J Yeungnam Med Sci.
2024 Oct;41(4):235-251. 10.12701/jyms.2024.00521.
Postoperative conditions of rehabilitative interest in lung transplantation: a systematic review
- Affiliations
-
- 1Department of Continuity of Care and Integration, Physical Medicine and Rehabilitation, IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy
- 2Department of Physical Therapy and Rehabilitation, University of Health Sciences Turkey, Hamidiye Faculty of Health Sciences, Istanbul, Turkey
- 3Department of Pulmonary and Critical Care Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
- 4Department of Rehabilitation, Royal Papworth Hospital NHS Foundation Trust, Cambridge, UK
- KMID: 2560484
- DOI: http://doi.org/10.12701/jyms.2024.00521
Abstract
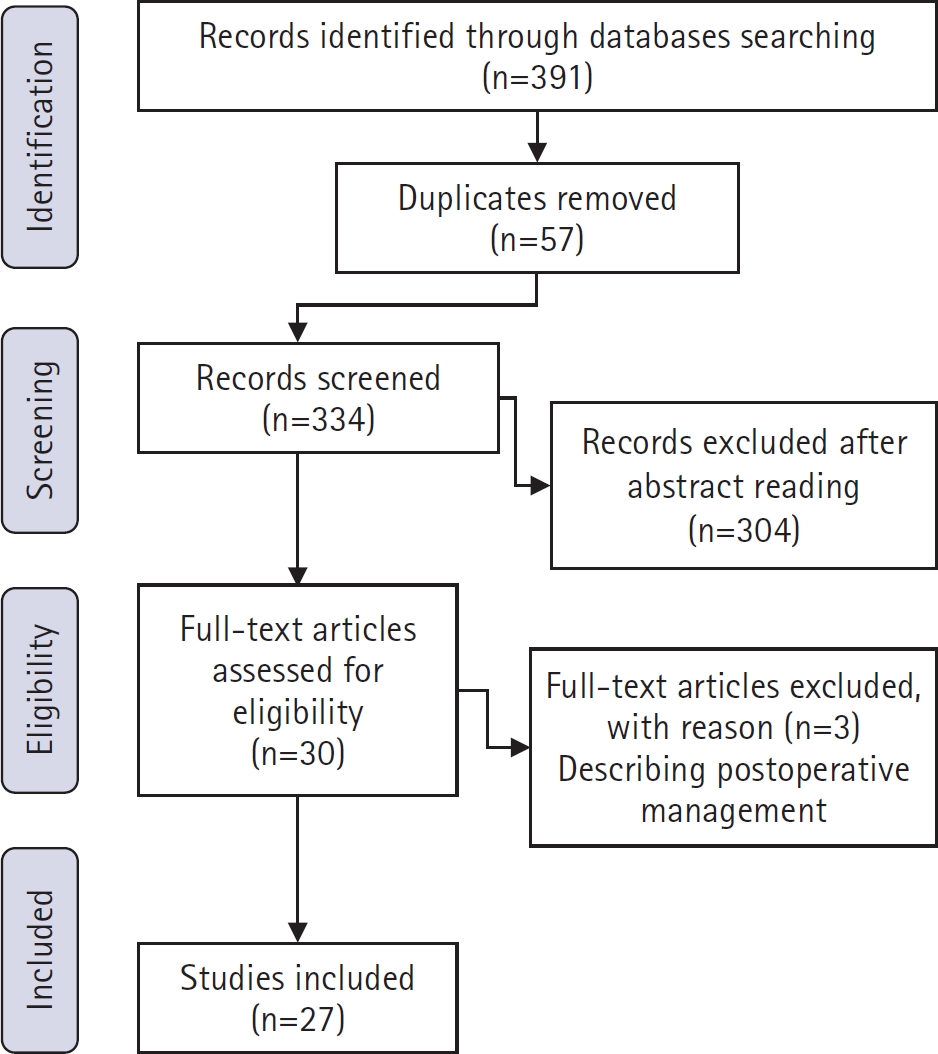
