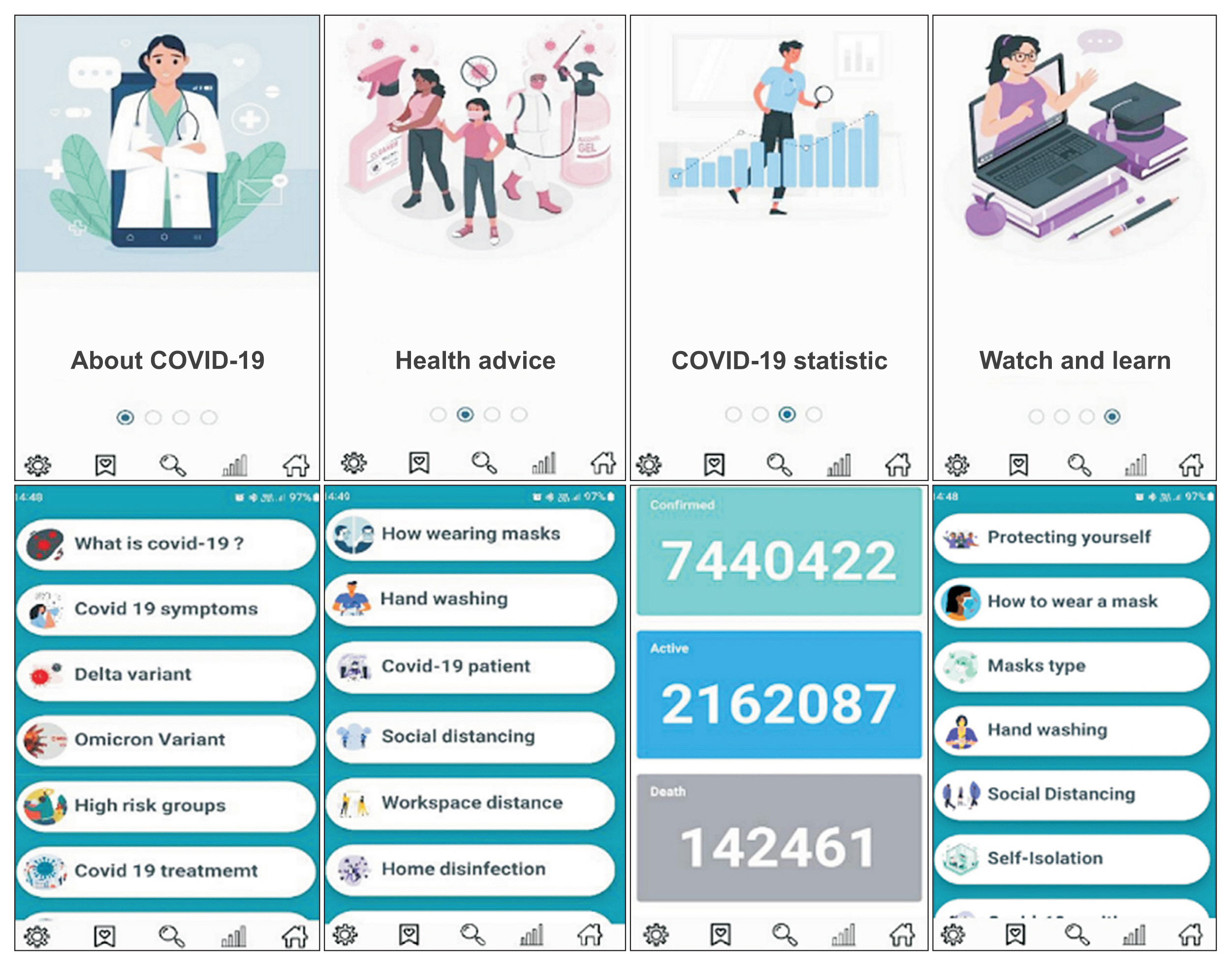
Methods
The development of the app involved a multi-step, user-centered approach that integrated qualitative expert consultations with quantitative survey research to pinpoint and validate key features. The app was initially prototyped using Enterprise Architect software and subsequently developed using Android Studio and MySQL. We conducted a usability evaluation using the System Usability Scale (SUS), where participants engaged in various tasks related to information seeking, self-assessment, and health management. Data were analyzed using descriptive statistics in SPSS version 19.
