Korean J Orthod.
2024 Sep;54(5):303-315. 10.4041/kjod23.112.
Effectiveness of autologous leukocyte–platelet-rich fibrin on the rate of maxillary canine retraction, rotation, pain, and soft tissue healing: A split-mouth randomized controlled trial
- Affiliations
-
- 1Department of Orthodontics and Dentofacial Orthopaedics, SCB Dental College and Hospital, Cuttack, India
- 2Department of Periodontics and Oral Implantology, SCB Dental College and Hospital, Cuttack, India
- KMID: 2559819
- DOI: http://doi.org/10.4041/kjod23.112
Abstract
Objective
To assess the effectiveness of leukocyte–platelet-rich fibrin (L-PRF) compared with conventional treatment on canine retraction, rotation, pain, and soft tissue healing.
Methods
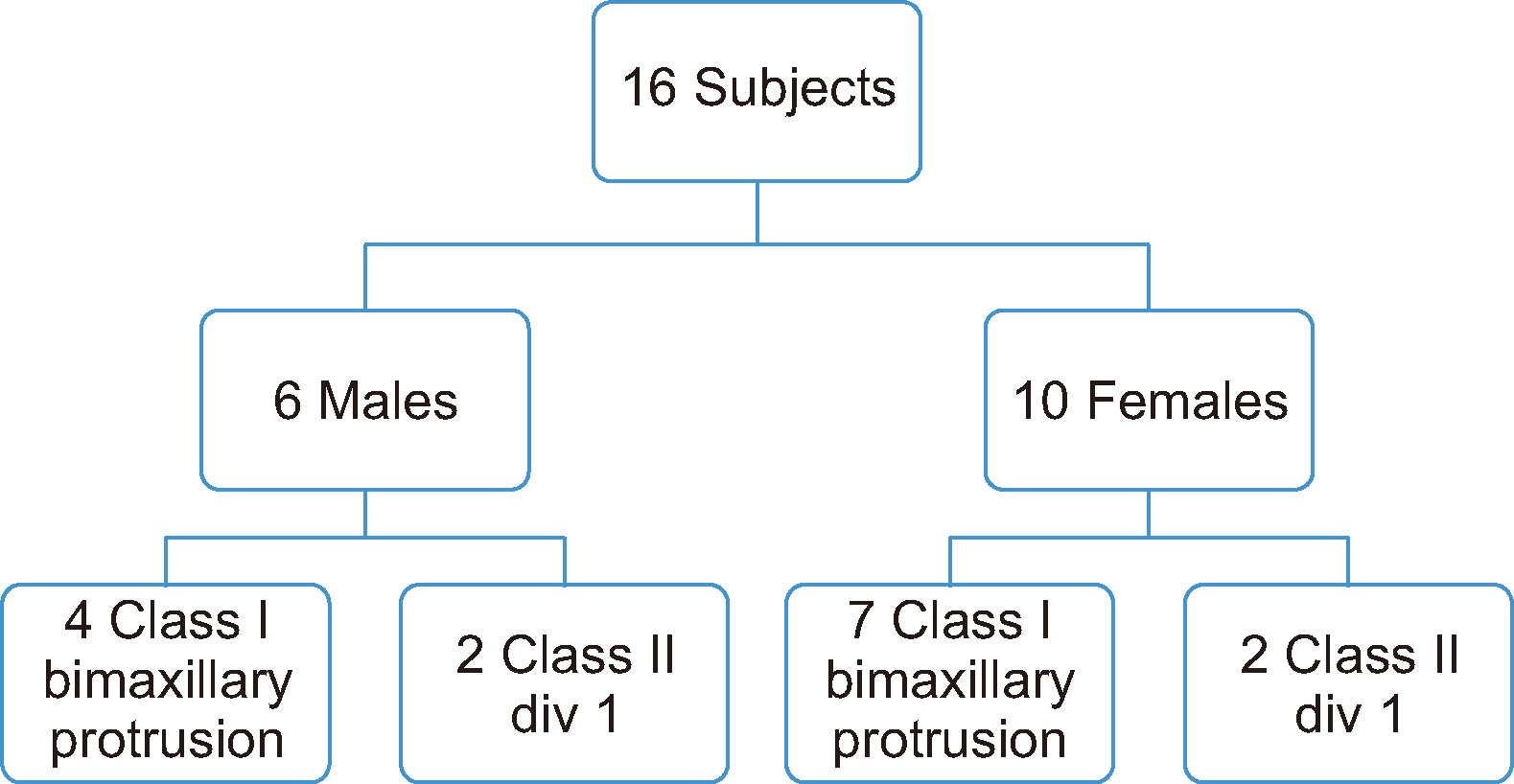
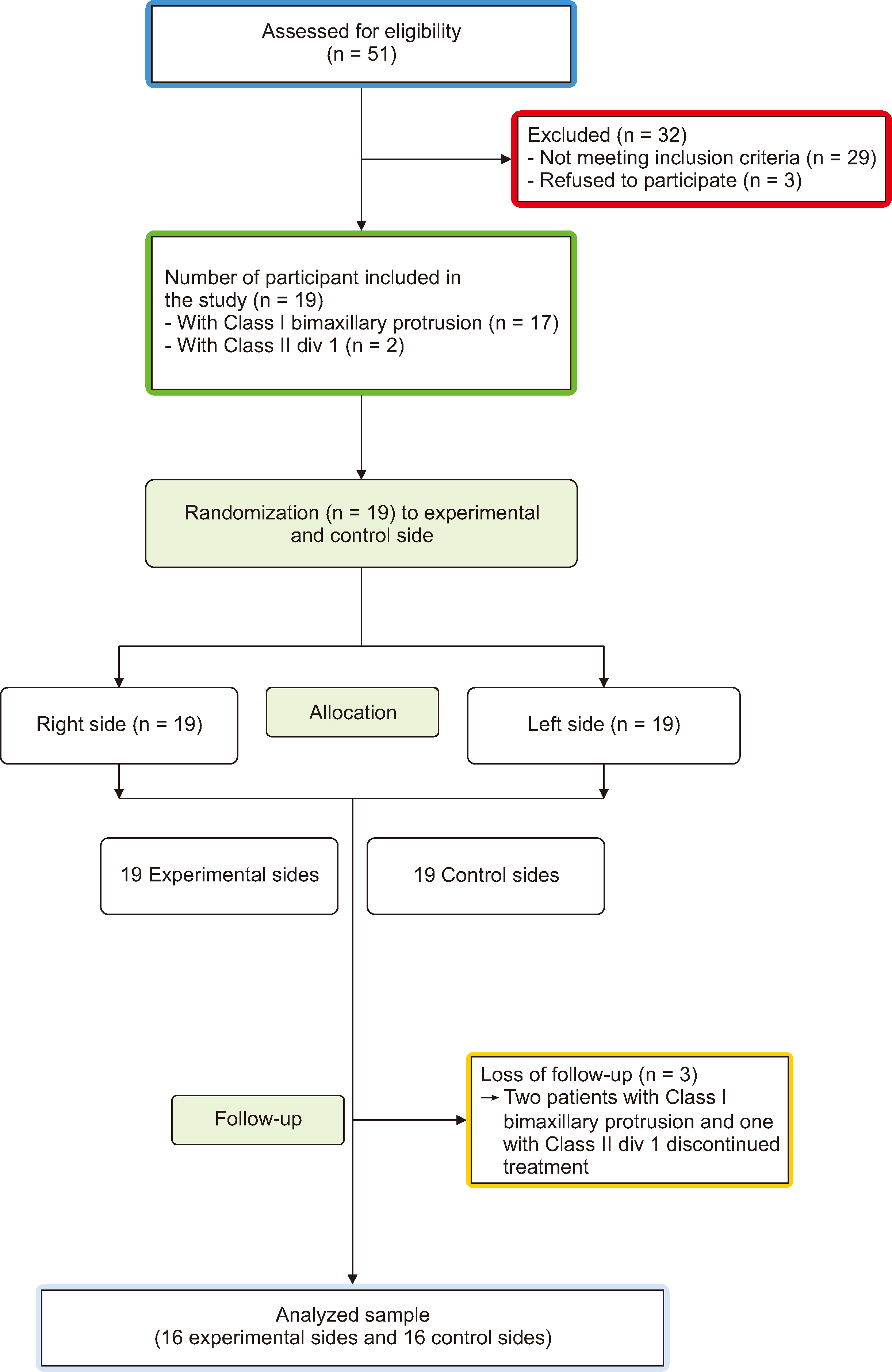
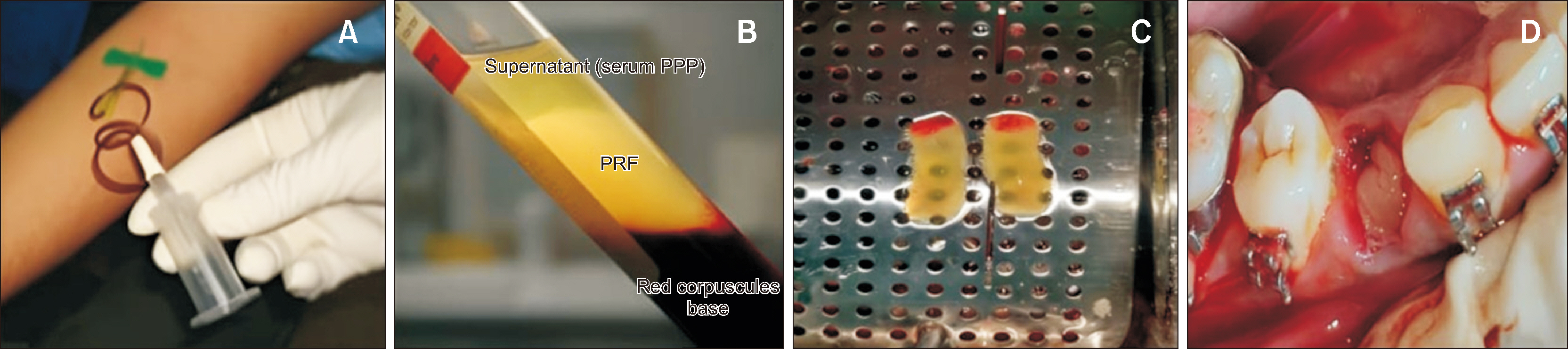
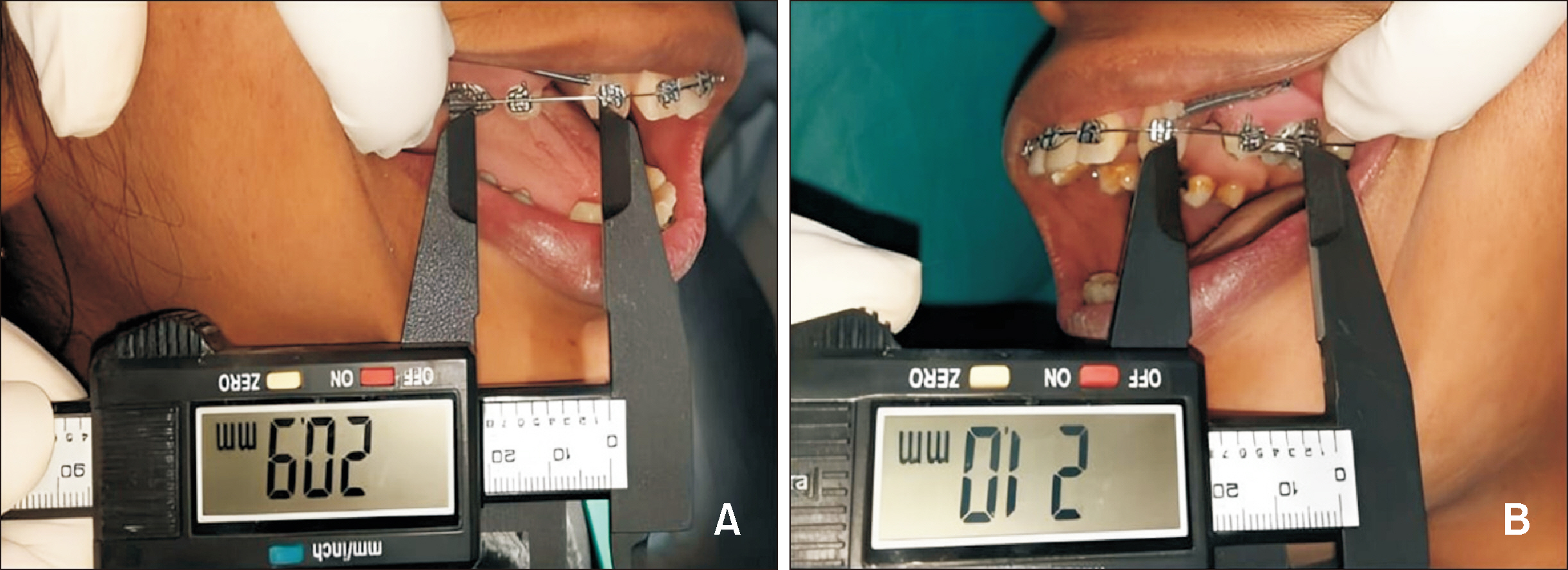
Sixteen adult patients aged 18–25 years (10 females, and 6 males; mean age 22.25 ± 2.26 years) with Class I bimaxillary protrusion and Class II div 1 malocclusion participated in this single-center, split-mouth randomized controlled trial at the Orthodontics Department of a single hospital in SCB Dental College and Hospital, Cuttack, India. Randomization was performed using a computer-assisted function with a 1:1 allocation ratio. The intervention included the placement of L-PRF on the experimental side and follow-up for 90 days. The primary outcome measures were canine retraction, rotation, pain, and soft tissue healing. The range of tooth movement was evaluated at 15-day intervals: 0th day (T0), 15th day (T1), 30th day (T2), 45th day (T3), 60th day (T4), 75th day (T5), and 90th day (T6). Canine rotation was assessed at T0 and T6, and pain and soft tissue healing were evaluated on the 3rd, 7th, and 15th days of the treatment.