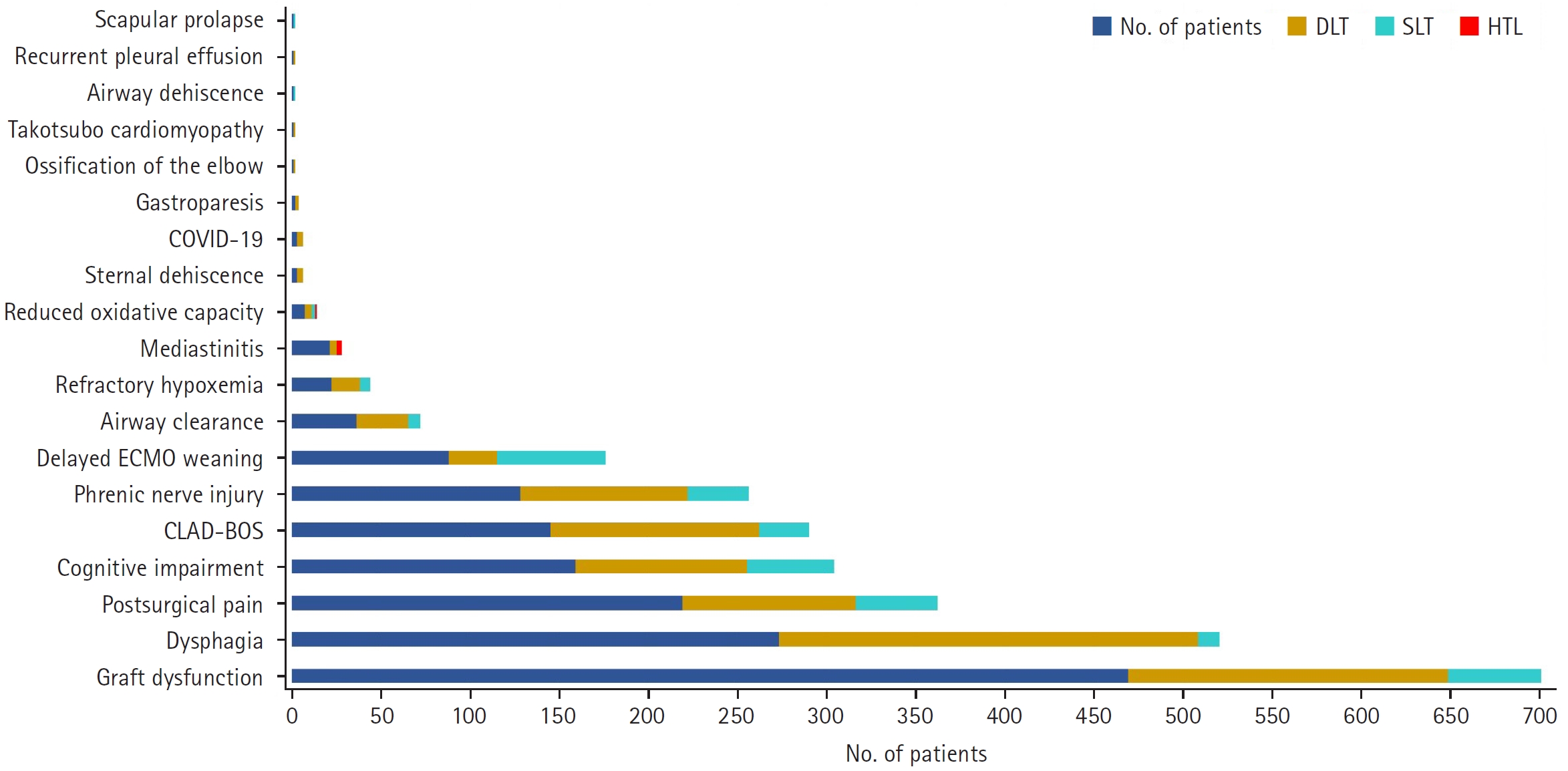
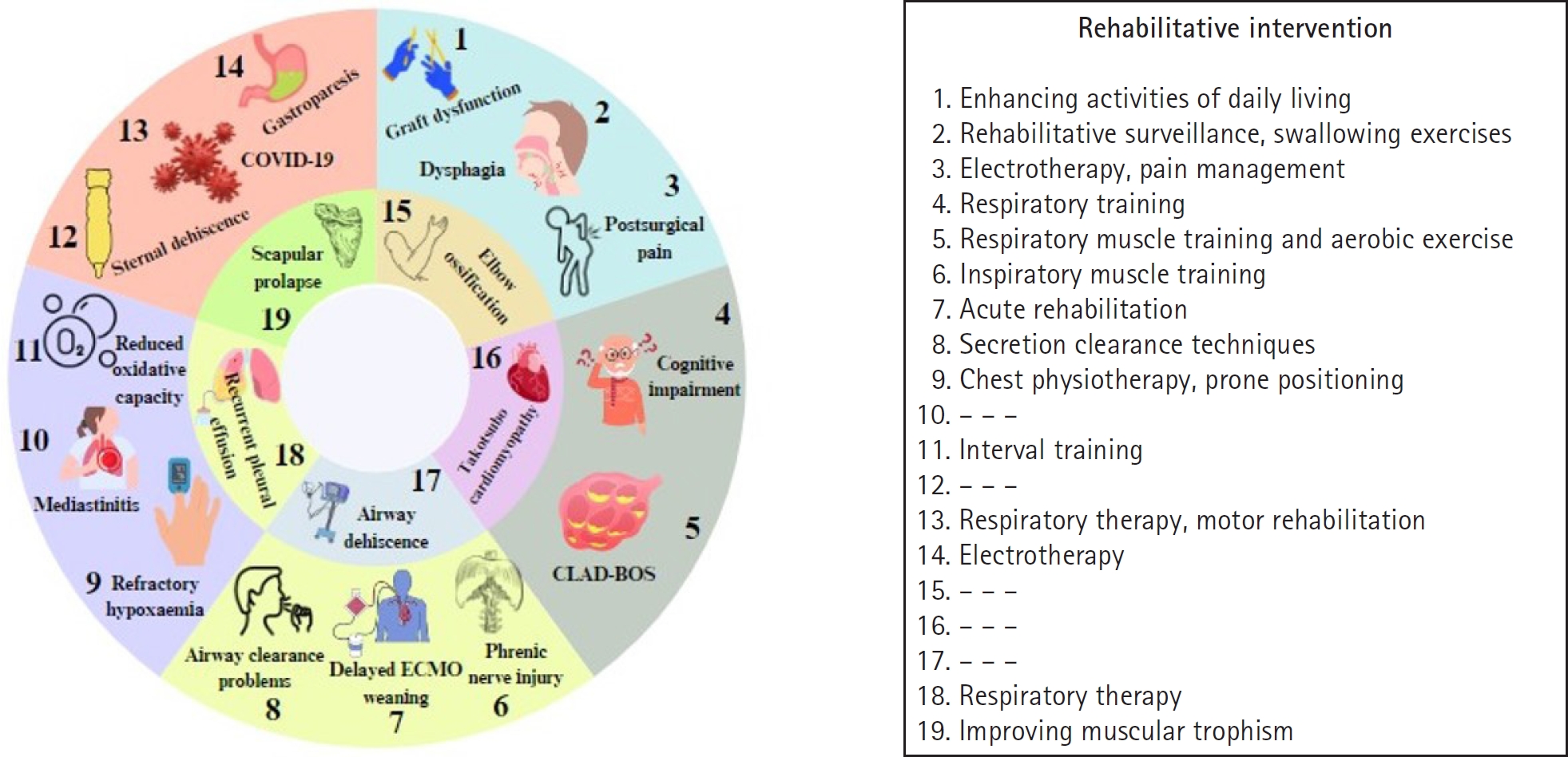
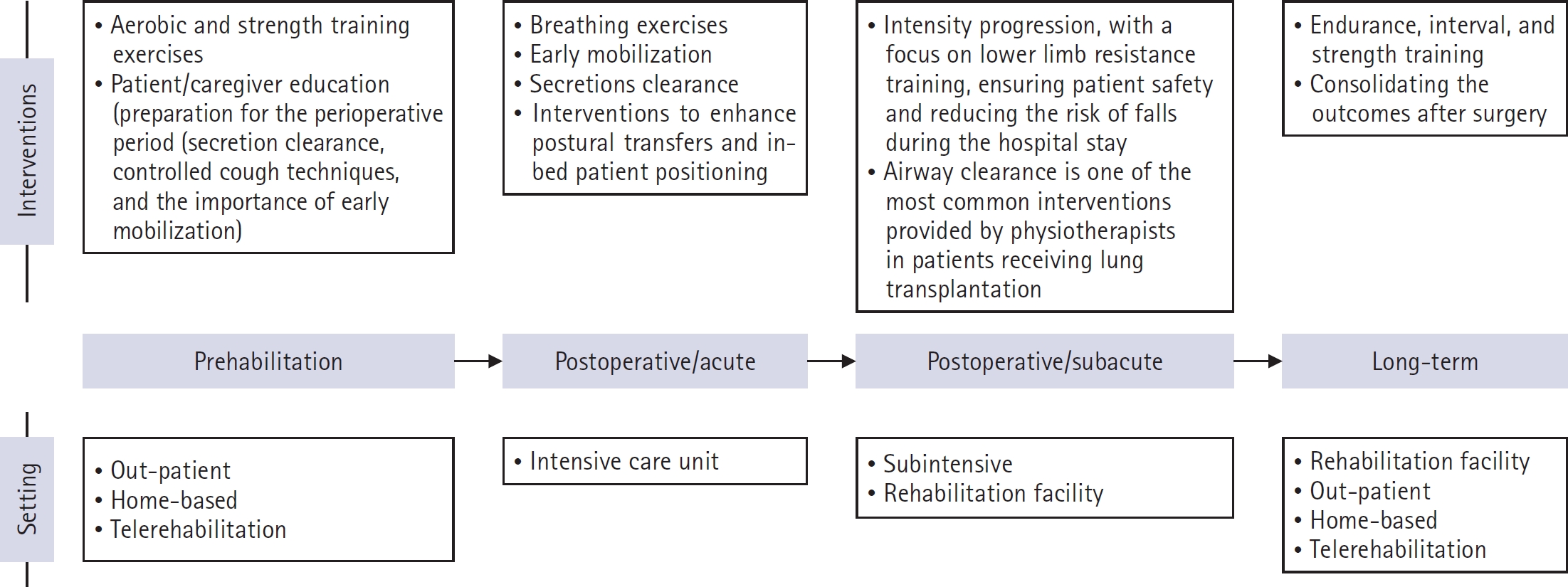
- Lung transplantation is an elective treatment option for end-stage respiratory diseases in which all medical therapy options have been exhausted. The current study aimed to identify updated information on the postoperative conditions that may impair rehabilitation after lung transplantation and to provide specific considerations of their clinical relevance during the recovery process. The present study is a systematic review conducted by searching three primary databases: the United States National Library of Medicine PubMed system, Scopus, and the Cochrane Library. The databases were searched for articles published from database inception until May 2024; at the end of the selection process, 27 documents were included in the final analysis. The retrieved material identified 19 conditions of rehabilitative interest that potentially affect the postoperative course: graft dysfunction, dysphagia, postsurgical pain, cognitive impairment, chronic lung allograft dysfunction-bronchiolitis obliterans syndrome, phrenic nerve injury, delayed extracorporeal membrane oxygenation weaning, airway clearance, refractory hypoxemia, mediastinitis, reduced oxidative capacity, sternal dehiscence, coronavirus disease 2019 (COVID-19), gastroparesis, ossification of the elbow, Takotsubo cardiomyopathy, airway dehiscence, recurrent pleural effusion, and scapular prolapse. Although some patients are not amenable to rehabilitation techniques, others can significantly improve with rehabilitation.
