Ann Surg Treat Res.
2024 Oct;107(4):212-220. 10.4174/astr.2024.107.4.212.
Optimal withdrawal time in initial surveillance colonoscopy after colorectal cancer surgery: comparison between anterior/low anterior resection and right hemicolectomy
- Affiliations
-
- 1Department of Surgery, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2560006
- DOI: http://doi.org/10.4174/astr.2024.107.4.212
Abstract
- Purpose
This study aimed to investigate the optimal withdrawal time (WT) for initial surveillance colonoscopy after curative resection for colorectal cancer (CRC) by comparing anterior/low anterior resection (AR/LAR) and right hemicolectomy (RHC) groups.
Methods
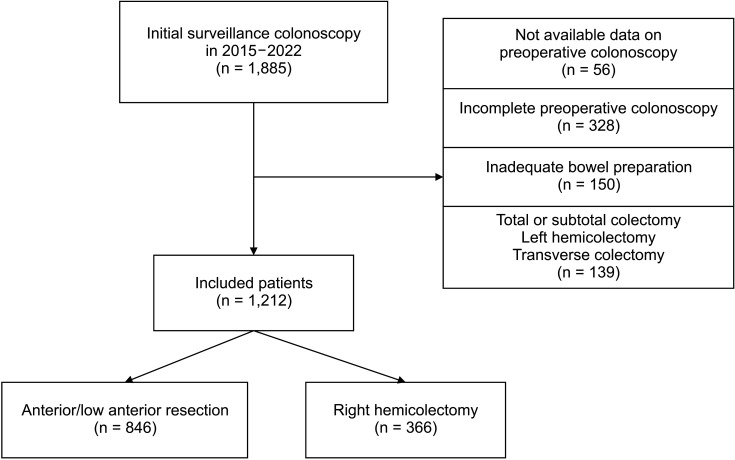
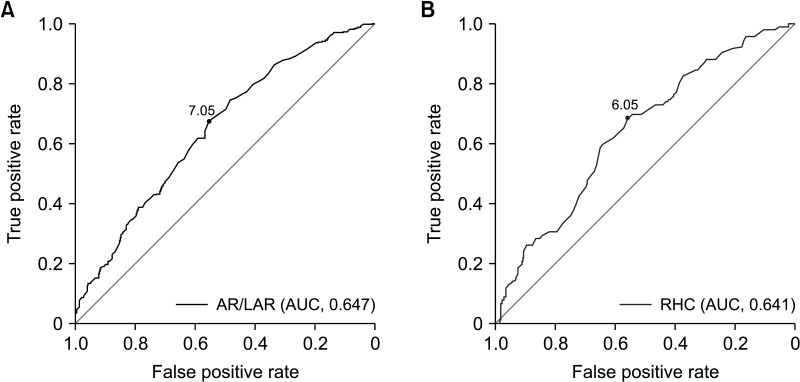
This retrospective study analyzed 1,212 patients who underwent initial surveillance colonoscopy after CRC resection between 2015 and 2022. The patients were divided into the AR/LAR (n = 846) and RHC (n = 366) groups. The optimal WT was determined using receiver operating characteristic curve analysis and validated using logistic regression models. The adenoma and advanced neoplasia detection rates (ADR/ANDR) were evaluated based on the optimal WT.
Results
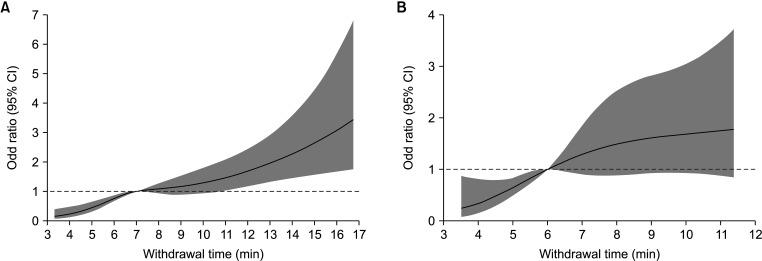
The optimal WT was 7 and 6 minutes in the AR/LAR and RHC groups, respectively. In multivariate analysis, WT ≥7 and ≥6 minutes in the AR/LAR (odds ratio [OR], 2.38; 95% confidence interval [CI], 1.75–3.24; P < 0.001) and RHC (OR, 2.64; 95% CI, 1.59–4.39; P = 0.001) groups, respectively, were significant factors for adenoma detection. In the AR/LAR group, ADR was 41.5% for WT ≥7 minutes compared to 21.9% for WT <7 minutes (P < 0.001). In the RHC group, ADR for WT ≥6 minutes was 33.9% compared to 15.8% for WT <6 minutes (P < 0.001). The ANDR also significantly improved with longer WTs in both groups.
Conclusion
This study suggests that a minimum WT of 7 and 6 minutes for AR/LAR and RHC patients, respectively, during the initial surveillance colonoscopy after CRC resection is optimal for maintaining a satisfactory ADR and ANDR. These findings highlight the importance of tailoring colonoscopic procedures according to the type of surgical resection.
Keyword
Figure
Reference
-
1. Baik SM, Lee RA. National cancer screening program for colorectal cancer in Korea. Ann Surg Treat Res. 2023; 105:333–340. PMID: 38076601.
