Cardiovasc Prev Pharmacother.
2024 Oct;6(4):103-108. 10.36011/cpp.2024.6.e16.
Sodium-glucose cotransporter 2 inhibitors in cardiocerebrovascular disease
- Affiliations
-
- 1Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- KMID: 2560381
- DOI: http://doi.org/10.36011/cpp.2024.6.e16
Abstract
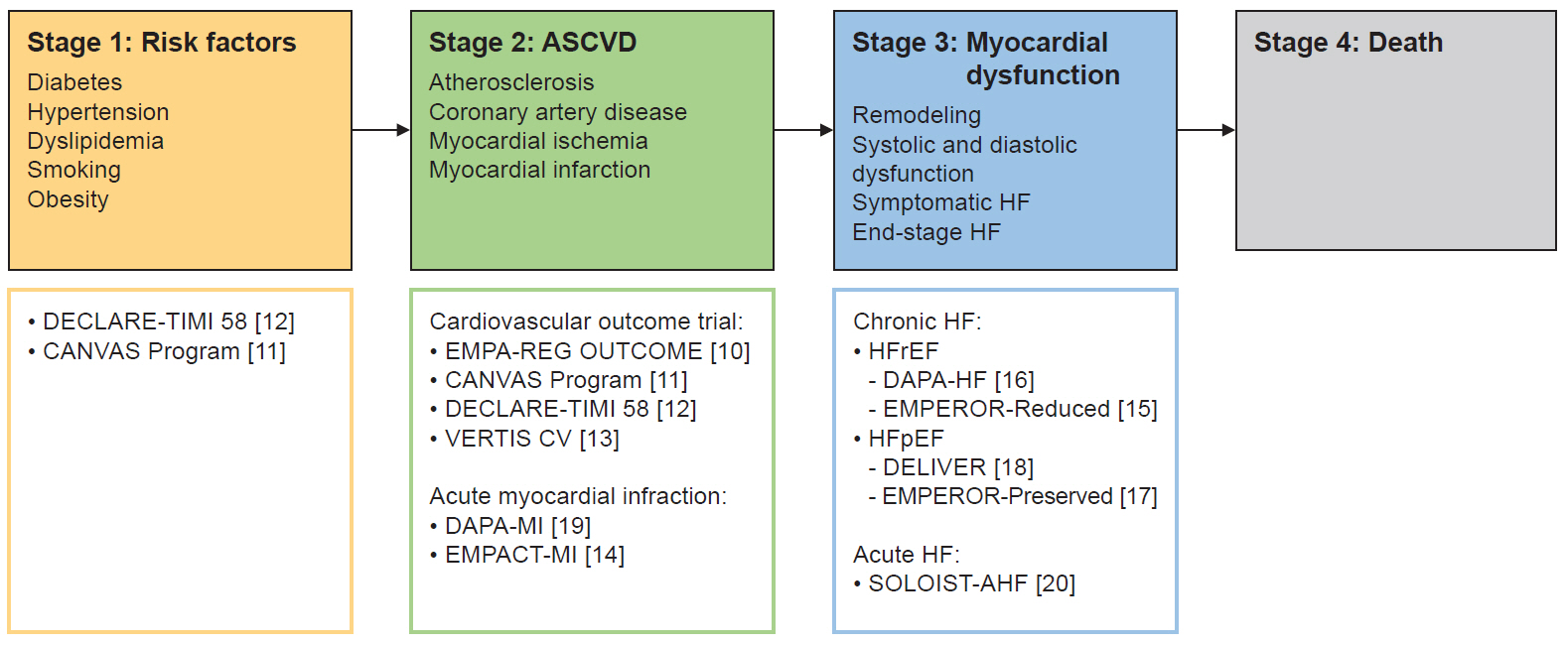
- Cardiovascular disease is a leading cause of global mortality, necessitating effective strategies for prevention and treatment. The cardiovascular disease continuum concept highlights the progression from risk factors such as hypertension and diabetes mellitus to advanced stages, including heart failure (HF) and death. Sodium-glucose cotransporter 2 (SGLT2) inhibitors, initially developed to manage diabetes, have emerged as effective therapies across all stages of the cardiovascular disease continuum. Numerous cardiovascular outcome trials demonstrate that SGLT2 inhibitors significantly reduce major adverse cardiovascular events and hospitalizations for HF in patients with and without established atherosclerotic cardiovascular disease. Notably, SGLT2 inhibitors have shown remarkable benefits in reducing HF risk, even in patients without diabetes, including those with HF and preserved ejection fraction. Furthermore, recent studies in post–myocardial infarction patients suggest potential benefits in reducing hospitalizations for HF. Despite their widespread use, the precise mechanisms by which SGLT2 inhibitors confer cardiovascular protection remain unclear, suggesting the need for further investigation. In conclusion, SGLT2 inhibitors have revolutionized cardiovascular disease management, offering significant therapeutic potential across a broad spectrum of patients, and are expected to play an increasingly prominent role in both the prevention and treatment of cardiovascular disease.