Results
Cumulatively, the L-PRF group demonstrated a significantly greater tooth movement as compared to conventional treatment group (P < 0.001). Overall, canine retraction was 1.5 times greater on the L-PRF side than on the control side. Canine rotation showed no significant relationship, whereas pain and soft tissue healing were significantly better on the L-PRF side than on the control side.
Conclusions
Local administration of L-PRF amplifies canine retraction while improving pain and soft tissue repair.
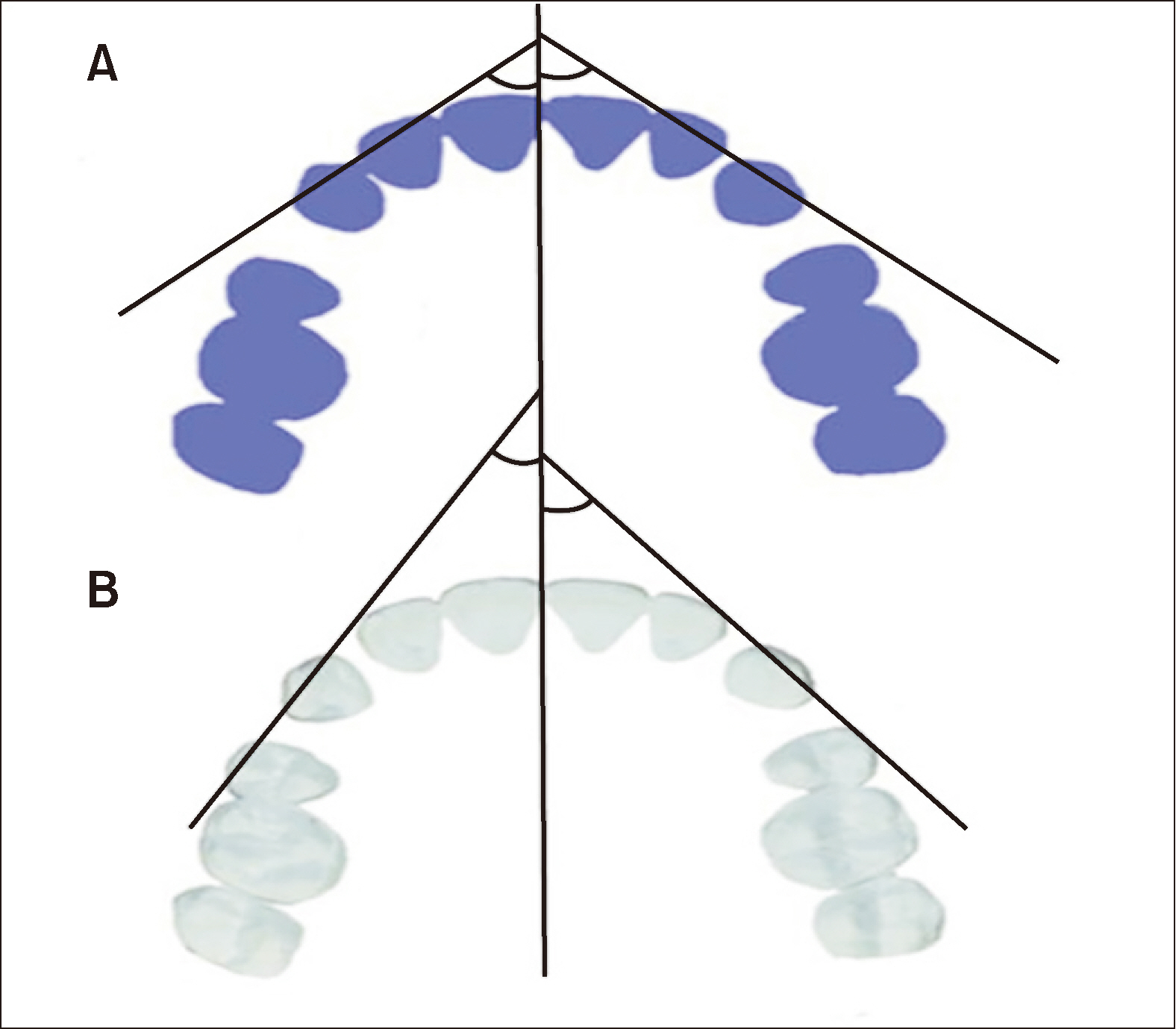
Figure
Reference
-
1. Segal GR, Schiffman PH, Tuncay OC. 2004; Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofac Res. 7:71–8. https://doi.org/10.1111/j.1601-6343.2004.00286.x. DOI: 10.1111/j.1601-6343.2004.00286.x.2. Teixeira CC, Khoo E, Tran J, Chartres I, Liu Y, Thant LM, et al. 2010; Cytokine expression and accelerated tooth movement. J Dent Res. 89:1135–41. https://doi.org/10.1177/0022034510373764. DOI: 10.1177/0022034510373764. PMID: 20639508. PMCID: PMC3318047.3. Andrade I Jr, Taddei SRA, Souza PEA. 2012; Inflammation and tooth movement: the role of cytokines, chemokines, and growth factors. Semin Orthod. 18:257–69. https://doi.org/10.1053/j.sodo.2012.06.004. DOI: 10.1053/j.sodo.2012.06.004.4. Nishimura M, Chiba M, Ohashi T, Sato M, Shimizu Y, Igarashi K, et al. 2008; Periodontal tissue activation by vibration: intermittent stimulation by resonance vibration accelerates experimental tooth movement in rats. Am J Orthod Dentofacial Orthop. 