Ann Dermatol.
2011 Sep;23(Suppl 1):S4-S7. 10.5021/ad.2011.23.S1.S4.
Solitary Type of Congenital Self-healing Reticulohistiocytosis
- Affiliations
-
- 1Department of Dermatology and Cutaneous Biology Research Institute, Yonsei University College of Medicine, Seoul, Korea. juhee@yuhs.ac
- KMID: 2156739
- DOI: http://doi.org/10.5021/ad.2011.23.S1.S4
Abstract
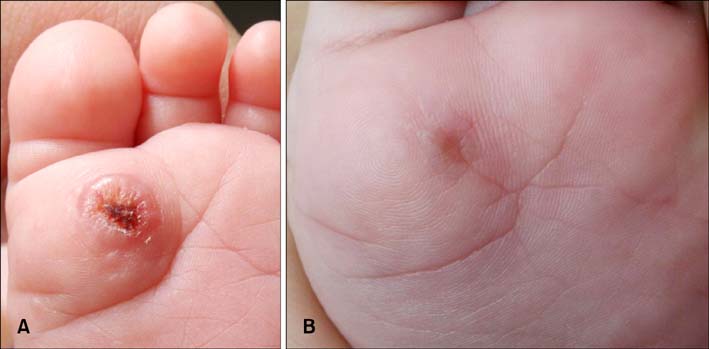
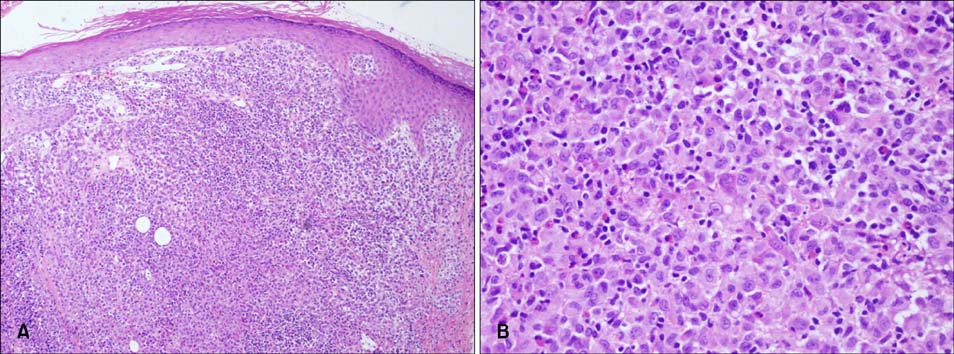
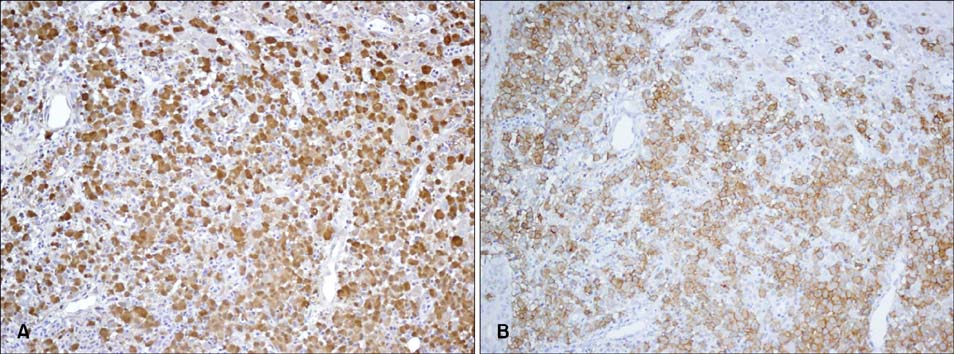
- Congenital self-healing reticulohistiocytosis is a rare, congenital, benign, self-healing variant of Langerhans cell histiocytosis. It usually appears as multiple papules or nodules; however, occurrence of the solitary type is very rare. We report on a case of solitary congenital self-healing reticulohistiocytosis in a 29-day-old girl who presented with a papule on her sole. Two months later, the lesion regressed with a slight scar. Based upon clinical and histologic findings, we made a diagnosis of solitary congenital self-healing reticulohistiocytosis. In this report, we summarized reported cases of solitary congenital self-healing retioculohistiocytosis in Korea with a review of the literature.
MeSH Terms
Figure
Cited by 1 articles
-
Solitary Congenital Erosion in a Newborn: Report of a Solitary Congenital Self-Healing Reticulohistiocytosis
Jung Eun Kim, Byung Jik Kim, Hoon Kang
Ann Dermatol. 2014;26(2):250-253. doi: 10.5021/ad.2014.26.2.250.
Reference
-
1. Hashimoto K, Pritzker MS. Electron microscopic study of reticulohistiocytoma. An unusual case of congenital, self-healing reticulohistiocytosis. Arch Dermatol. 1973. 107:263–270.
