Child Kidney Dis.
2024 Jun;28(2):80-85. 10.3339/ckd.24.007.
Lupus anticoagulant hypoprothrombinemia syndrome associated with a hemorrhagic ovarian cyst in a girl with systemic lupus erythematosus: a case report
- Affiliations
-
- 1Department of Pediatrics, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Republic of Korea
- KMID: 2557074
- DOI: http://doi.org/10.3339/ckd.24.007
Abstract
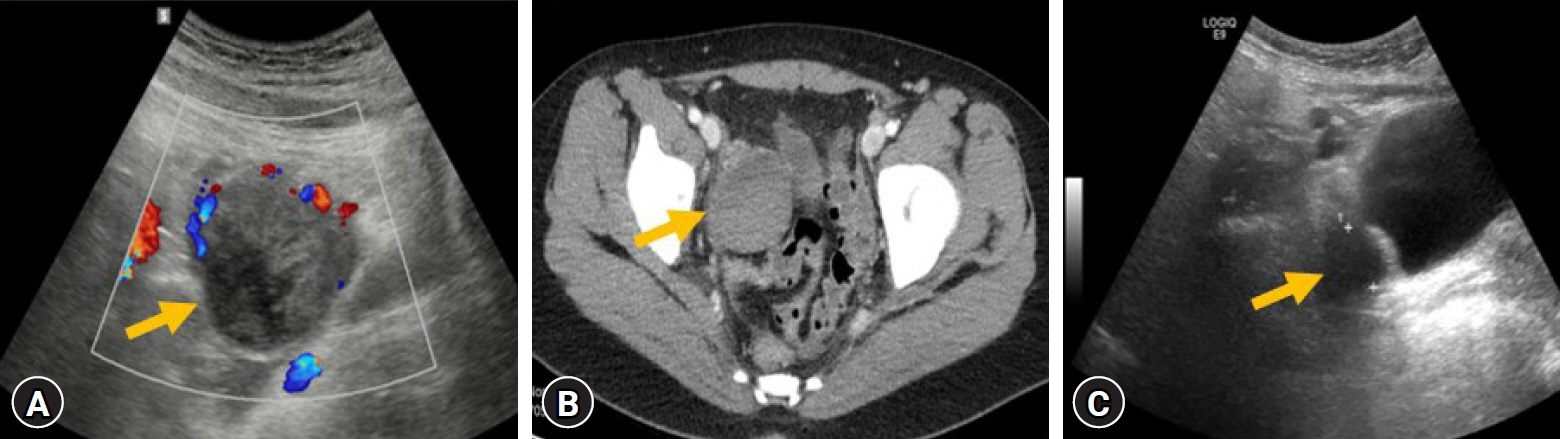
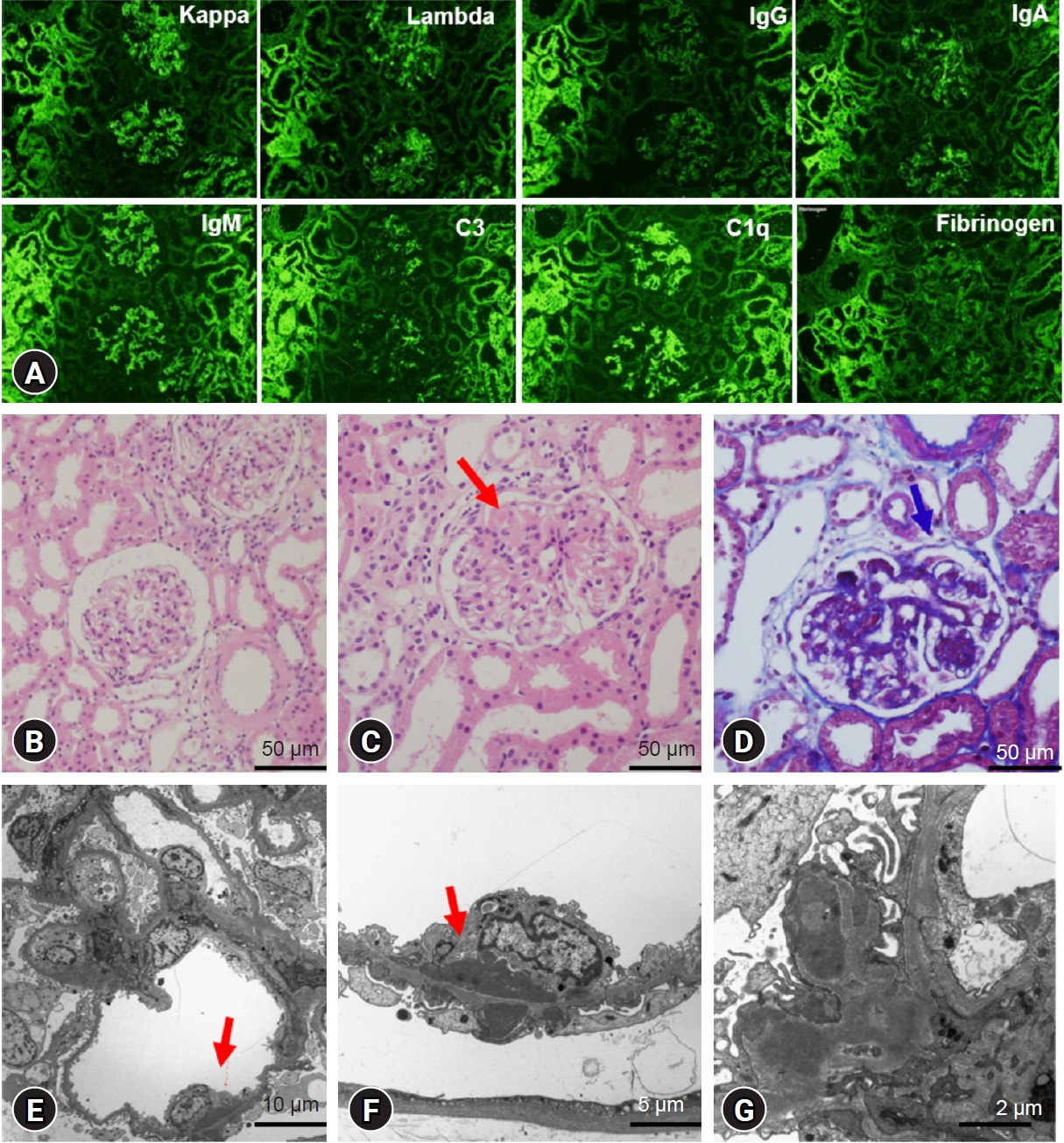
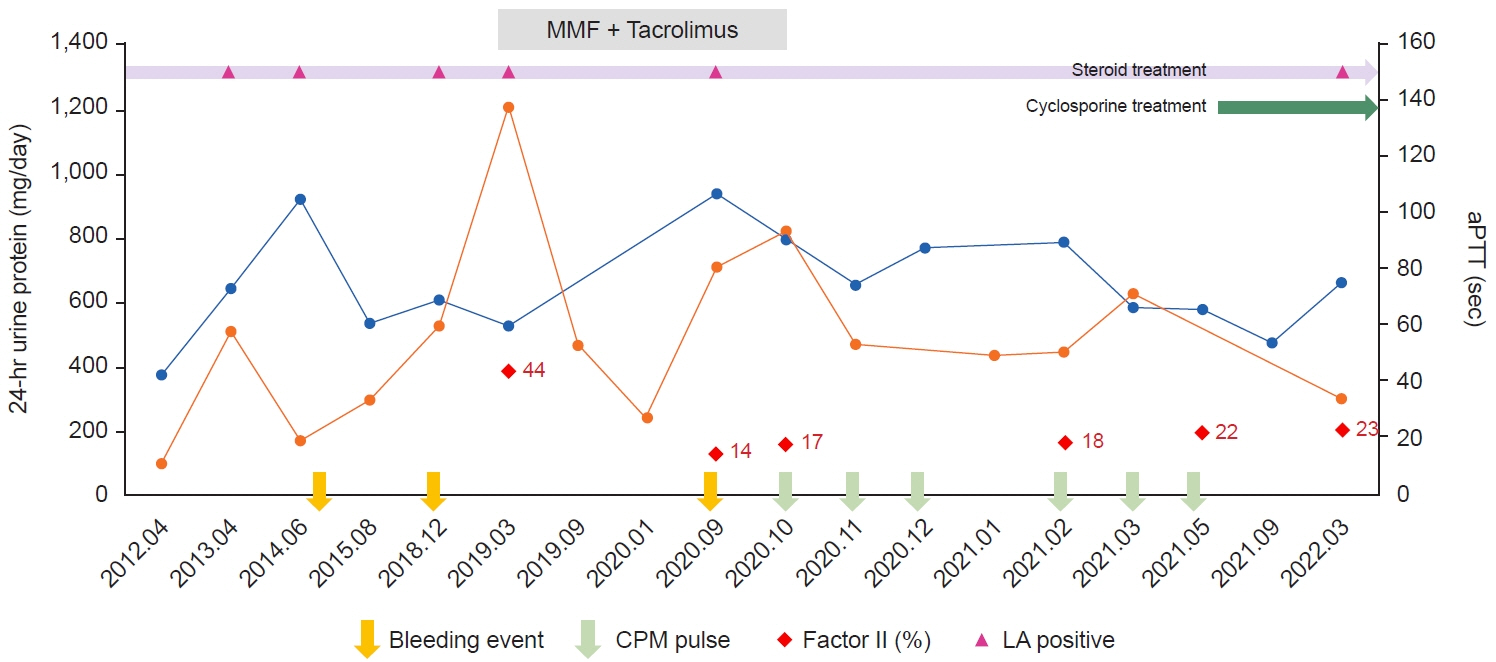
- Lupus anticoagulant hypoprothrombinemia syndrome (LAHPS) is a rare entity characterized by the presence of lupus anticoagulant (LA) and prothrombin (factor II) deficiency. It may cause severe bleeding contrary to classical antiphospholipid syndrome. Here, we report a case of LAHPS presenting with a hemorrhagic ovarian cyst in a 17-year-old girl with systemic lupus erythematosus (SLE) nephritis. She had been followed up for 8 years. Her first manifestation of SLE was prolonged gingival bleeding after tooth extraction at 9 years of age. During the follow-up period, she had neither severe bleeding nor thrombotic complications despite a positive LA and a prolonged activated partial thromboplastin time (aPTT). At this visit, the patient presented with colicky abdominal pain, a hemorrhagic ovarian cyst, a prolonged prothrombin time, a prolonged aPTT, a low factor II level, and a positive LA, leading to the diagnosis of LAHPS. While a hemorrhagic ovarian cyst resolved completely in 3 months, she received oral pill, transfusions of red blood cells and plasma, and intravenous cyclophosphamide pulse therapy in combination with glucocorticoids due to persistent menorrhagia, anemia, prolonged aPTT, and lupus flaring. Thus, LAHPS needs to be considered in SLE patients with positive LA and prolonged aPTT.