133:572–83. https://doi.org/10.1016/j.ajodo.2006.01.046. DOI: 10.1016/j.ajodo.2006.01.046. PMID: 18405822.5. Wilcko MT, Wilcko WM, Bissada NF. 2008; An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: a synthesis of scientific perspectives. Semin Orthod. 14:305–16. https://doi.org/10.1053/j.sodo.2008.07.007. DOI: 10.1053/j.sodo.2008.07.007.6. Güleç A, Bakkalbaşı BÇ, Cumbul A, Uslu Ü, Alev B, Yarat A. 2017; Effects of local platelet-rich plasma injection on the rate of orthodontic tooth movement in a rat model: a histomorphometric study. Am J Orthod Dentofacial Orthop. 151:92–104. https://doi.org/10.1016/j.ajodo.2016.05.016. DOI: 10.1016/j.ajodo.2016.05.016.7. Rashid A, ElSharaby FA, Nassef EM, Mehanni S, Mostafa YA. 2017; Effect of platelet-rich plasma on orthodontic tooth movement in dogs. Orthod Craniofac Res. 20:102–10. https://doi.org/10.1111/ocr.12146. DOI: 10.1111/ocr.12146.8. Del Corso M, Vervelle A, Simonpieri A, Jimbo R, Inchingolo F, Sammartino G, et al. 2012; Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 1: periodontal and dentoalveolar surgery. Curr Pharm Biotechnol. 13:1207–30. https://doi.org/10.2174/138920112800624391. DOI: 10.2174/138920112800624391.9. Yuan T, Guo SC, Han P, Zhang CQ, Zeng BF. 2012; Applications of leukocyte- and platelet-rich plasma (L-PRP) in trauma surgery. Curr Pharm Biotechnol. 13:1173–84. 20112800624445. DOI: 10.2174/138920112800624445. PMID: 21740374.10. Schär MO, Diaz-Romero J, Kohl S, Zumstein MA, Nesic D. 2015; Platelet-rich concentrates differentially release growth factors and induce cell migration in vitro. Clin Orthop Relat Res. 473:1635–43. https://doi.org/10.1007/s11999-015-4192-2. DOI: 