Article2. Lautenbach E, Forde KA, Neugut AI. Benefits of colonoscopic surveillance after curative resection of colorectal cancer. Ann Surg. 1994; 220:206–211. PMID: 8053743.3. Fuccio L, Rex D, Ponchon T, Frazzoni L, Dinis-Ribeiro M, Bhandari P, et al. New and recurrent colorectal cancers after resection: a systematic review and metaanalysis of endoscopic surveillance studies. Gastroenterology. 2019; 156:1309–1323. PMID: 30553914.
Article4. Kahi CJ, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, et al. Colonoscopy surveillance after colorectal cancer resection: recommendations of the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2016; 111:337–346. PMID: 26871541.
Article5. Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006; 355:2533–2541. PMID: 17167136.
Article6. Petrelli F, Tomasello G, Borgonovo K, Ghidini M, Turati L, Dallera P, et al. Prognostic survival associated with left-sided vs right-sided colon cancer: a systematic review and meta-analysis. JAMA Oncol. 2017; 3:211–219. PMID: 27787550.7. Yang JF, Noffsinger AE, Agrawal D, Yang QH. Colorectal cancer anatomic distribution patterns remain the same after sessile serrated adenoma/polyp considered cancer precursor: a 9-year comparison study from community-based endoscopy centers. J Gastrointest Oncol. 2016; 7:917–923. PMID: 28078114.
Article8. Shin R, Lee S, Han KS, Sohn DK, Moon SH, Choi DH, et al. Guidelines for accreditation of endoscopy units: quality measures from the Korean Society of Coloproctology. Ann Surg Treat Res. 2021; 100:154–165. PMID: 33748029.
Article9. Aziz M, Haghbin H, Gangwani MK, Nawras M, Nawras Y, Dahiya DS, et al. 9-Minute withdrawal time improves adenoma detection rate compared with 6-minute withdrawal time during colonoscopy: a meta-analysis of randomized controlled trials. J Clin Gastroenterol. 2023; 57:863–870. PMID: 37389958.
Article10. Zhao M, Xu Y, Zhu H, Chen J, Sun W, Yang D, et al. A prospective cohort study of the relationship between the withdrawal time and the detection rate of colorectal adenoma. Scand J Gastroenterol. 2022; 57:1131–1137. PMID: 35465795.11. Rusiecki J, Cifu AS. Colonoscopy surveillance after colorectal cancer resection. JAMA. 2017; 318:2346–2347. PMID: 29260211.
Article12. le Clercq CM, Winkens B, Bakker CM, Keulen ET, Beets GL, Masclee AA, et al. Metachronous colorectal cancers result from missed lesions and non-compliance with surveillance. Gastrointest Endosc. 2015; 82:325–333. PMID: 25843613.
Article13. Jung DH, Lee JI, Huh CW, Kim MJ, Youn YH, Choi YH, et al. Withdrawal time of 8 minutes is associated with higher adenoma detection rates in surveillance colonoscopy after surgery for colorectal cancer. Surg Endosc. 2021; 35:2354–2361. PMID: 32440929.
Article14. Bostanci MT, Yilmaz I. Surgical resection length and harvested lymph nodes in colon cancer. J Coll Physicians Surg Pak. 2021; 31:798–804. PMID: 34271779.15. Üstüner MA, Aksel B, Dogan L. The minimum length of colonic segment to be removed for adequate lymph node dissection in colorectal cancer. Hellenic J Surg. 2020; 92:110–114.
Article16. Gupta S, Balasubramanian BA, Fu T, Genta RM, Rockey DC, Lash R. Polyps with advanced neoplasia are smaller in the right than in the left colon: implications for colorectal cancer screening. Clin Gastroenterol Hepatol. 2012; 10:1395–1401. PMID: 22835574.
Article17. Montgomery E. Serrated colorectal polyps: emerging evidence suggests the need for a reappraisal. Adv Anat Pathol. 2004; 11:143–149. PMID: 15096728.18. Bartolí R, Boix J, Odena G, De la Ossa ND, de Vega VM, Lorenzo-Zúñiga V. Colonoscopy in rats: an endoscopic, histological and tomographic study. World J Gastrointest Endosc. 2013; 5:226–230. PMID: 23678375.19. Heldwein W, Dollhopf M, Rösch T, Meining A, Schmidtsdorff G, Hasford J, et al. The Munich Polypectomy Study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy. 2005; 37:1116–1122. PMID: 16281142.
Article20. Maratt JK, Dickens J, Schoenfeld PS, Elta GH, Jackson K, Rizk D, et al. Factors associated with surveillance adenoma and sessile serrated polyp detection rates. Dig Dis Sci. 2017; 62:3579–3585. PMID: 29043592.
Article21. Mitsuhashi S, Azari J, Dioguardi V, Bilello J, Tang M, Kastenberg D. Age matters: adenoma detection rates in average-risk screening patients aged 45 to 49 compared with those aged 50 to 54. J Clin Gastroenterol. 2024; 58:896–901. PMID: 38059772.22. Zhou W, Yao L, Wu H, Zheng B, Hu S, Zhang L, et al. Multi-step validation of a deep learning-based system for the quantification of bowel preparation: a prospective, observational study. Lancet Digit Health. 2021; 3:e697–e706. PMID: 34538736.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal Colonoscopy Surveillance Interval after Polypectomy
- Comparison of Colonoscopy Surveillance Outcomes Between Young and Older Colorectal Cancer Patients
- Post-colonoscopy Colorectal Cancer: Causes and Prevention of Interval Colorectal Cancer
- Colorectal Cancer after Colonoscopy: Causes and Prevention Strategies
- Surveillance Colonoscopy After a Resection of Colorectal Cancer