Keyword
Figure
Reference
-
References
1. Egan TM, Westerman JH, Lambert CJ, Detterbeck FC, Thompson JT, Mill MR, et al. Isolated lung transplantation for end-stage lung disease: a viable therapy. Ann Thorac Surg. 1992; 53:590–6.2. Mendeloff EN. Lung transplantation for cystic fibrosis. Semin Thorac Cardiovasc Surg. 1998; 10:202–12.3. Marulli G, Rea F. Lung transplantation for emphysema. Transplant Proc. 2008; 40:2006–9.4. Adler FR, Aurora P, Barker DH, Barr ML, Blackwell LS, Bosma OH, et al. Lung transplantation for cystic fibrosis. Proc Am Thorac Soc. 2009; 6:619–33.5. Pirson J, Duysinx B, Nguyen D, Corhay JL, Louis R. Lung transplantation benefits for terminal lung diseases. Rev Med Liege. 2011; 66:434–9.6. Kropski JA, Blackwell TS. Progress in understanding and treating idiopathic pulmonary fibrosis. Annu Rev Med. 2019; 70:211–24.7. Greer M, Welte T. Chronic obstructive pulmonary disease and lung transplantation. Semin Respir Crit Care Med. 2020; 41:862–73.8. Cheronis N, Rabold E, Singh A, Cheema T. Lung transplantation in COPD. Crit Care Nurs Q. 2021; 44:61–73.9. Kapnadak SG, Raghu G. Lung transplantation for interstitial lung disease. Eur Respir Rev. 2021; 30:210017.10. Neto DM, Chan EG, Sanchez PG. Double lung transplantation in patients with lung atelectasis and complete mediastinal shift. Clin Case Rep. 2022; 10:e05515.11. Leong SW, Bos S, Lordan JL, Nair A, Fisher AJ, Meachery G. Lung transplantation for interstitial lung disease: evolution over three decades. BMJ Open Respir Res. 2023; 10:e001387.12. Marro M, Leiva-Juárez MM, D'Ovidio F, Chan J, Van Raemdonck D, Ceulemans LJ, et al. Lung transplantation for primary ciliary dyskinesia and kartagener syndrome: a multicenter study. Transpl Int. 2023; 36:10819.13. Renaud-Picard B, Tissot A, Burgel PR, Grenet D, de Miranda S, Coiffard B. Lung transplantation for cystic fibrosis and bronchiectasis. Rev Mal Respir. 2023; 40(Suppl 1):e33–41.14. Strykowski R, Adegunsoye A. Idiopathic pulmonary fibrosis and progressive pulmonary fibrosis. Immunol Allergy Clin North Am. 2023; 43:209–28.15. Tasoudis P, Lobo LJ, Coakley RD, Agala CB, Egan TM, Haithcock BE, et al. Outcomes following lung transplant for COVID-19-related complications in the US. JAMA Surg. 2023; 158:1159–66.16. Verleden GM, Gottlieb J. Lung transplantation for COPD/pulmonary emphysema. Eur Respir Rev. 2023; 32:220116.17. Catelli C, Faccioli E, Silvestrin S, Lorenzoni G, Luzzi L, Bennett D, et al. Lung transplantation in patients with previous or unknown oncological disease: evaluation of short- and long-term outcomes. Cancers (Basel). 2024; 16:538.18. Fang YC, Cheng WH, Lu HI, Wang YS, Chuang KH, Lai HH, et al. Double lung transplantation is better than single lung transplantation for end-stage chronic obstructive pulmonary disease: a meta-analysis. J Cardiothorac Surg. 2024; 19:162.19. Cottini SR, Wenger U, Sailer S, Stehberger PA, Schuepbach RA, Hasenclever P, et al. Extracorporeal membrane oxygenation: beneficial strategy for lung transplant recipients. J Extra Corpor Technol. 2013; 45:16–20.20. Hayanga JW, Hayanga HK, Holmes SD, Ren Y, Shigemura N, Badhwar V, et al. Mechanical ventilation and extracorporeal membrane oxygenation as a bridge to lung transplantation: closing the gap. J Heart Lung Transplant. 2019; 38:1104–11.21. Swol J, Shigemura N, Ichiba S, Steinseifer U, Anraku M, Lorusso R. Artificial lungs: where are we going with the lung replacement therapy? Artif Organs. 2020; 44:1135–49.22. Hoopes C, Diaz Guzman Zavala E. Pulmonary transplant after more than 1 year of continuous ambulatory extracorporeal support. ASAIO J. 2022; 68:e172.23. Patterson CM, Shah A, Rabin J, DiChiacchio L, Cypel M, Hoetzenecker K, et al. Extracorporeal life support as a bridge to lung transplantation: where are we now? J Heart Lung Transplant. 2022; 41:1547–55.24. Cha S, Kim BS, Ha JS, Bush EL. How to do it: a safe bedside protocol for dual-lumen right internal jugular cannulation for venovenous extracorporeal membrane oxygenation in COVID-19 patients with severe acute respiratory distress syndrome. ASAIO J. 2023; 69:31–5.25. Bermudez CA, Crespo MM. The case for prolonged ECMO for COVID-19 ARDS as a bridge to recovery or lung transplantation. Transplantation. 2022; 106:e198–9.26. Bennett D, DE Vita E, Fossi A, Bargagli E, Paladini P, Luzzi L, et al. Outcome of ECMO bridge to lung transplantation: a single cohort study. Minerva Med. 2024; 115:116–8.27. Shou BL, Kalra A, Zhou AL, Barbur I, McGoldrick MT, Larson E, et al. Impact of extracorporeal membrane oxygenation bridging duration on lung transplant outcomes. Ann Thorac Surg. 2024; 118:496–503.28. Annema C, De Smet S, Castle EM, Overloop Y, Klaase JM, Janaudis-Ferreira T, et al. European Society of Organ Transplantation (ESOT) consensus statement on prehabilitation for solid organ transplantation candidates. Transpl Int. 2023; 36:11564.29. Quint EE, Ferreira M, van Munster BC, Nieuwenhuijs-Moeke G, Te Velde-Keyzer C, Bakker SJ, et al. Prehabilitation in adult solid organ transplant candidates. Curr Transplant Rep. 2023; 10:70–82.30. Wickerson L, Grewal R, Singer LG, Chaparro C. Experiences and perceptions of receiving and prescribing rehabilitation in adults with cystic fibrosis undergoing lung transplantation. Chron Respir Dis. 2023; 20:14799731221139293.31. Cullum P. Lung transplantation at King's College Hospital. Physiotherapy. 