Results
The findings revealed a high usability level (SUS score of 81.35), with participants reporting ease of use and learnability. The app effectively countered misinformation by providing access to trusted sources and evidence-based counterarguments. User feedback emphasized the app’s strengths in clarity, accuracy, trustworthiness, and its comprehensive approach. Plans for future improvements include the integration of artificial intelligence to deliver personalized content.
Conclusions
Despite limitations such as the small sample size and potential self-selection bias, this study highlights the significant potential of mHealth apps to provide reliable health information and combat misinformation.
Figure
Reference
-
References
1. Risoldi Cochrane Z, Gregory P, Wilson A. Readability of consumer health information on the internet: a comparison of U.S. government-funded and commercially funded websites. J Health Commun. 2012; 17(9):1003–10. https://doi.org/10.1080/10810730.2011.650823.
Article2. Suarez-Lledo V, Alvarez-Galvez J. Prevalence of health misinformation on social media: systematic review. J Med Internet Res. 2021; 23(1):e17187. https://doi.org/10.2196/17187.
Article3. Zhao Y, Zhu S, Wan Q, Li T, Zou C, Wang H, et al. Understanding how and by whom COVID-19 misinformation is spread on social media: coding and network analyses. J Med Internet Res. 2022; 24(6):e37623. https://doi.org/10.2196/37623.
Article4. Lee JJ, Kang KA, Wang MP, Zhao SZ, Wong JY, O’Connor S, et al. Associations between COVID-19 misinformation exposure and belief with COVID-19 knowledge and preventive behaviors: cross-sectional online study. J Med Internet Res. 2020; 22(11):e22205. https://doi.org/10.2196/22205.
Article5. Pickles K, Cvejic E, Nickel B, Copp T, Bonner C, Leask J, et al. COVID-19 misinformation trends in Australia: prospective longitudinal national survey. J Med Internet Res. 2021; 23(1):e23805. https://doi.org/10.2196/23805.
Article6. Nsoesie EO, Cesare N, Muller M, Ozonoff A. COVID-19 misinformation spread in eight countries: exponential growth modeling study. J Med Internet Res. 2020; 22(12):e24425. https://doi.org/10.2196/24425.
Article7. Ekong I, Chukwu E, Chukwu M. COVID-19 mobile positioning data contact tracing and patient privacy regulations: exploratory search of global response strategies and the use of digital tools in Nigeria. JMIR Mhealth Uhealth. 2020; 8(4):e19139. https://doi.org/10.2196/19139.
Article8. Alwashmi MF. The use of digital health in the detection and management of COVID-19. Int J Environ Res Public Health. 2020; 17(8):2906. https://doi.org/10.3390/ijerph17082906.
Article9. Camacho-Rivera M, Islam JY, Rivera A, Vidot DC. Attitudes toward using COVID-19 mHealth tools among adults with chronic health conditions: secondary data analysis of the COVID-19 impact survey. JMIR Mhealth Uhealth. 2020; 8(12):e24693. https://doi.org/10.2196/24693.
Article10. Kanera IM, Willems RA, Bolman CA, Mesters I, Zambon V, Gijsen BC, et al. Use and appreciation of a tailored self-management eHealth intervention for early cancer survivors: process evaluation of a randomized controlled trial. J Med Internet Res. 2016; 18(8):e229. https://doi.org/10.2196/jmir.5975.
Article11. Nightingale R, Hall A, Gelder C, Friedl S, Brennan E, Swallow V. Desirable components for a customized, home-based, digital care-management app for children and young people with long-term, chronic conditions: a qualitative exploration. J Med Internet Res. 2017; 19(7):e235. https://doi.org/10.2196/jmir.7760.
Article12. Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011; 1(1):53–71. https://doi.org/10.1007/s13142-011-0021-7.
Article13. Kondylakis H, Katehakis DG, Kouroubali A, Logothetidis F, Triantafyllidis A, Kalamaras I, et al. COVID-19 mobile apps: a systematic review of the literature. J Med Internet Res. 2020; 22(12):e23170. https://doi.org/10.2196/23170.
Article14. John Leon Singh H, Couch D, Yap K. Mobile health apps that help with COVID-19 management: scoping review. JMIR Nurs. 2020; 3(1):e20596. https://doi.org/10.2196/20596.