Keyword
Figure
Reference
-
1. Dzau VJ, Antman EM, Black HR, Hayes DL, Manson JE, Plutzky J, et al. The cardiovascular disease continuum validated: clinical evidence of improved patient outcomes: part I: Pathophysiology and clinical trial evidence (risk factors through stable coronary artery disease). Circulation. 2006; 114:2850–70.
Article2. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022; 79:e263–421.3. Park JJ. Epidemiology, pathophysiology, diagnosis and treatment of heart failure in diabetes. Diabetes Metab J. 2021; 45:146–57.
Article4. Lee KS, Noh J, Park SM, Choi KM, Kang SM, Won KC, et al. Evaluation and management of patients with diabetes and heart failure: a Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement. Int J Heart Fail. 2023; 5:1–20.
Article5. Lee HY. Heart failure and diabetes mellitus: dangerous liaisons. Int J Heart Fail. 2022; 4:163–74.
Article6. Lee CJ, Lee H, Yoon M, Chun KH, Kong MG, Jung MH, et al. Heart failure statistics 2024 update: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2024; 6:56–69.
Article7. Choi JH, Lee KA, Moon JH, Chon S, Kim DJ, Kim HJ, et al. 2023 Clinical practice guidelines for diabetes mellitus of the Korean Diabetes Association. Diabetes Metab J. 2023; 47:575–94.
Article8. Control Group, Turnbull FM, Abraira C, Anderson RJ, Byington RP, Chalmers JP, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia. 2009; 52:2288–98.
Article9. Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007; 356:2457–71.
Article10. Zinman B, Lachin JM, Inzucchi SE. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2016; 374:1094.
Article11. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017; 377:644–57.
Article12. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019; 380:347–57.
Article13. Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020; 383:1425–35.
Article14. Butler J, Jones WS, Udell JA, Anker SD, Petrie MC, Harrington J, et al. Empagliflozin after Acute Myocardial Infarction. N Engl J Med. 2024; 390:1455–66.15. Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020; 383:1413–24.16. McMurray JJ, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019; 381:1995–2008.17. Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Bohm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021; 385:1451–61.18. Solomon SD, Vaduganathan M, Claggett BL, de Boer RA, DeMets D, Hernandez AF, et al. Baseline characteristics of patients with HF with mildly reduced and preserved ejection fraction: DELIVER trial. JACC Heart Fail. 2022; 10:184–97.19. James S, Erlinge D, Storey RF, McGuire DK, de Belder M, Eriksson N, et al. Dapagliflozin in myocardial infarction without diabetes or heart failure. NEJM Evid. 2024; 3:EVIDoa2300286.
Article20. Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med. 2021; 384:117–128.
Article21. Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019; 393:31–9.
Article22. Youn JC, Kim D, Cho JY, Cho DH, Park SM, Jung MH, et al. Korean Society of Heart Failure guidelines for the management of heart failure: treatment. Int J Heart Fail. 2023; 5:66–81.
Article23. Cho JY, Cho DH, Youn JC, Kim D, Park SM, Jung MH, et al. Korean Society of Heart Failure guidelines for the management of heart failure: definition and diagnosis. Int J Heart Fail. 2023; 5:51–65.
Article24. SOLVD Investigators, Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991; 325:293–302.
Article25. McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371:993–1004.
Article26. Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med. 1996; 334:1349–55.
Article27. Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999; 341:709–17.
Article28. Yoo BS. President’s message: 4 pillars of Korean Society of Heart Failure. Int J Heart Fail. 2024; 6:117–8.
Article29. Park SM, Lee SY, Jung MH, Youn JC, Kim D, Cho JY, et al. Korean Society of Heart Failure guidelines for the management of heart failure: management of the underlying etiologies and comorbidities of heart failure. Int J Heart Fail. 2023; 5:127–45.
Article30. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2023 Focused update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023; 44:3627–39.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- SGLT2 Inhibitors and Ketoacidosis: Pathophysiology and Management
- The Side Effects of Sodium Glucose Cotransporter 2 (SGLT2) Inhibitor
- Emerging Safety Issues of Dipeptidyl Peptidase-4 Inhibitors and Sodium Glucose Cotransporter 2 Inhibitors: How to Interpret and Apply in Clinical Practice
- Sodium-Glucose Cotransporter 2 Inhibitors for People with Type 1 Diabetes
- Glucose Lowering Effect of SGLT2 Inhibitors: A Review of Clinical Studies