1972; 58:100–2.32. Craven JL, Bright J, Dear CL. Psychiatric, psychosocial, and rehabilitative aspects of lung transplantation. Clin Chest Med. 1990; 11:247–57.33. Downs AM. Physical therapy in lung transplantation. Phys Ther. 1996; 76:626–42.34. Palmer SM, Tapson VF. Pulmonary rehabilitation in the surgical patient. Lung transplantation and lung volume reduction surgery. Respir Care Clin N Am. 1998; 4:71–83.35. Clancy MJ, Adler J, Tevald MA, Zaleski D, Fluehr L, Wamsley C, et al. Rehabilitation characteristics and outcomes for lung transplantation for COVID-19: a case series. Phys Ther. 2023; 103:pzad026.36. Mei J, Hu J, Krause EM, Chen-Yoshikawa TF, Alvarez A, Wang X. The efficacy of pulmonary rehabilitation training program for patients after lung transplantation. J Thorac Dis. 2024; 16:530–41.37. Chhajed PN, Tamm M, Malouf MA, Glanville AR. Lung transplantation: management and complications. Indian J Chest Dis Allied Sci. 2002; 44:31–43.38. Sun H, Deng M, Chen W, Liu M, Dai H, Wang C. Graft dysfunction and rejection of lung transplant, a review on diagnosis and management. Clin Respir J. 2022; 16:5–12.39. Shigemura N, Sclabassi RJ, Bhama JK, Gries CJ, Crespo MM, Johnson B, et al. Early major neurologic complications after lung transplantation: incidence, risk factors, and outcome. Transplantation. 2013; 95:866–71.40. de la Torre M, Fernández R, Fieira E, González D, Delgado M, Méndez L, et al. Postoperative surgical complications after lung transplantation. Rev Port Pneumol (2006). 2015; 21:36–40.41. Machuzak M, Santacruz JF, Gildea T, Murthy SC. Airway complications after lung transplantation. Thorac Surg Clin. 2015; 25:55–75.42. Mahajan AK, Folch E, Khandhar SJ, Channick CL, Santacruz JF, Mehta AC, et al. The diagnosis and management of airway complications following lung transplantation. Chest. 2017; 152:627–38.43. Frye L, Machuzak M. Airway complications after lung transplantation. Clin Chest Med. 2017; 38:693–706.44. Tejwani V, Deshwal H, Ho B, Loss MJ, Avery RK, Mehta AC. Cutaneous complications in recipients of lung transplants: a pictorial review. Chest. 2019; 155:178–93.45. Kovvuru K, Kanduri SR, Vaitla P, Marathi R, Gosi S, Garcia Anton DF, et al. Risk factors and management of osteoporosis post-transplant. Medicina (Kaunas). 2020; 56:302.46. Soetanto V, Grewal US, Mehta AC, Shah P, Varma M, Garg D, et al. Early postoperative complications in lung transplant recipients. Indian J Thorac Cardiovasc Surg. 2022; 38(Suppl 2):260–70.47. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021; 88:105906.48. Yu HC, Kleiman V, Kojic K, Slepian PM, Cortes H, McRae K, et al. Prevention and management of chronic postsurgical pain and persistent opioid use following solid organ transplantation: experiences from the Toronto General Hospital Transitional Pain Service. Transplantation. 2023; 107:1398–405.49. Wildgaard K, Iversen M, Kehlet H. Chronic pain after lung transplantation: a nationwide study. Clin J Pain. 2010; 26:217–22.50. Li LJ, Xu HY, Wang XW, Jin K, Zhang C, Du M, et al. Impact of delayed veno-venous extracorporeal membrane oxygenation weaning on postoperative rehabilitation of lung transplantation: a single-center comparative study. J Artif Organs. 2023; 26:303–8.51. Dallal-York J, Segalewitz T, Croft K, Colsky J, DiBiase L, Anderson A, et al. Incidence, risk factors, and sequelae of dysphagia mediated aspiration following lung transplantation. J Heart Lung Transplant. 2022; 41:1095–103.52. Black RJ, Bogaardt H, McCabe P, Glanville AR, MacDonald P, Madill C. Clinical predictors for oropharyngeal dysphagia and laryngeal dysfunction after lung and heart transplantation. Int J Lang Commun Disord. 2019; 54:894–901.53. Hernández-Hernández MA, Sánchez-Moreno L, Orizaola P, Iturbe D, Álvaréz C, Fernández-Rozas S, et al. A prospective evaluation of phrenic nerve injury after lung transplantation: incidence, risk factors, and analysis of the surgical procedure. J Heart Lung Transplant. 2022; 41:50–60.54. Cohen DG, Christie JD, Anderson BJ, Diamond JM, Judy RP, Shah RJ, et al. Cognitive function, mental health, and health-related quality of life after lung transplantation. Ann Am Thorac Soc. 2014; 11:522–30.55. Tomasi R, Klemm M, Hinske CL, Hulde N, Schramm R, Zwißler B, et al. Impairment of cognitive function in different domains early after lung transplantation. J Clin Psychol Med Settings. 2022; 29:103–12.56. Cao L, Ye S, Chen Y, Pei Y, Chen J, Li X. Longitudinal study on the trajectory and influencing factors of cognitive dysfunction in lung transplantation patients. Transpl Immunol. 2024; 84:102053.57. Armstrong HF, Lederer DJ, Bacchetta M, Bartels MN. Primary graft dysfunction: long-term physical function outcomes among lung transplant recipients. Heart Lung. 2016; 45:544–9.58. Kolaitis NA, Gao Y, Soong A, Greenland JR, Hays SR, Golden J, et al. Primary graft dysfunction attenuates improvements in health-related quality of life after lung transplantation, but not disability or depression. Am J Transplant. 