Child Kidney Dis.
2024 Oct;28(3):131-137. 10.3339/ckd.24.021.
Lupus anticoagulant-hypoprothrombinemia syndrome with lupus nephritis in a girl misdiagnosed with immunoglobulin A nephropathy: a case report
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Republic of Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea
- 3Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Republic of Korea
- KMID: 2560483
- DOI: http://doi.org/10.3339/ckd.24.021
Abstract
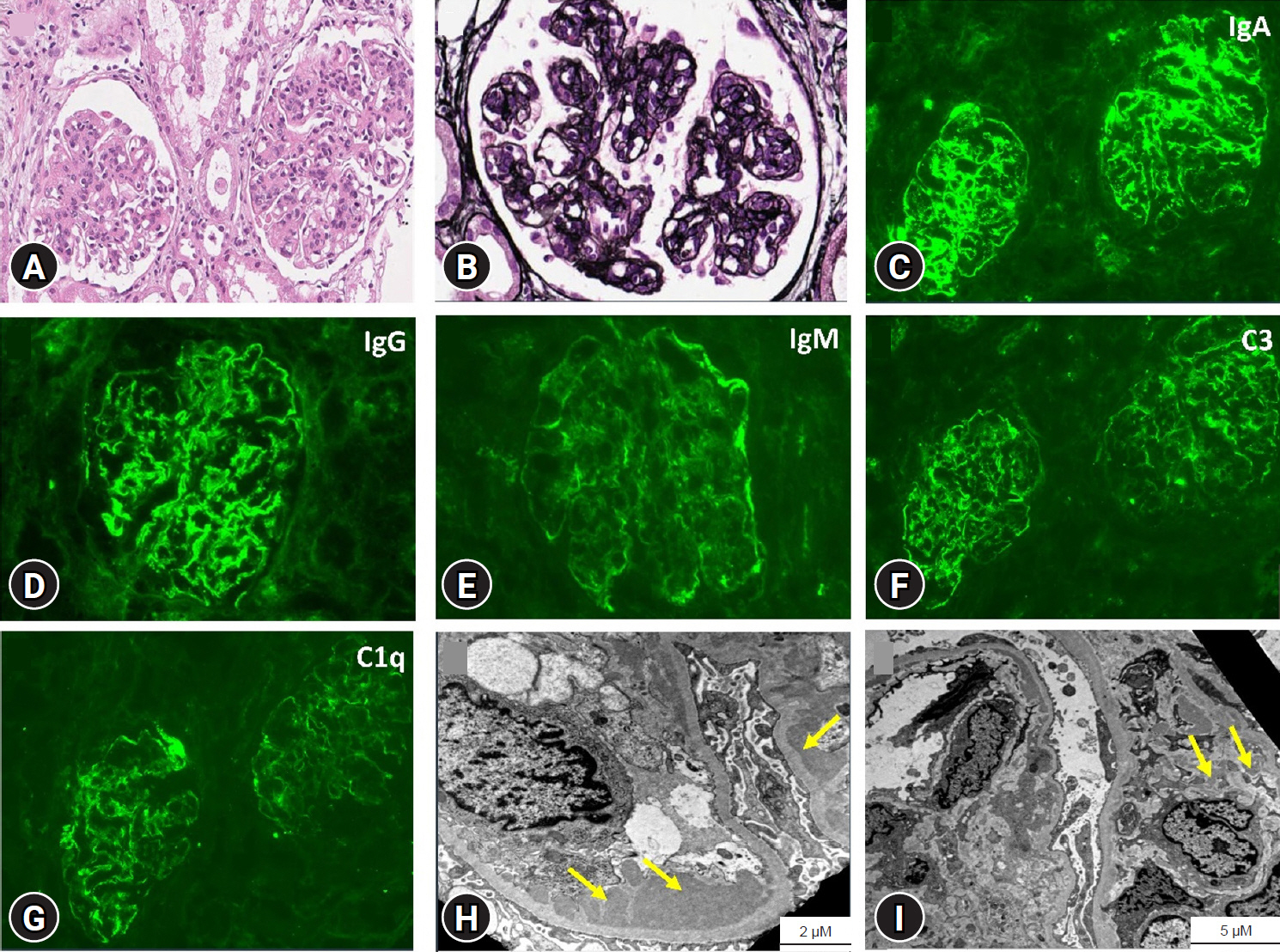
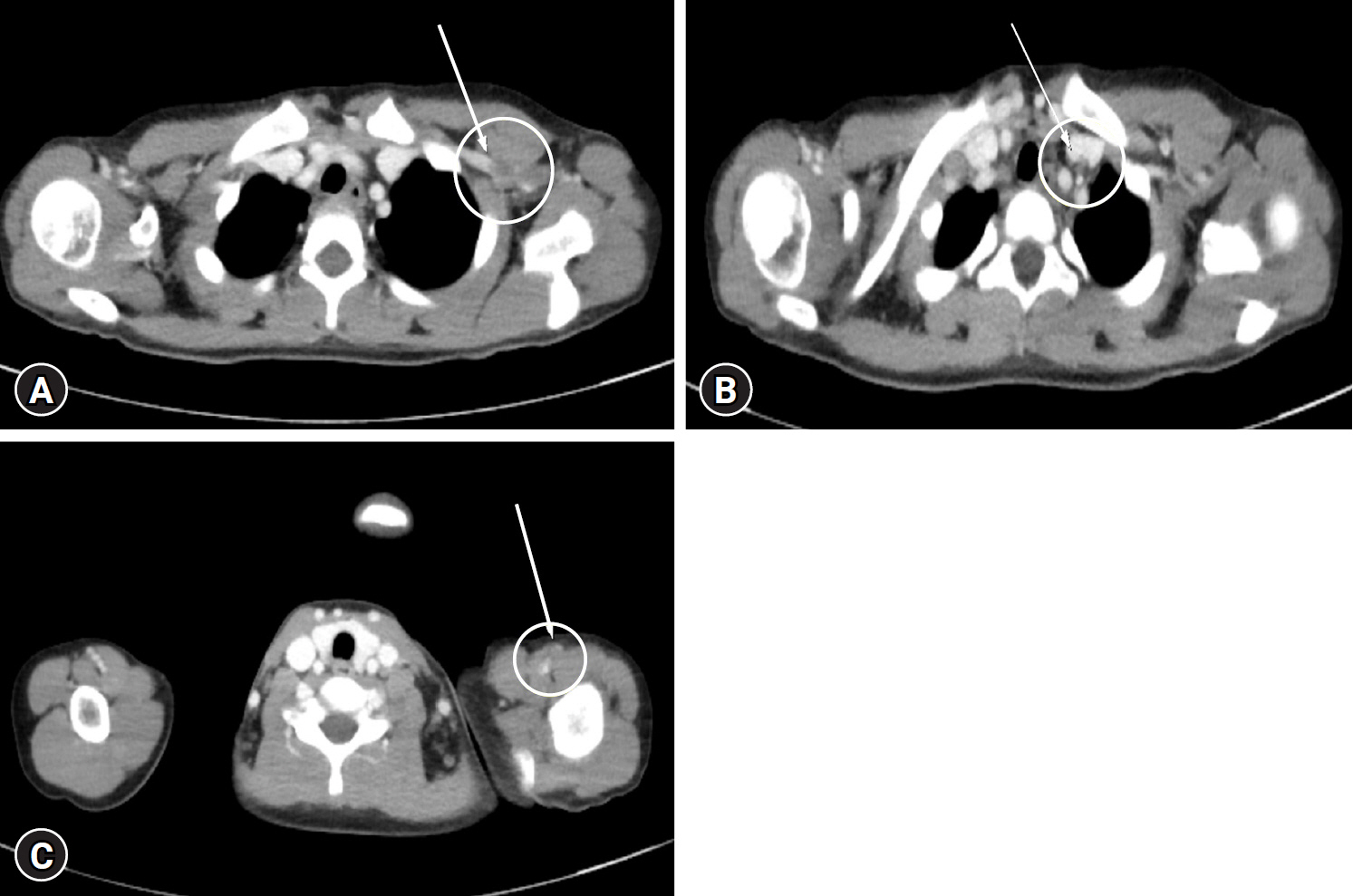
- Distinguishing lupus nephritis (LN) from other glomerulopathies, such as immunoglobulin A nephropathy (IgAN), poses a diagnostic challenge owing to overlapping clinical and histopathologic findings. Lupus anticoagulant-hypoprothrombinemia syndrome (LAHPS) is a rare and potentially fatal disorder characterized by the presence of lupus anticoagulant and acquired factor II deficiency. We report a pediatric case of LN with LAHPS, which was initially diagnosed as IgAN. An 8-year-old girl presented with gross hematuria with nephrotic syndrome. Based on the kidney biopsy results, treatment for IgAN with membranoproliferative pattern was initiated. Two months later, she developed left upper extremity swelling with multiple vein thromboses requiring anticoagulation; treatment led to remission, allowing discontinuation of immunosuppressants within 8 months. Gross hematuria recurred 10 months later and was accompanied by hypocomplementemia; positive antinuclear, anti-double stranded DNA, and triple antiphospholipid antibodies; and factor II deficiency, prompting revision of the diagnosis to LN and LAHPS. Initial delay in LN diagnosis was attributed to the patient’s young age, nonspecific symptoms, and inconclusive laboratory and histopathological findings. Immunosuppressive therapy for IgAN partially improved LN, further complicating the diagnosis. This case emphasized the importance of clinical suspicion; integrating clinical, serological, and histopathological data; and considering LAHPS in differential diagnosis of glomerulonephritis with coagulopathy.