Keyword
Figure
Reference
-
References
1. Chung CH, Park CY. Lupus anticoagulant-hypoprothrombinemia in healthy adult. Korean J Intern Med. 2008; 23:149–51.
Article2. Mulliez SM, De Keyser F, Verbist C, Vantilborgh A, Wijns W, Beukinga I, et al. Lupus anticoagulant-hypoprothrombinemia syndrome: report of two cases and review of the literature. Lupus. 2015; 24:736–45.
Article3. Atsumi T, Koike T. Clinical relevance of antiprothrombin antibodies. Autoimmun Rev. 2002; 1:49–53.
Article4. Montes de Oca MA, Babron MC, Bletry O, Broyer M, Courtecuisse V, Fontaine JL, et al. Thrombosis in systemic lupus erythematosus: a French collaborative study. Arch Dis Child. 1991; 66:713–7.
Article5. Rapaport SI, Ames SB, Duvall BJ. A plasma coagulation defect in systemic lupus erythematosus arising from hypoprothrombinemia combined with antiprothrombinase activity. Blood. 1960; 15:212–27.
Article6. Hoffman M, Meng ZH, Roberts HR, Monroe DM. Rethinking the coagulation cascade. Jpn J Thromb Hemost. 2005; 16:70–81.
Article7. Lackner KJ, Muller-Calleja N. Pathogenesis of the antiphospholipid syndrome revisited: time to challenge the dogma. J Thromb Haemost. 2016; 14:1117–20.
Article8. Mazodier K, Arnaud L, Mathian A, Costedoat-Chalumeau N, Haroche J, Frances C, et al. Lupus anticoagulant-hypoprothrombinemia syndrome: report of 8 cases and review of the literature. Medicine (Baltimore). 2012; 91:251–60.9. Kocheril AP, Vettiyil GI, George AS, Shah S, Geevar T, Dave RG, et al. Pediatric systemic lupus erythematosus with lupus anticoagulant hypoprothrombinemia syndrome: a case series with review of literature. Lupus. 2021; 30:641–8.
Article10. Bajaj SP, Rapaport SI, Fierer DS, Herbst KD, Schwartz DB. A mechanism for the hypoprothrombinemia of the acquired hypoprothrombinemia-lupus anticoagulant syndrome. Blood. 1983; 61:684–92.
Article11. Laboratory Corporation of America Holdings (LabCorp). Lupus anticoagulants [Internet]. LabCorp; 2024 [cited 2024 Feb 16]. Available from: https://www.labcorp.com/resource/lupus-anticoagulants/.12. Tarr T, Lakos G, Bhattoa HP, Soltesz P, Shoenfeld Y, Szegedi G, et al. Clinical thrombotic manifestations in SLE patients with and without antiphospholipid antibodies: a 5-year follow-up. Clin Rev Allergy Immunol. 2007; 32:131–7.
Article13. Cetin Gedik K, Siddique S, Aguiar CL. Rituximab use in pediatric lupus anticoagulant hypoprothrombinemia syndrome: report of three cases and review of the literature. Lupus. 2018; 27:1190–7.
Article14. Lim W. Antiphospholipid syndrome. Hematology Am Soc Hematol Educ Program. 2013; 2013:675–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lupus Anticoagulant-hypoprothrombinemia Syndrome as an Initial Manifestation of Systemic Lupus Erythematosus: A Case Report
- Lupus Anticoagulant-hypoprothrombinemia Syndrome that did not Progress to Systemic Lupus Erythematosus: A Case Report
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus
- A case of Limited Scleroderma Associated with Antiphospholipid Syndrome
- A Case of Systemic Lupus Erythematosus and Secondary AntiphospholipidSyndrome Presenting as Livedo Reticularis