2021; 21:815–24.59. Riera J, Maldonado C, Mazo C, Martínez M, Baldirà J, Lagunes L, et al. Prone positioning as a bridge to recovery from refractory hypoxaemia following lung transplantation. Interact Cardiovasc Thorac Surg. 2017; 25:292–6.60. van Den Berg JW, Geertsma A, van Der Bij W, Koëter GH, de Boer WJ, Postma DS, et al. Bronchiolitis obliterans syndrome after lung transplantation and health-related quality of life. Am J Respir Crit Care Med. 2000; 161:1937–41.61. Vermeulen KM, Groen H, van der Bij W, Erasmus ME, Koëter GH, TenVergert EM. The effect of bronchiolitis obliterans syndrome on health related quality of life. Clin Transplant. 2004; 18:377–83.62. Abid Q, Nkere UU, Hasan A, Gould K, Forty J, Corris P, et al. Mediastinitis in heart and lung transplantation: 15 years experience. Ann Thorac Surg. 2003; 75:1565–71.63. Xu Y, Qing Q, Liang M, Liang W, Lin Z, Wu W, et al. Diaphragm electromyography guidance for a lung transplant recipient with difficult weaning from mechanical ventilation: a case report. Medicine (Baltimore). 2018; 97:e10989.64. Munin MC, Balu G, Sotereanos DG. Elbow complications after organ transplantation. Case reports. Am J Phys Med Rehabil. 1995; 74:67–72.65. Keller BC, Le A, Sobhanie M, Colburn N, Burcham P, Rosenheck J, et al. Early COVID-19 infection after lung transplantation. Am J Transplant. 2020; 20:2923–7.66. Duclos G, Mignon A, Zieleskiewicz L, Kelway C, Forel JM, Thuny F, et al. Takotsubo cardiomyopathy following induction of anesthesia for lung transplantation, an unexpected complication. J Cardiothorac Vasc Anesth. 2018; 32:1855–7.67. Backer E, Dincer EH, Keenan JC, Diaz-Gutierrez I, Cho RJ. Successful treatment of airway dehiscence in a lung transplant patient with radiofrequency ablation. J Bronchology Interv Pulmonol. 2020; 27:e56–9.68. Panchabhai TS, Farver C, Murthy SC, Mehta AC. Recurrent right pleural effusion after double lung transplant. Ann Am Thorac Soc. 2015; 12:1572–4.69. Chansakul T, von Keudell A, Rohloff P, Janneck L, Bustamante N, Weaver MJ, et al. Scapular prolapse into the intrathoracic cavity in a lung transplant patient. Lancet. 2014; 384:1476.70. Orsini B, D'Journo XB, Reynaud-Gaubert M, Thomas PA. Sternal dehiscence after clamshell incision in lung transplantation treated with the STRAsbourg Thoracic Osteosyntheses System (STRATOS). Ann Thorac Surg. 2014; 97:e55–7.71. Weinkauf JG, Yiannopoulos A, Faul JL. Transcutaneous electrical nerve stimulation for severe gastroparesis after lung transplantation. J Heart Lung Transplant. 2005; 24:1444.72. Gergen AK, Madsen HJ, Tilva KR, Smith JB, Weyant MJ. Coronavirus disease 2019 in lung transplant recipients. Ann Thorac Surg. 2021; 111:e343–5.73. Wang XN, Williams TJ, McKenna MJ, Li JL, Fraser SF, Side EA, et al. Skeletal muscle oxidative capacity, fiber type, and metabolites after lung transplantation. Am J Respir Crit Care Med. 1999; 160:57–63.74. Munro PE, Button BM, Bailey M, Whitford H, Ellis SJ, Snell GI. Should lung transplant recipients routinely perform airway clearance techniques? A randomized trial. Respirology. 2008; 13:1053–60.75. Schuurmans MM, Benden C, Inci I. Practical approach to early postoperative management of lung transplant recipients. Swiss Med Wkly. 2013; 143:w13773.76. Tarrant BJ, Quinn E, Robinson R, Poulsen M, Fuller L, Snell G, et al. Post-operative, inpatient rehabilitation after lung transplant evaluation (PIRATE): a feasibility randomized controlled trial. Physiother Theory Pract. 2023; 39:1406–16.77. Kienbacher T, Achim-Gunacker G, Pachner M, Kerschan-Schindl K, Gunacker P, Habenicht R, et al. Feasibility and reliability of functional muscle tests in lung transplant recipients. Am J Phys Med Rehabil. 2018; 97:390–6.78. Mirenayat MS, Heshmatnia J, Saghebi SR, Sheikhy K, Marjani M, Fakharian A, et al. Uncommon complications of lung transplantation in a referral center. Tanaffos. 2022; 21:179–85.79. Girgis RE, Hadley RJ, Murphy ET. Pulmonary, circulatory and renal considerations in the early postoperative management of the lung transplant recipient. Glob Cardiol Sci Pract. 2023; 2023:e202318.80. Chen-Yoshikawa TF. Ischemia-reperfusion injury in lung transplantation. Cells. 2021; 10:1333.81. Avtaar Singh SS, Das De S, Al-Adhami A, Singh R, Hopkins PM, Curry PA. Primary graft dysfunction following lung transplantation: from pathogenesis to future frontiers. World J Transplant. 2023; 13:58–85.82. Ntiamoah P, Budev M, Turowski J, Lane CR, McCurry KR. Retransplantation for COVID-19-related lung graft failure: a case report of successful outcome in a critically ill lung transplant recipient. Ann Thorac Med. 2023; 18:217–8.83. Gupta VF, Halpern SE, Pontula A, Krischak MK, Reynolds JM, Klapper JA, et al. Short-term outcomes after third-time lung transplantation: a single institution experience. J Heart Lung Transplant. 2024; 43:771–9.84. Polastri M, Reed RM. Rehabilitative goals for patients undergoing lung retransplantation. J Yeungnam Med Sci. 2024; 41:134–8.85. Atkins BZ, Petersen RP, Daneshmand MA, Turek JW, Lin SS, Davis RD. Impact of oropharyngeal dysphagia on long-term outcomes of lung transplantation. Ann Thorac Surg. 2010; 90:1622–8.86. Polastri M, Paganelli GM, Dolci G, Di Ciaccio E, Prediletto I. Musculoskeletal syndrome treated with global postural re-education in double-redo lung transplantation: a case report with an 8-month follow-up. 2022;74:10.4081/reumatismo.2022.1386.87. Farquhar JM, Smith PJ, Snyder L, Gray AL, Reynolds JM, Blumenthal JA. Patterns and predictors of pain following lung transplantation. Gen Hosp Psychiatry. 