10.1007/s11999-015-4192-2. PMID: 25690170. PMCID: PMC4385378.11. Anitua E, Zalduendo M, Troya M, Padilla S, Orive G. 2015; Leukocyte inclusion within a platelet rich plasma-derived fibrin scaffold stimulates a more pro-inflammatory environment and alters fibrin properties. PLoS One. 10:e0121713. https://doi.org/10.1371/journal.pone.0121713. DOI: 10.1371/journal.pone.0121713. PMID: 25823008. PMCID: PMC4379078. PMID: 1487ebf3db6e4948981f50c38ce0e938.12. Pifer MA, Maerz T, Baker KC, Anderson K. 2014; Matrix metalloproteinase content and activity in low-platelet, low-leukocyte and high-platelet, high-leukocyte platelet rich plasma (PRP) and the biologic response to PRP by human ligament fibroblasts. Am J Sports Med. 42:1211–8. https://doi.org/10.1177/0363546514524710. DOI: 10.1177/0363546514524710. PMID: 24627579.13. Baeyens W, Glineur R, Evrard L. 2010; [The use of platelet concentrates: platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in bone reconstruction prior to dental implant surgery]. Rev Med Brux. 31:521–7. French.14. Dohan Ehrenfest DM, Bielecki T, Jimbo R, Barbé G, Del Corso M, Inchingolo F, et al. 2012; Do the fibrin architecture and leukocyte content influence the growth factor release of platelet concentrates? An evidence-based answer comparing a pure platelet-rich plasma (P-PRP) gel and a leukocyte- and platelet-rich fibrin (L-PRF). Curr Pharm Biotechnol. 13:1145–52. https://doi.org/10.2174/138920112800624382. DOI: 10.2174/138920112800624382.15. Pandis N. 2012; Sample calculation for split-mouth designs. Am J Orthod Dentofacial Orthop. 