Keyword
Figure
Reference
-
References
1. Mazodier K, Arnaud L, Mathian A, Costedoat-Chalumeau N, Haroche J, Frances C, et al. Lupus anticoagulant-hypoprothrombinemia syndrome: report of 8 cases and review of the literature. Medicine (Baltimore). 2012; 91:251–60.2. Acedo N, Alonso A, Feijoo ES, Garcia C, Ortiz AM, Alegre A. Lupus anticoagulant hypoprothrombinemia syndrome: a case report. Clin Case Rep. 2023; 11:e7071.
Article3. Kim JS, Kim MJ, Bae EY, Jeong DC. Pulmonary hemorrhage in pediatric lupus nticoagulant hypoprothrombinemia syndrome. Korean J Pediatr. 2014; 57:202–5.
Article4. Sarker T, Roy S, Hollon W, Rajpurkar M. Lupus anticoagulant acquired hypoprothrombinemia syndrome in childhood: two distinct patterns and review of the literature. Haemophilia. 2015; 21:754–60.
Article5. Schreiber K, Sciascia S, de Groot PG, Devreese K, Jacobsen S, Ruiz-Irastorza G, et al. Antiphospholipid syndrome. Nat Rev Dis Primers. 2018; 4:17103.
Article6. Thakral A, Klein-Gitelman MS. An update on treatment and management of pediatric systemic lupus erythematosus. Rheumatol Ther. 2016; 3:209–19.
Article7. Pattrapornpisut P, Avila-Casado C, Reich HN. IgA nephropathy: core curriculum 2021. Am J Kidney Dis. 2021; 78:429–41.
Article8. Anders HJ, Saxena R, Zhao MH, Parodis I, Salmon JE, Mohan C. Lupus nephritis. Nat Rev Dis Primers. 2020; 6:7.
Article9. Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int. 2004; 65:521–30.
Article10. Bajaj SP, Rapaport SI, Fierer DS, Herbst KD, Schwartz DB. A mechanism for the hypoprothrombinemia of the acquired hypoprothrombinemia-lupus anticoagulant syndrome. Blood. 1983; 61:684–92.
Article11. Peralta-Amaro AL, Triana-Gonzalez S, Manzo-Carballo MF, Vera Lastra OL, Garcia-Chavez J, Lucas-Hernandez A. Antiphospholipid syndrome and lupus anticoagulant-hypoprothrombinemia. QJM. 2023; 116:308–9.
Article12. Lee YA. New classification criteria for systemic lupus erythematosus. Korean J Med. 2020; 95:151–61.
Article13. Levin A. Management of membranoproliferative glomerulonephritis: evidence-based recommendations. Kidney Int Suppl. 1999; 70:S41–6.
Article14. Andeen NK, Jefferson JA, Akilesh S, Alpers CE, Bissonnette ML, Finn LS, et al. IgA-dominant glomerulonephritis with a membranoproliferative pattern of injury. Hum Pathol. 2018; 81:272–80.
Article15. Iitaka K, Yamamoto A, Ogawa N, Sekine T, Tamai S, Motoyama O. IgA-associated glomerulonephritis with membranoproliferative glomerulonephritis-like pattern in two children. Clin Exp Nephrol. 2003; 7:284–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lupus anticoagulant hypoprothrombinemia syndrome associated with a hemorrhagic ovarian cyst in a girl with systemic lupus erythematosus: a case report
- A Case of Systemic Lupus Erythematosus Involving the Kidneys in a Patient with IgA Nephropathy
- Pulmonary hemorrhage in pediatric lupus anticoagulant hypoprothrombinemia syndrome
- Lupus Anticoagulant-hypoprothrombinemia Syndrome as an Initial Manifestation of Systemic Lupus Erythematosus: A Case Report
- A case of Lupus Nephritis