2018; 50:125–30.88. Richard C, Girard F, Ferraro P, Chouinard P, Boudreault D, Ruel M, et al. Acute postoperative pain in lung transplant recipients. Ann Thorac Surg. 2004; 77:1951–5.89. Michel-Cherqui M, Fessler J, Szekely B, Glorion M, Sage E, Fischler M, et al. Complementary therapy learning in the setting of lung transplantation: a single-center observational study of appropriation and efficacy. J Clin Med. 2023; 12:1722.90. Polastri M, Venturini E, Pastore S, Dell'Amore A. Do chest expansion exercises aid re-shaping the diaphragm within the first 72 hours following lung transplantation in a usual interstitial pneumonia patient? Physiother Res Int. 2015; 20:191–6.91. Wu T, Zhou S, Wu B, Chen J, Zhu X, Cai Y. The effect of early tracheal extubation combined with physical training on pulmonary rehabilitation of patients after lung transplantation: a randomized controlled trial. J Thorac Dis. 2022; 14:1120–9.92. Estenne M, Maurer JR, Boehler A, Egan JJ, Frost A, Hertz M, et al. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant. 2002; 21:297–310.93. Todd JL, Palmer SM. Bronchiolitis obliterans syndrome: the final frontier for lung transplantation. Chest. 2011; 140:502–8.94. Verleden GM, Glanville AR, Lease ED, Fisher AJ, Calabrese F, Corris PA, et al. Chronic lung allograft dysfunction: definition, diagnostic criteria, and approaches to treatment. A consensus report from the Pulmonary Council of the ISHLT. J Heart Lung Transplant. 2019; 38:493–503.95. Subramani MV, Pandit S, Gadre SK. Acute rejection and post lung transplant surveillance. Indian J Thorac Cardiovasc Surg. 2022; 38(Suppl 2):S271–9.96. Hanks J, Girard C, Sehgal S. Acute rejection post lung transplant. Curr Opin Pulm Med. 2024; 30:391–7.97. Choi HE, Lim SN, Lee JH, Park SH. Comprehensive pulmonary rehabilitation in patients with bronchiolitis obliterans syndrome: a case series. Respir Med Case Rep. 2020; 31:101161.98. LoMauro A, Righi I, Privitera E, Vergari M, Nigro M, Aliverti A, et al. The impaired diaphragmatic function after bilateral lung transplantation: a multifactorial longitudinal study. J Heart Lung Transplant. 2020; 39:795–804.99. Sheridan PH, Cheriyan A, Doud J, Dornseif SE, Montoya A, Houck J, et al. Incidence of phrenic neuropathy after isolated lung transplantation. The Loyola University Lung Transplant Group. J Heart Lung Transplant. 1995; 14:684–91.100. Polastri M, Di Marco L, Dell’Amore A, Comellini V. Hemidiaphragm elevation after thoracic and cardiac surgical procedures: there is room for respiratory physiotherapy. Int J Ther Rehabil. 2023; 30:1–5.101. Bureau C, Van Hollebeke M, Dres M. Managing respiratory muscle weakness during weaning from invasive ventilation. Eur Respir Rev. 2023; 32:220205.102. Faccioli E, Inci I. Extracorporeal life support as a bridge to lung transplantation: a narrative review. J Thorac Dis. 2023; 15:5221–31.103. Yang J, Xie X, Li J, Li Y, Li B, Wang C, et al. Which strategy is better for lung transplantation: cardiopulmonary bypass or extracorporeal membrane oxygenation? Perfusion. 2024; Apr. 1. [Epub]. https://doi.org/10.1177/02676591241242018.104. Florian J, Watte G, Teixeira PJ, Altmayer S, Schio SM, Sanchez LB, et al. Pulmonary rehabilitation improves survival in patients with idiopathic pulmonary fibrosis undergoing lung transplantation. Sci Rep. 2019; 9:9347.105. Polastri M, Loforte A, Dell'Amore A, Nava S. Physiotherapy for patients on awake extracorporeal membrane oxygenation: a systematic review. Physiother Res Int. 2016; 21:203–9.106. Polastri M, Eden A, Loforte A, Dell'Amore A, Antonini MV, Riera J, et al. Physiotherapy for patients on extracorporeal membrane oxygenation support: how, when, and who. An international EuroELSO survey. Perfusion. 2024; 39:162–73.107. Polastri M, Swol J, Loforte A, Dell'Amore A. Extracorporeal membrane oxygenation and rehabilitation in patients with COVID-19: a scoping review. Artif Organs. 2022; 46:30–9.108. Polastri M, Eden A, Swol J. Rehabilitation for adult patients undergoing extracorporeal membrane oxygenation. Perfusion. 2024; 39(1 Suppl):115S–26S.109. Suryadinata R, Levin K, Holsworth L, Paraskeva M, Robinson P. Airway cilia recovery post lung transplantation. Immun Inflamm Dis. 2021; 9:1716–23.110. Barnes L, Reed RM, Parekh KR, Bhama JK, Pena T, Rajagopal S, et al. Mechanical ventilation for the lung transplant recipient. Curr Pulmonol Rep. 2015; 4:88–96.111. Stilma W, van Meenen DM, Valk CM, de Bruin H, Paulus F, Serpa Neto A, et al. Incidence and practice of early prone positioning in invasively ventilated COVID-19 patients: insights from the PRoVENT-COVID observational study. J Clin Med. 2021; 10:4783.112. Elmer N, Reißhauer A, Brehm K, Vockeroth C, Liebl ME. Long-term complications of prone position ventilation with relevance for acute and postacute rehabilitation: a systematic review of the literature. Eur J Phys Rehabil Med. 2023; 59:111–21.113. Oliveira VM, Piekala DM, Deponti GN, Batista DC, Minossi SD, Chisté M, et al. Safe prone checklist: construction and implementation of a tool for performing the prone maneuver. Rev Bras Ter Intensiva. 2017; 29:131–41.114. Cavenaghi S, Ferreira LL, Marino LH, Lamari NM. Respiratory physiotherapy in the pre and postoperative myocardial revascularization surgery. Rev Bras Cir Cardiovasc. 