141:818–9. https://doi.org/10.1016/j.ajodo.2012.03.015. DOI: 10.1016/j.ajodo.2012.03.015. PMID: 22640684.16. Schulz KF, Altman DG, Moher D. 2010; CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother. 1:100–7. https://doi.org/10.4103/0976-500X.72352. DOI: 10.4103/0976-500X.72352. PMID: 21350618. PMCID: PMC3043330.17. Dohan Ehrenfest DM, Rasmusson L, Albrektsson T. 2009; Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol. 27:158–67. https://doi.org/10.1016/j.tibtech.2008.11.009. DOI: 10.1016/j.tibtech.2008.11.009.18. Ziegler P, Ingervall B. 1989; A clinical study of maxillary canine retraction with a retraction spring and with sliding mechanics. Am J Orthod Dentofacial Orthop. 95:99–106. https://doi.org/10.1016/0889-5406(89)90388-0. DOI: 10.1016/0889-5406(89)90388-0.19. Landry RG, Turnbull RS, Howley T. 1988; Effectiveness of benzydamyne HCl in the treatment of periodontal post-surgical patients. Res Clin Forums. 10:105–18. https://scholar.google.com/scholar_lookup?journal=Res+Clin+Forums&title=Effectiveness+of+benzydamyne+HCl+in+the+treatment+of+periodontal+post-surgical+patients&author=RG+Landry&author=RS+Turnbull&author=T+Howley&volume=10&publication_year=1988&pages=105-118&.20. McCaffery M, Beebe A. 1989. Pain: clinical manual for nursing practice. Mosby;St. Louis: https://books.google.co.kr/books/about/Pain.html?id=GlBwnQAACAAJ&redir_esc=y. DOI: 10.1016/0304-3959(89)90226-1.21. Frost HM. 1983; The regional acceleratory phenomenon: a review. Henry Ford Hosp Med J. 31:3–9. https://pubmed.ncbi.nlm.nih.gov/6345475/. DOI: 10.1159/000351897.22. El-Timamy A, El Sharaby F, Eid F, El Dakroury A, Mostafa Y, Shaker O. 2020; Effect of platelet-rich plasma on the rate of orthodontic tooth movement. Angle Orthod. 