Endocrinol Metab.
2024 Oct;39(5):813-818. 10.3803/EnM.2024.2014.
Impact of Diabetes on COVID-19 Susceptibility: A Nationwide Propensity Score Matching Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Sungkyunkwan University School of Medicine, Suwon, Korea
- 3Department of Biostatistics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- KMID: 2560289
- DOI: http://doi.org/10.3803/EnM.2024.2014
Abstract
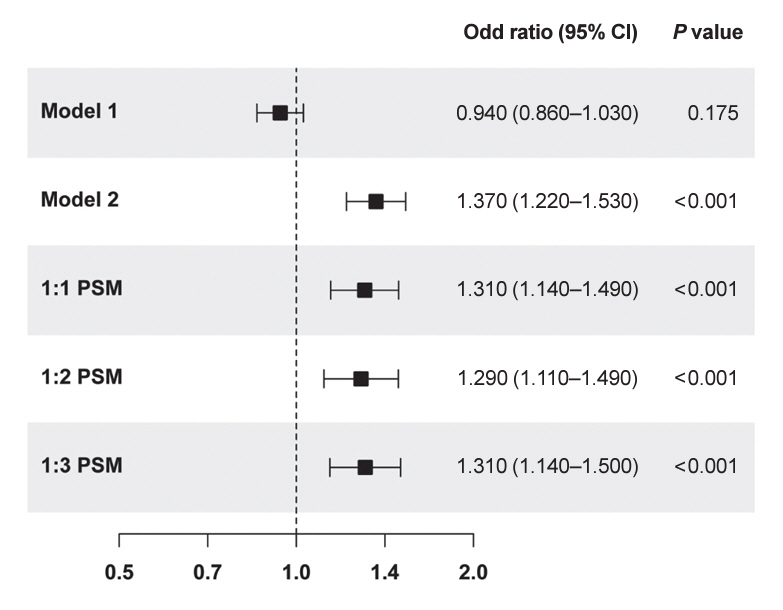
- Prior research has highlighted poor clinical outcomes in coronavirus disease 2019 (COVID-19)-infected patients with diabetes; however, susceptibility to COVID-19 infection in patients with diabetes has not been extensively studied. Participants aged ≥30 years who underwent COVID-19 testing from December 2019 to April 2020 were analyzed using the National Health Insurance Service data in South Korea. In a cohort comprising 29,433 1:1 propensity score-matched participants, COVID-19 positivity was significantly higher in participants with diabetes than in those without diabetes (512 [3.5%] vs. 395 [2.7%], P<0.001). Logistic regression analysis indicated that diabetes significantly increased the risk of COVID-19 test positivity (odds ratio, 1.307; 95% confidence interval, 1.144 to 1.493; P<0.001). Patients with diabetes exhibited heightened COVID-19 infection rates compared to individuals without diabetes, and diabetes increased the susceptibility to COVID-19, reinforcing the need for heightened preventive measures, particularly considering the poor clinical outcomes in this group.
Keyword
Figure
Reference
-
1. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020; 395:565–74.
Article2. World Health Organization. COVID-19 weekly epidemiological update, edition 141, 4 May 2023 [Internet]. Geneva: WHO;2023. [cited 2024 Jun 17]. Available from: https://iris.who.int/handle/10665/367666.3. Hartantri Y, Debora J, Widyatmoko L, Giwangkancana G, Suryadinata H, Susandi E, et al. Clinical and treatment factors associated with the mortality of COVID-19 patients admitted to a referral hospital in Indonesia. Lancet Reg Health Southeast Asia. 2023; 11:100167.
Article4. Moon SJ, Rhee EJ, Jung JH, Han KD, Kim SR, Lee WY, et al. Independent impact of diabetes on the severity of coronavirus disease 2019 in 5,307 patients in South Korea: a nationwide cohort study. Diabetes Metab J. 2020; 44:737–46.
Article5. Lechien JR, Chiesa-Estomba CM, Place S, Van Laethem Y, Cabaraux P, Mat Q, et al. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 2020; 288:335–44.
