Child Kidney Dis.
2024 Oct;28(3):99-105. 10.3339/ckd.24.013.
Congenital solitary functioning kidney: evaluations to do which, when, and how
- Affiliations
-
- 1Department of Pediatrics, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Republic of Korea
- KMID: 2560478
- DOI: http://doi.org/10.3339/ckd.24.013
Abstract
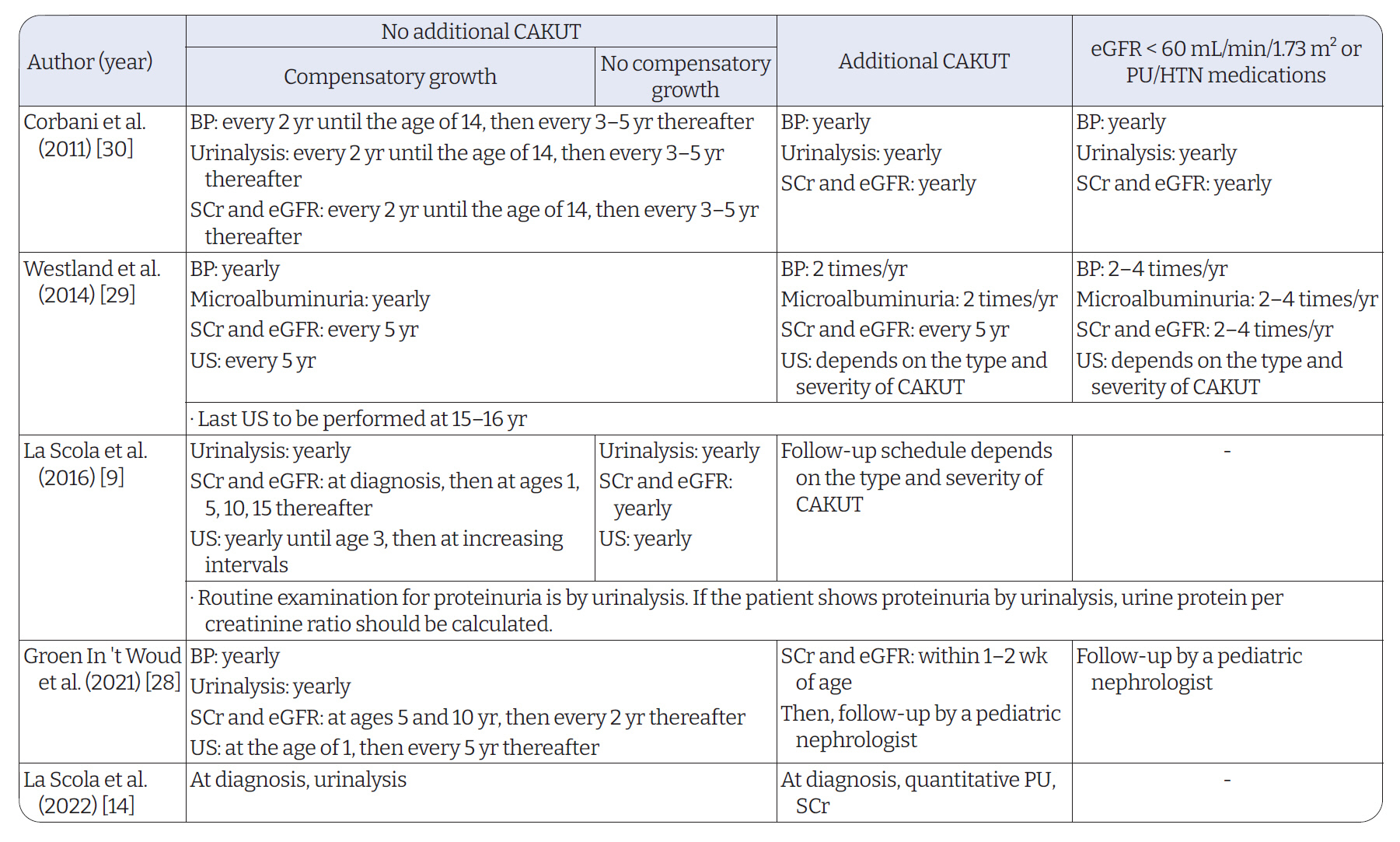
- Congenital solitary functioning kidney (CSFK) is characterized by an anatomical or functional absence of one kidney from birth. When suspected on perinatal ultrasonography (US), repeat US after birth should be performed for confirmation. Although postnatal 99mTc-dimercaptosuccinic acid scintigraphy (DMSA scan) is the gold standard for confirming CSFK, it carries the risk of radiation exposure; US alone is sufficient when performed by an experienced radiologist. One-third of patients with CSFK have additional congenital anomalies of the kidney and urinary tract at the solitary functioning kidney, the most common of which is vesicoureteral reflux. As evidence regarding vesicoureteral reflux with normal kidney US is correlated with significant urinary tract infection is lacking, voiding cystourethrogram may be considered in patients with CSFK with abnormal US findings. Furthermore, approximately 30% of patients with CSFK have extrarenal malformations. Moreover, up to 10% of them have syndromic features. In particular, examining for female genitalia malformations, which can have potential for complications from untreated obstructive malformations, is important. In conclusion, DMSA scan and voiding cystourethrogram are not necessary for all patients with CSFK, and the risk of each patient should be assessed to determine which test is needed during follow-up. The presence of extrarenal manifestations should also always be considered.