90:354–61. https://doi.org/10.2319/072119-483.1. DOI: 10.2319/072119-483.1.23. Gkantidis N, Mistakidis I, Kouskoura T, Pandis N. 2014; Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: a systematic review and meta-analysis. J Dent. 42:1300–19. https://doi.org/10.1016/j.jdent.2014.07.013. DOI: 10.1016/j.jdent.2014.07.013. PMID: 25072362.24. Hoffmann S, Papadopoulos N, Visel D, Visel T, Jost-Brinkmann PG, Präger TM. 2017; Influence of piezotomy and osteoperforation of the alveolar process on the rate of orthodontic tooth movement: a systematic review. J Orofac Orthop. 78:301–11. https://doi.org/10.1007/s00056-017-0085-1. DOI: 10.1007/s00056-017-0085-1.25. Liou EJ. 2016; The development of submucosal injection of platelet rich plasma for accelerating orthodontic tooth movement and preserving pressure side alveolar bone. APOS Trends Orthod. 6:5–11. https://doi.org/10.4103/2321-1407.173725. DOI: 10.4103/2321-1407.173725.26. Li Z, Zhou J, Chen S. 2021; The effectiveness of locally injected platelet-rich plasma on orthodontic tooth movement acceleration. Angle Orthod. 91:391–8. https://doi.org/10.2319/061320-544.1. DOI: 10.2319/061320-544.1.27. Tehranchi A, Behnia H, Pourdanesh F, Behnia P, Pinto N, Younessian F. 2018; The effect of autologous leukocyte platelet rich fibrin on the rate of orthodontic tooth movement: a prospective randomized clinical trial. Eur J Dent. 12:350–7. https://doi.org/10.4103/ejd.ejd_424_17. DOI: 10.4103/ejd.ejd_424_17. PMID: 30147398. PMCID: PMC6089057.28. Nemtoi A, Sirghe A, Nemtoi A, Haba D. 2018; The effect of a plasma with platelet-rich fibrin in bone regeneration and on rate of orthodontic tooth movement in adolescents. Rev Chim. 69:3727–30. https://doi.org/10.37358/RC.18.12.6829. DOI: 10.37358/RC.18.12.6829.29. Erdur EA, Karakaslı K, Oncu E, Ozturk B, Hakkı S. 2021; Effect of injectable platelet-rich fibrin (i-PRF) on the rate of tooth movement. Angle Orthod. 