Child Kidney Dis.
2024 Oct;28(3):124-130. 10.3339/ckd.24.015.
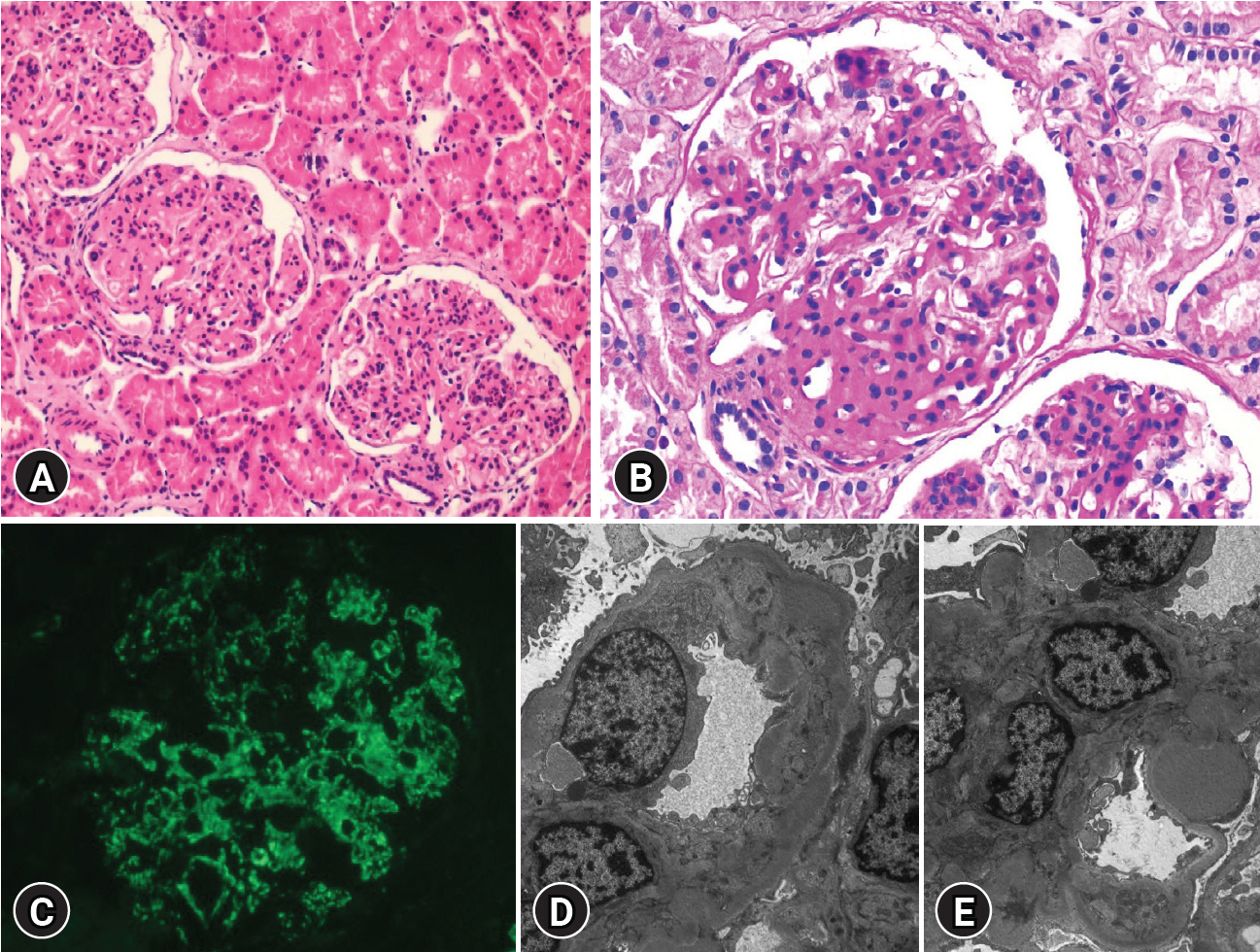
C3 glomerulonephritis with genetically confirmed C3 deficiency in a pediatric patient: a case report
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Republic of Korea
- 2Division of Pediatric Nephrology, Severance Children’s Hospital, Seoul, Republic of Korea
- 3Institute of Kidney Disease Research, Yonsei University College of Medicine, Seoul, Republic of Korea
- 4Department of Pediatrics, Gangnam Severance Hospital, Seoul, Republic of Korea
- 5Department of Clinical Genetics, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
- 6Institute for Immunology and Immunological Diseases, Yonsei University College of Medicine, Seoul, Republic of Korea
- 7Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea
- 8Dr. Cho’s Kidney Clinic, Seoul, Republic of Korea
- KMID: 2560482
- DOI: http://doi.org/10.3339/ckd.24.015
Abstract
- Complement component 3 glomerulonephritis (C3GN) is a rare kidney disease characterized by complement dysregulation that results in prominent complement component 3 (C3) deposition in the kidneys. The clinical course of C3GN varies from mild hematuria to progressive chronic kidney disease. In most patients, C3GN is driven by acquired factors, namely, autoantibodies that target C3 or C5 convertases. Genetic variations in complement-related genes are less frequent. We report the case of a 9-yearold Korean boy who presented with microscopic hematuria and a persistently low C3 level and had biopsy findings of C3GN, with the presence of a C3 gene mutation: a frameshift mutation associated with C3 deficiency. However, the patient did not exhibit any other symptoms of complement deficiency. Direct DNA sequencing of his family members revealed the same genetic mutation in his father and older brother. This case report is significant because there are very few such reports worldwide concerning gene mutations related to C3 deficiency to be discovered in patients with C3GN. Explaining C3GN pathogenesis is challenging; therefore, additional research is required in the future.