Figure
Reference
-
References
1. Hiraoka M, Tsukahara H, Ohshima Y, Kasuga K, Ishihara Y, Mayumi M. Renal aplasia is the predominant cause of congenital solitary kidneys. Kidney Int. 2002; 61:1840–4.
Article2. Schreuder MF, Westland R, van Wijk JA. Unilateral multicystic dysplastic kidney: a meta-analysis of observational studies on the incidence, associated urinary tract malformations and the contralateral kidney. Nephrol Dial Transplant. 2009; 24:1810–8.
Article3. Westland R, Schreuder MF, Ket JC, van Wijk JA. Unilateral renal agenesis: a systematic review on associated anomalies and renal injury. Nephrol Dial Transplant. 2013; 28:1844–55.
Article4. Kim S, Chang Y, Lee YR, Jung HS, Hyun YY, Lee KB, et al. Solitary kidney and risk of chronic kidney disease. Eur J Epidemiol. 2019; 34:879–88.
Article5. Sanna-Cherchi S, Ravani P, Corbani V, Parodi S, Haupt R, Piaggio G, et al. Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int. 2009; 76:528–33.
Article6. Westland R, Kurvers RA, van Wijk JA, Schreuder MF. Risk factors for renal injury in children with a solitary functioning kidney. Pediatrics. 2013; 131:e478–85.
Article7. Marzuillo P, Guarino S, Grandone A, Di Somma A, Della Vecchia N, Esposito T, et al. Outcomes of a cohort of prenatally diagnosed and early enrolled patients with congenital solitary functioning kidney. J Urol. 2017; 198:1153–8.
Article8. Whittam BM, Calaway A, Szymanski KM, Carroll AE, Misseri R, Kaefer M, et al. Ultrasound diagnosis of multicystic dysplastic kidney: is a confirmatory nuclear medicine scan necessary? J Pediatr Urol. 2014; 10:1059–62.
Article9. La Scola C, Ammenti A, Puccio G, Lega MV, De Mutiis C, Guiducci C, et al. Congenital solitary kidney in children: size matters. J Urol. 2016; 196:1250–6.
Article10. Mansoor O, Chandar J, Rodriguez MM, Abitbol CL, Seeherunvong W, Freundlich M, et al. Long-term risk of chronic kidney disease in unilateral multicystic dysplastic kidney. Pediatr Nephrol. 2011; 26:597–603.
Article11. Groen In 't Woud S, Renkema KY, Schreuder MF, Wijers CH, van der Zanden LF, Knoers NV, et al. Maternal risk factors involved in specific congenital anomalies of the kidney and urinary tract: a case-control study. Birth Defects Res A Clin Mol Teratol. 2016; 106:596–603.12. Urisarri A, Gil M, Mandia N, Aldamiz-Echevarria L, Iria R, Gonzalez-Lamuno D, et al. Retrospective study to identify risk factors for chronic kidney disease in children with congenital solitary functioning kidney detected by neonatal renal ultrasound screening. Medicine (Baltimore). 2018; 97:e11819.
Article13. Krill A, Cubillos J, Gitlin J, Palmer LS. Abdominopelvic ultrasound: a cost-effective way to diagnose solitary kidney. J Urol. 2012; 187:2201–4.
Article14. La Scola C, Ammenti A, Bertulli C, Bodria M, Brugnara M, Camilla R, et al. Management of the congenital solitary kidney: consensus recommendations of the Italian Society of Pediatric Nephrology. Pediatr Nephrol. 2022; 37:2185–207.
Article15. van Vuuren SH, van der Doef R, Cohen-Overbeek TE, Goldschmeding R, Pistorius LR, de Jong TP. Compensatory enlargement of a solitary functioning kidney during fetal development. Ultrasound Obstet Gynecol. 2012; 40:665–8.
Article16. Marzuillo P, Guarino S, Grandone A, Di Somma A, Diplomatico M, Rambaldi PF, et al. Congenital solitary kidney size at birth could predict reduced eGFR levels later in life. J Perinatol. 2019; 39:129–34.
Article17. Rosenbaum DM, Korngold E, Teele RL. Sonographic assessment of renal length in normal children. AJR Am J Roentgenol. 1984; 142:467–9.
Article18. Basturk T, Koc Y, Ucar Z, Sakaci T, Ahbap E, Kara E, et al. Renal damage frequency in patients with solitary kidney and factors that affect progression. Int J Nephrol. 2015; 2015:876907.