Article6. Gold JA, Wong KK, Szablewski CM, Patel PR, Rossow J, da Silva J, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19: Georgia, March 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:545–50.7. Kang D, Choi J, Kim Y, Kwon D. An analysis of the dynamic spatial spread of COVID-19 across South Korea. Sci Rep. 2022; 12:9364.
Article8. Chun SY, Kim DW, Lee SA, Lee SJ, Chang JH, Choi YJ, et al. Does diabetes increase the risk of contracting COVID-19?: a population-based study in Korea. Diabetes Metab J. 2020; 44:897–907.
Article9. Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr Diabetes Rev. 2020; 16:442–9.
Article10. Mooradian AD, Reed RL, Meredith KE, Scuderi P. Serum levels of tumor necrosis factor and IL-1 alpha and IL-1 beta in diabetic patients. Diabetes Care. 1991; 14:63–5.11. Tanaka T, Narazaki M, Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol. 2014; 6:a016295.
Article12. Martinez N, Ketheesan N, Martens GW, West K, Lien E, Kornfeld H. Defects in early cell recruitment contribute to the increased susceptibility to respiratory Klebsiella pneumoniae infection in diabetic mice. Microbes Infect. 2016; 18:649–55.
Article13. Stegenga ME, van der Crabben SN, Blumer RM, Levi M, Meijers JC, Serlie MJ, et al. Hyperglycemia enhances coagulation and reduces neutrophil degranulation, whereas hyperinsulinemia inhibits fibrinolysis during human endotoxemia. Blood. 2008; 112:82–9.
Article14. Berrou J, Fougeray S, Venot M, Chardiny V, Gautier JF, Dulphy N, et al. Natural killer cell function, an important target for infection and tumor protection, is impaired in type 2 diabetes. PLoS One. 2013; 8:e62418.
Article15. Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003; 426:450–4.
Article16. Roca-Ho H, Riera M, Palau V, Pascual J, Soler MJ. Characterization of ACE and ACE2 expression within different organs of the NOD mouse. Int J Mol Sci. 2017; 18:563.
Article17. Romani-Perez M, Outeirino-Iglesias V, Moya CM, Santisteban P, Gonzalez-Matias LC, Vigo E, et al. Activation of the GLP-1 receptor by liraglutide increases ACE2 expression, reversing right ventricle hypertrophy, and improving the production of SP-A and SP-B in the lungs of type 1 diabetes rats. Endocrinology. 2015; 156:3559–69.
Article18. Zhang W, Li C, Liu B, Wu R, Zou N, Xu YZ, et al. Pioglitazone upregulates hepatic angiotensin converting enzyme 2 expression in rats with steatohepatitis. Ann Hepatol. 2013; 12:892–900.
Article19. Kriszta G, Kriszta Z, Vancsa S, Hegyi PJ, Frim L, Eross B, et al. Effects of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers on angiotensin-converting enzyme 2 levels: a comprehensive analysis based on animal studies. Front Pharmacol. 2021; 12:619524.
Article20. Hartmann-Boyce J, Rees K, Perring JC, Kerneis SA, Morris EM, Goyder C, et al. Risks of and from SARS-CoV-2 infection and COVID-19 in people with diabetes: a systematic review of reviews. Diabetes Care. 2021; 44:2790–811.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19 infection and severe clinical outcomes in patients with kidney disease by vaccination status: a nationwide cohort study in Korea
- Relationship between the Geriatric Nutrition Risk Index and the Prognosis of Severe Coronavirus Disease 2019 in Korea
- Impact of solid organ transplantation on the effectiveness of COVID-19 vaccination in hospitalized patients with COVID-19: a propensity score-matched cohort study
- Impact of COVID-19 infection during the postoperative period in patients who underwent gastrointestinal surgery: a retrospective study
- Impact of Dementia on Mortality Due to Coronavirus Disease 2019: Propensity-Score-Matching Study