2011; 26:455–61.115. Holloszy JO. Biochemical adaptations in muscle. Effects of exercise on mitochondrial oxygen uptake and respiratory enzyme activity in skeletal muscle. J Biol Chem. 1967; 242:2278–82.116. Plotkin DL, Roberts MD, Haun CT, Schoenfeld BJ. Muscle fiber type transitions with exercise training: shifting perspectives. Sports (Basel). 2021; 9:127.117. Wilson JM, Loenneke JP, Jo E, Wilson GJ, Zourdos MC, Kim JS. The effects of endurance, strength, and power training on muscle fiber type shifting. J Strength Cond Res. 2012; 26:1724–9.118. Fernández AM, Ruiz E, Cantador B, González FJ, Baamonde C, Álvarez A. Case report of complex chest wall repair for sternal dehiscence after bilateral lung transplantation. Transplant Proc. 2023; 55:2307–8.119. Muthialu N, McIntyre D, McIntosh N, Plumridge J, Elliott MJ. Disturbingly high fracture rate of STRATOS bars in pectus corrections. Eur J Cardiothorac Surg. 2019; 55:300–3.120. Sharma PK, Willems TP, Touw DJ, Woudstra W, Erasmus ME, Ebels T. Implant failure: STRATOS system for pectus repair. Ann Thorac Surg. 2017; 103:1536–43.121. Opsomer R, Kuypers D. COVID-19 and solid organ transplantation: finding the right balance. Transplant Rev (Orlando). 2022; 36:100710.122. Watanabe T, Hirama T, Akiba M, Watanabe T, Watanabe Y, Oishi H, et al. COVID-19 pneumonia in lung transplant recipients: understanding risk factors and treatment outcomes in Japan. Clin Exp Med. 2024; 24:123.123. Reemann L, Kneidinger N, Sczepanski B, Koczulla AR. COVID-19 in lung transplant recipients: a report on 10 recent cases. Viruses. 2024; 16:709.124. Antonacci F, Petroncini M, Salvaterra E, Bertoglio P, Daddi N, Lai G, et al. Lung transplant recipients and COVID-19: report of two cases. J Clin Med. 2023; 12:4287.125. Hussein M, Gallais F, Dégot T, Hirschi S, Leroux J, Riou M, et al. Impact of the COVID-19 pandemic on lung transplant patients and on a cohort of patients with rare lung disease: a single-center study. Respir Med Res. 2024; 85:101100.126. Alvarez-Aquino FG, Shah S. Lung transplantation: challenges in the COVID-19 era, a narrative review of the literature. Curr Chall Thorac Surg. 2021; 3:29.127. Polastri M, Carbonara P, Prediletto I, Gardini A, Venturoli F, Tagariello F, et al. Effects of early rehabilitation on motor function, dyspnoea intensity, respiratory muscle performance and handgrip strength in patients with COVID-19: an observational study. Int J Ther Rehabil. 2022; 29:1–13.128. Saeki T, Ogawa F, Chiba R, Nonogaki M, Uesugi J, Takeuchi I, et al. Rehabilitation therapy for a COVID-19 patient who received mechanical ventilation in Japan. Am J Phys Med Rehabil. 2020; 99:873–5.129. Nicolosi C, Barber K, Draganich C, Niehaus W. Inpatient rehabilitation after COVID-19 hospitalization in a patient with lung transplant: a case study. Am J Phys Med Rehabil. 2021; 100:627–30.130. Rawashdeh B, Yaghmour N, Sulieman D, Abuassi M, Cooper M. Takotsubo cardiomyopathy after solid organ transplantation: a scoping review. Ann Med Surg (Lond). 2024; 86:2883–91.131. Ghadri JR, Bataisou RD, Diekmann J, Lüscher TF, Templin C. First case of atypical takotsubo cardiomyopathy in a bilateral lung-transplanted patient due to acute respiratory failure. Eur Heart J Acute Cardiovasc Care. 2015; 4:482–5.132. Santacruz JF, Mehta AC. Airway complications and management after lung transplantation: ischemia, dehiscence, and stenosis. Proc Am Thorac Soc. 2009; 6:79–93.133. Yataco JC, Dweik RA. Pleural effusions: evaluation and management. Cleve Clin J Med. 2005; 72:854.134. Light RW. Pleural effusions. Med Clin North Am. 2011; 95:1055–70.135. Beaudoin S, Gonzalez AV. Evaluation of the patient with pleural effusion. CMAJ. 2018; 190:E291–5.136. Polastri M, Pantaleo A. Managing a left pleural effusion after aortic surgery. Eur Rev Med Pharmacol Sci. 2012; 16(Suppl 4):78–80.137. Polastri M, Savini C, Di Marco L, Jafrancesco G, Semprini A, Grigioni F. Post-operative pleural effusion in a heart transplant recipient: a single-case study of physiotherapy treatment. Int J Ther Rehabil. 2017; 24:302–5.138. Gould SW, Radecki PD, Gembala-Parsons RB, Caroline DF. Intrathoracic scapular prolapse after thoracotomy. Can Assoc Radiol J. 1994; 45:145–7.139. Eguchi T, Kondo R, Shiina T, Yoshida K. An intrathoracic scapular prolapse with hemorrhagic shock after a thoracotomy. Interact Cardiovasc Thorac Surg. 2011; 12:326–7.140. Nishimura M, Suzuki H. Scapular prolapse into the intrathoracic cavity after lobectomy with rib resection. Ann Thorac Surg. 2018; 105:e181.141. Wu Q, Qiao K, Liu J, Zhen S, Zhou Z. Scapular dislocation following radical surgical excision of lung sarcomatoid carcinoma: a rare case report. Medicine (Baltimore). 2024; 103:e36884.142. Polastri M. Physiotherapy for lung transplant candidates and recipients: timeframe from pre-operative to long-term care. Int J Ther Rehabil. 2019; 26:1–6.143. Simanovski J, Ralph J. Readmissions after lung transplantation. Prog Transplant. 2020; 30:365–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rehabilitative goals for patients undergoing lung retransplantation
- Critical Care Management Following Lung Transplantation
- Indications for Lung Transplantation and Patient Selection
- Recent Advancement in Heart and Lung Transplantation
- Anesthesia for non-pulmonary surgical intervention following lung transplantation: two cases report