91:285–92. https://doi.org/10.2319/060320-508.1. DOI: 10.2319/060320-508.1.30. Nakornnoi T, Leethanakul C, Samruajbenjakun B. 2019; The influence of leukocyte-platelet-rich plasma on accelerated orthodontic tooth movement in rabbits. Korean J Orthod. 49:372–80. https://doi.org/10.4041/kjod.2019.49.6.372. DOI: 10.4041/kjod.2019.49.6.372. PMID: 31815105. PMCID: PMC6883214.31. Reyes Pacheco AA, Collins JR, Contreras N, Lantigua A, Pithon MM, Tanaka OM. 2020; Distalization rate of maxillary canines in an alveolus filled with leukocyte-platelet-rich fibrin in adults: a randomized controlled clinical split-mouth trial. Am J Orthod Dentofacial Orthop. 158:182–91. https://doi.org/10.1016/j.ajodo.2020.03.020. DOI: 10.1016/j.ajodo.2020.03.020.32. Barhate UH, Duggal I, Mangaraj M, Sharan J, Duggal R, Jena AK. 2022; Effects of autologous leukocyte-platelet rich fibrin (L-PRF) on the rate of maxillary canine retraction and various biomarkers in gingival crevicular fluid (GCF): a split mouth randomized controlled trial. Int Orthod. 20:100681. https://doi.org/10.1016/j.ortho.2022.100681. DOI: 10.1016/j.ortho.2022.100681. PMID: 36151016.33. Çağlı Karcı İ, Baka ZM. 2021; Assessment of the effects of local platelet-rich fibrin injection and piezocision on orthodontic tooth movement during canine distalization. Am J Orthod Dentofacial Orthop. 