Article2. Chun SI, Song MS. Congenital self-healing reticulohistiocytosis-report of a case of the solitary type and review of the literature. Yonsei Med J. 1992. 33:194–198.
Article3. Shin MS, Park HJ, Choi YJ, Park MY. A case of solitary type of congenital self-healing reticulohistiocytosis. Korean J Dermatol. 2008. 46:411–413.4. Berger TG, Lane AT, Headington JT, Hartmann K, Burrish G, Levin MW, et al. A solitary variant of congenital self-healing reticulohistiocytosis: solitary Hashimoto-Pritzker disease. Pediatr Dermatol. 1986. 3:230–236.
Article5. Bernstein EF, Resnik KS, Loose JH, Halcin C, Kauh YC. Solitary congenital self-healing reticulohistiocytosis. Br J Dermatol. 1993. 129:449–454.
Article6. Kapur P, Erickson C, Rakheja D, Carder KR, Hoang MP. Congenital self-healing reticulohistiocytosis (Hashimoto-Pritzker disease): ten-year experience at Dallas children's medical center. J Am Acad Dermatol. 2007. 56:290–294.
Article7. Jang KA, Ahn SJ, Choi JH, Sung KJ, Moon KC, Koh JK. Histiocytic disorders with spontaneous regression in infancy. Pediatr Dermatol. 2000. 17:364–368.8. Higgins CR, Tatnall FM, Leigh IM. Vesicular Langerhans cell histiocytosis-an uncommon variant. Clin Exp Dermatol. 1994. 19:350–352.
Article9. Inuzuka M, Tomita K, Tokura Y, Takigawa M. Congenital self-healing reticulohistiocytosis presenting with hemorrhagic bullae. J Am Acad Dermatol. 2003. 48:5 Suppl. S75–S77.
Article10. Kanitakis J, Zambruno G, Schmitt D, Cambazard F, Jacquemier D, Thivolet J. Congenital self-healing histiocytosis (Hashimoto-Pritzker). An ultrastructural and immunohistochemical study. Cancer. 1988. 61:508–516.
Article11. Zunino-Goutorbe C, Eschard C, Durlach A, Bernard P. Congenital solitary histiocytoma: a variant of Hashimoto-Pritzker histiocytosis. A retrospective study of 8 cases. Dermatology. 2008. 216:118–124.
Article12. Zwerdling T, Konia T, Silverstein M. Congenital, single system, single site, Langerhans cell histiocytosis: a new case, observations from the literature, and management considerations. Pediatr Dermatol. 2009. 26:121–126.
Article13. Saijo S, Hara M, Kuramoto Y, Tagami H. Generalized eruptive histiocytoma: a report of a variant case showing the presence of dermal indeterminate cells. J Cutan Pathol. 1991. 18:134–136.
Article14. Willman CL, Busque L, Griffith BB, Favara BE, McClain KL, Duncan MH, et al. Langerhans'-cell histiocytosis (histiocytosis X)-a clonal proliferative disease. N Engl J Med. 1994. 331:154–160.
Article15. Sidoroff A, Zelger B, Steiner H, Smith N. Indeterminate cell histiocytosis--a clinicopathological entity with features of both X- and non-X histiocytosis. Br J Dermatol. 1996. 134:525–532.
Article16. Weiss T, Weber L, Scharffetter-Kochanek K, Weiss JM. Solitary cutaneous dendritic cell tumor in a child: role of dendritic cell markers for the diagnosis of skin Langerhans cell histiocytosis. J Am Acad Dermatol. 2005. 53:838–844.
Article17. Valladeau J, Duvert-Frances V, Pin JJ, Dezutter-Dambuyant C, Vincent C, Massacrier C, et al. The monoclonal antibody DCGM4 recognizes Langerin, a protein specific of Langerhans cells, and is rapidly internalized from the cell surface. Eur J Immunol. 1999. 29:2695–2704.
Article18. Geissmann F, Lepelletier Y, Fraitag S, Valladeau J, Bodemer C, Debré M, et al. Differentiation of Langerhans cells in Langerhans cell histiocytosis. Blood. 2001. 97:1241–1248.
Article19. Esterly NB, Maurer HS, Gonzalez-Crussi F. Histiocytosis X: a seven-year experience at a children's hospital. J Am Acad Dermatol. 1985. 13:481–496.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Congenital self-healing reticulohistiocytosis: report of a case of the solitary type and review of the literature
- A Case of a Solitary Type of Congenital Self-healing Reticulohistiocytosis
- Congenital self-healing Reticulohistiocytosis
- Solitary Congenital Erosion in a Newborn: Report of a Solitary Congenital Self-Healing Reticulohistiocytosis
- A Case of Congenital Self-Healing Reticulohistiocytosis Presenting as Erythematous Erosive Patches and Vesicles