Figure
Reference
-
References
1. Kim YJ. Pathology of C3 glomerulonephritis. J Korean Soc Pediatr Nephrol. 2013; 17:1–5.
Article2. Appel GB. C3 glomerulopathy: a new disease comes of age. Mayo Clin Proc. 2018; 93:968–9.
Article3. Sethi S, Fervenza FC, Zhang Y, Zand L, Vrana JA, Nasr SH, et al. C3 glomerulonephritis: clinicopathological findings, complement abnormalities, glomerular proteomic profile, treatment, and follow-up. Kidney Int. 2012; 82:465–73.
Article4. Smith RJH, Appel GB, Blom AM, Cook HT, D'Agati VD, Fakhouri F, et al. C3 glomerulopathy: understanding a rare complement-driven renal disease. Nat Rev Nephrol. 2019; 15:129–43.
Article5. Servais A, Noel LH, Fremeaux-Bacchi V, Lesavre P. C3 glomerulopathy. Contrib Nephrol. 2013; 181:185–93.
Article6. Ravindran A, Fervenza FC, Smith RJH, De Vriese AS, Sethi S. C3 glomerulopathy: ten years' experience at Mayo Clinic. Mayo Clin Proc. 2018; 93:991–1008.
Article7. Schroder-Braunstein J, Kirschfink M. Complement deficiencies and dysregulation: Pathophysiological consequences, modern analysis, and clinical management. Mol Immunol. 2019; 114:299–311.
Article8. Martinez-Barricarte R, Heurich M, Valdes-Canedo F, Vazquez-Martul E, Torreira E, Montes T, et al. Human C3 mutation reveals a mechanism of dense deposit disease pathogenesis and provides insights into complement activation and regulation. J Clin Invest. 2010; 120:3702–12.
Article9. Xiao X, Pickering MC, Smith RJ. C3 glomerulopathy: the genetic and clinical findings in dense deposit disease and C3 glomerulonephritis. Semin Thromb Hemost. 2014; 40:465–71.
Article10. Barbier M, Gross MS, Aubart M, Hanna N, Kessler K, Guo DC, et al. MFAP5 loss-of-function mutations underscore the involvement of matrix alteration in the pathogenesis of familial thoracic aortic aneurysms and dissections. Am J Hum Genet. 2014; 95:736–43.
Article11. Li Y, Kong Y, Duan W, Yu S, Zhou X, Hu Y, et al. Evaluating the monogenic contribution and genotype-phenotype correlation in patients with isolated thoracic aortic aneurysm. Eur J Hum Genet. 2021; 29:1129–38.
Article12. Zhang H, Apfelroth SD, Hu W, Davis EC, Sanguineti C, Bonadio J, et al. Structure and expression of fibrillin-2, a novel microfibrillar component preferentially located in elastic matrices. J Cell Biol. 1994; 124:855–63.
Article13. Okura Y, Kobayashi I, Yamada M, Sasaki S, Yamada Y, Kamioka I, et al. Clinical characteristics and genotype-phenotype correlations in C3 deficiency. J Allergy Clin Immunol. 2016; 137:640–4.
Article14. Kida M, Fujioka H, Kosaka Y, Hayashi K, Sakiyama Y, Ariga T. The first confirmed case with C3 deficiency caused by compound heterozygous mutations in the C3 gene; a new aspect of pathogenesis for C3 deficiency. Blood Cells Mol Dis. 2008; 40:410–3.
Article15. Bomback AS, Smith RJ, Barile GR, Zhang Y, Heher EC, Herlitz L, et al. Eculizumab for dense deposit disease and C3 glomerulonephritis. Clin J Am Soc Nephrol. 2012; 7:748–56.
Article