160:29–40. https://doi.org/10.1016/j.ajodo.2020.03.029. DOI: 10.1016/j.ajodo.2020.03.029.34. Zeitounlouian TS, Zeno KG, Brad BA, Haddad RA. 2021; Effect of injectable platelet-rich fibrin (i-PRF) in accelerating orthodontic tooth movement: a randomized split-mouth-controlled trial. J Orofac Orthop. 82:268–77. https://doi.org/10.1007/s00056-020-00275-x. DOI: 10.1007/s00056-020-00275-x.35. Zeitounlouian TS, Zeno KG, Brad BA, Haddad RA. 2021; Three-dimensional evaluation of the effects of injectable platelet rich fibrin (i-PRF) on alveolar bone and root length during orthodontic treatment: a randomized split mouth trial. BMC Oral Health. 21:92. https://doi.org/10.1186/s12903-021-01456-9. DOI: 10.1186/s12903-021-01456-9. PMID: 33653326. PMCID: PMC7971145. PMID: b6d0a221c58c43a9962c172673cf8714.36. de Almeida Barros Mourão CF, de Mello-Machado RC, Javid K, Moraschini V. 2020; The use of leukocyte- and platelet-rich fibrin in the management of soft tissue healing and pain in post-extraction sockets: a randomized clinical trial. J Craniomaxillofac Surg. 48:452–7. https://doi.org/10.1016/j.jcms.2020.02.020. DOI: 10.1016/j.jcms.2020.02.020.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Platelet-rich Plasma on Burn Wounds according to Time of Application: An Experimental Study on Rats
- Leukocyte platelet-rich fibrin in endodontic microsurgery: a report of 2 cases
- Clinical effectiveness of combining platelet rich fibrin with alloplastic bone substitute for the management of combined endodontic periodontal lesion
- Acceleration of Wound Healing Using Adipose-derived Stem Cell Therapy with Platelet Concentrates: Platelet-rich Plasma (PRP) vs. Platelet-rich Fibrin (PRF)
- The double-barrier technique using platelet-rich fibrin for closure of oroantral fistulas