Article19. Weinstein A, Goodman TR, Iragorri S. Simple multicystic dysplastic kidney disease: end points for subspecialty follow-up. Pediatr Nephrol. 2008; 23:111–6.
Article20. Wang Y, Wang Z, Wang W, Ren H, Zhang W, Chen N. Analysis of factors associated with renal function in Chinese adults with congenital solitary kidney. Intern Med. 2010; 49:2203–9.
Article21. Dinkel E, Ertel M, Dittrich M, Peters H, Berres M, Schulte-Wissermann H. Kidney size in childhood: sonographical growth charts for kidney length and volume. Pediatr Radiol. 1985; 15:38–43.
Article22. Chen JJ, Zhi J, Mao W, Steinhardt GF. MrNomogram: a web-based multivariable pediatric renal nomogram. J Pediatr Urol. 2006; 2:436–8.
Article23. Zerin JM, Blane CE. Sonographic assessment of renal length in children: a reappraisal. Pediatr Radiol. 1994; 24:101–6.
Article24. Blachman-Braun R, Camp MM, Becerra MF, Guevara CG, Velasquez MC, Moscardi PR, et al. Voiding cystourethrogram in children with unilateral multicystic dysplastic kidney: is it still necessary? Urology. 2020; 139:156–60.
Article25. Brown C, McLeod D, Ching C. Knowledge of vesicoureteral reflux obtained by screening voiding cystourethrogram in children with multicystic dysplastic kidney does not change patient management or prevent febrile urinary tract infection. J Pediatr Urol. 2019; 15:267.
Article26. Ross I, Ahn HJ, Roelof B, Barber T, Huynh V, Rockette A, et al. Sonographic assessment of the effect of vesicoureteral reflux and urinary tract infections on growth of the pediatric solitary kidney. J Pediatr Urol. 2015; 11:145.
Article27. Poggiali IV, Simoes E Silva AC, Vasconcelos MA, Dias CS, Gomes IR, Carvalho RA, et al. A clinical predictive model of renal injury in children with congenital solitary functioning kidney. Pediatr Nephrol. 2019; 34:465–74.
Article28. Groen In 't Woud S, Westland R, Feitz WF, Roeleveld N, van Wijk JA, van der Zanden LF, et al. Clinical management of children with a congenital solitary functioning kidney: overview and recommendations. Eur Urol Open Sci. 2021; 25:11–20.29. Westland R, Schreuder MF, van Goudoever JB, Sanna-Cherchi S, van Wijk JA. Clinical implications of the solitary functioning kidney. Clin J Am Soc Nephrol. 2014; 9:978–86.
Article30. Corbani V, Ghiggeri GM, Sanna-Cherchi S. ‘Congenital solitary functioning kidneys: which ones warrant follow-up into adult life?’. Nephrol Dial Transplant. 2011; 26:1458–60.
Article31. Friedman MA, Aguilar L, Heyward Q, Wheeler C, Caldamone A. Screening for Mullerian anomalies in patients with unilateral renal agenesis: leveraging early detection to prevent complications. J Pediatr Urol. 2018; 14:144–9.
Article32. Kenney PJ, Spirt BA, Leeson MD. Genitourinary anomalies: radiologic-anatomic correlations. Radiographics. 1984; 4:233–60.
Article33. Santos XM, Dietrich JE. Obstructed hemivagina with ipsilateral renal anomaly. J Pediatr Adolesc Gynecol. 2016; 29:7–10.
Article34. Semmens JP. Congenital anomalies of female genital tract: functional classification based on review of 56 personal cases and 500 reported cases. Obstet Gynecol. 1962; 19:328–50.35. Acien P. Embryological observations on the female genital tract. Hum Reprod. 1992; 7:437–45.36. Zurawin RK, Dietrich JE, Heard MJ, Edwards CL. Didelphic uterus and obstructed hemivagina with renal agenesis: case report and review of the literature. J Pediatr Adolesc Gynecol. 2004; 17:137–41.
Article37. Smith NA, Laufer MR. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil Steril. 2007; 87:918–22.
Article38. Heinonen PK. Pregnancies in women with uterine malformation, treated obstruction of hemivagina and ipsilateral renal agenesis. Arch Gynecol Obstet. 2013; 287:975–8.
Article39. Del Vescovo R, Pisanti F, Russo V, Battisti S, Cazzato RL, D'Agostino F, et al. Dynamic contrast-enhanced MR evaluation of prostate cancer before and after endorectal high-intensity focused ultrasound. Radiol Med. 2013; 118:851–62.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Congenital Solitary Pelvic Kidney
- Congenital Solitary Kidney Associated with Giant Hydronephrosis
- Renal growth slope in children with congenital and acquired solitary functioning kidneys
- Salvation of a solitary kidney in a patient with grade IV renal trauma: a case report
- Solitary Type of Congenital Self-healing Reticulohistiocytosis