Article15. Taghipour F, Ashrafi-Rizi H, Soleymani MR. Dissemination and acceptance of COVID-19 misinformation in iran: a qualitative study. Community Health Equity Res Policy. 2023; 43(3):283–91. https://doi.org/10.1177/0272684X211022155.
Article16. Asadzadeh A, Mohammadzadeh Z, Fathifar Z, Jahangiri- Mirshekarlou S, Rezaei-Hachesu P. A framework for information technology-based management against COVID-19 in Iran. BMC Public Health. 2022; 22(1):402. https://doi.org/10.1186/s12889-022-12781-1.
Article17. Aalaei S, Khoshrounejad F, Saleh LA, Amini M. Design of a mobile application and evaluation of its effects on psychological parameters of covid-19 inpatients: a protocol for a randomized controlled trial. Front Psychiatry. 2021; 12:612384. https://doi.org/10.3389/fpsyt.2021.612384.
Article18. Hajesmaeel-Gohari S, Khordastan F, Fatehi F, Samzadeh H, Bahaadinbeigy K. The most used questionnaires for evaluating satisfaction, usability, acceptance, and quality outcomes of mobile health. BMC Med Inform Decis Mak. 2022; 22(1):22. https://doi.org/10.1186/s12911-022-01764-2.
Article19. Virzi RA. Refining the test phase of usability evaluation: how many subjects is enough? Hum Fact. 1992; 34(4):457–68. https://doi.org/10.1177/001872089203400407.
Article20. Faulkner L. Beyond the five-user assumption: benefits of increased sample sizes in usability testing. Behav Res Methods Instrum Comput. 2003; 35(3):379–83. https://doi.org/10.3758/bf03195514.
Article21. Silva AC, Goes FG, Avila FM, Goulart MC, Pinto LF, Stipp MA. Construction and validation of a mobile application for health education about COVID-19. Rev Gaucha Enferm. 2022; 43:e20210289. https://doi.org/10.1590/1983-1447.2022.20210289.en.
Article22. Kodali PB, Hense S, Kopparty S, Kalapala GR, Haloi B. How Indians responded to the Arogya Setu app? Indian J Public Health. 2020; 64(Supplement):S228–30. https://doi.org/10.4103/ijph.IJPH_499_20.
Article23. Hussain M, Al-Haiqi A, Zaidan AA, Zaidan BB, Kiah ML, Anuar NB, et al. The landscape of research on smartphone medical apps: coherent taxonomy, motivations, open challenges and recommendations. Comput Methods Programs Biomed. 2015; 122(3):393–408. https://doi.org/10.1016/j.cmpb.2015.08.015.
Article24. Salehinejad S, Niakan Kalhori SR, Hajesmaeel Gohari S, Bahaadinbeigy K, Fatehi F. A review and content analysis of national apps for COVID-19 management using Mobile Application Rating Scale (MARS). Inform Health Soc Care. 2021; 46(1):42–55. https://doi.org/10.1080/17538157.2020.1837838.
Article25. Mohammad H, Elham M, Mehraeen E, Aghamohammadi V, Seyedalinaghi S, Kalantari S, et al. Identifying data elements and key features of a mobile-based self-care application for patients with COVID-19 in Iran. Health Informatics J. 2021; 27(4):14604582211065703. https://doi.org/10.1177/14604582211065703.
Article26. Saeidnia H, Mohammadzadeh Z, Saeidnia M, Mahmoodzadeh A, Ghorbani N, Hasanzadeh M. Identifying Requirements of a Self-care System on smartphones for preventing coronavirus disease 2019 (COVID-19). Iran J Med Microbiol. 2020; 14(3):241–51. https://doi.org/10.30699/ijmm.14.3.241.
Article27. Nouri R, Salari R, Kalhori SR, Ayyoubzadeh SM, Gholamzadeh M. Persian mobile health applications for COVID- 19: a use case-based study. J Educ Health Promot. 2022; 11:100. https://doi.org/10.4103/jehp.jehp_759_21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19 and abortion right
- Occurrence of erythema multiforme following COVID-19 vaccination: a review
- Exploring the experience of developing COVID-19 vaccines in Iran
- Mesenchymal Stem Cell-Derived Exosomes for COVID-19 Therapy, Preclinical and Clinical Evidence
- Immune Response to COVID-19 Vaccination in Hematologic Malignancies: A Mini-Review