Clin Transplant Res.
2024 Sep;38(3):188-196. 10.4285/ctr.24.0025.
Assessment of fluid responsiveness after tidal volume challenge in renal transplant recipients: a nonrandomized prospective interventional study
- Affiliations
-
- 1Department of Organ Transplant Anaesthesia and Critical Care, Mahatma Gandhi Medical College and Hospital, Jaipur, India
- 2Department of Anaesthesia, Mahatma Gandhi Medical College and Hospital, Jaipur, India
- 3Division of Biostatistics, Department of Community Medicine, Mahatma Gandhi Medical College and Hospital, Jaipur, India
- KMID: 2559804
- DOI: http://doi.org/10.4285/ctr.24.0025
Abstract
- Background
When applying lung-protective ventilation, fluid responsiveness cannot be predicted by pulse pressure variation (PPV) or stroke volume variation (SVV). Functional hemodynamic testing may help address this limitation. This study examined whether changes in dynamic indices such as PPV and SVV, induced by tidal volume challenge (TVC), can reliably predict fluid responsiveness in patients undergoing renal transplantation who receive lung-protective ventilation.
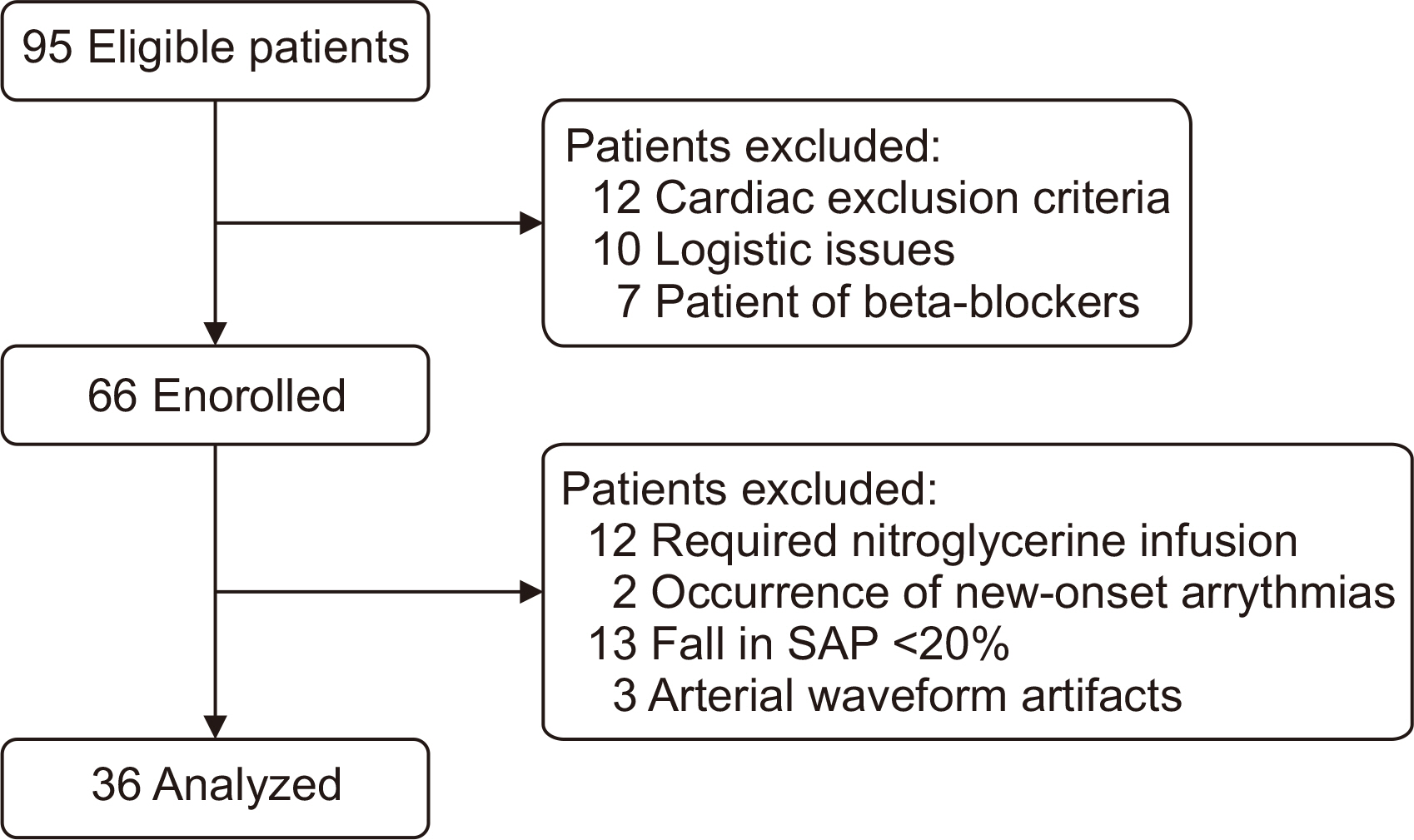
Methods
This nonrandomized interventional study included renal transplant recipients with end-stage renal disease. Patients received ventilation with a 6 mL/kg tidal volume (TV), and the FloTrac system was attached for continuous hemodynamic monitoring. Participants were classified as responders or nonresponders based on whether fluid challenge increased the stroke volume index by more than 10%.
Results
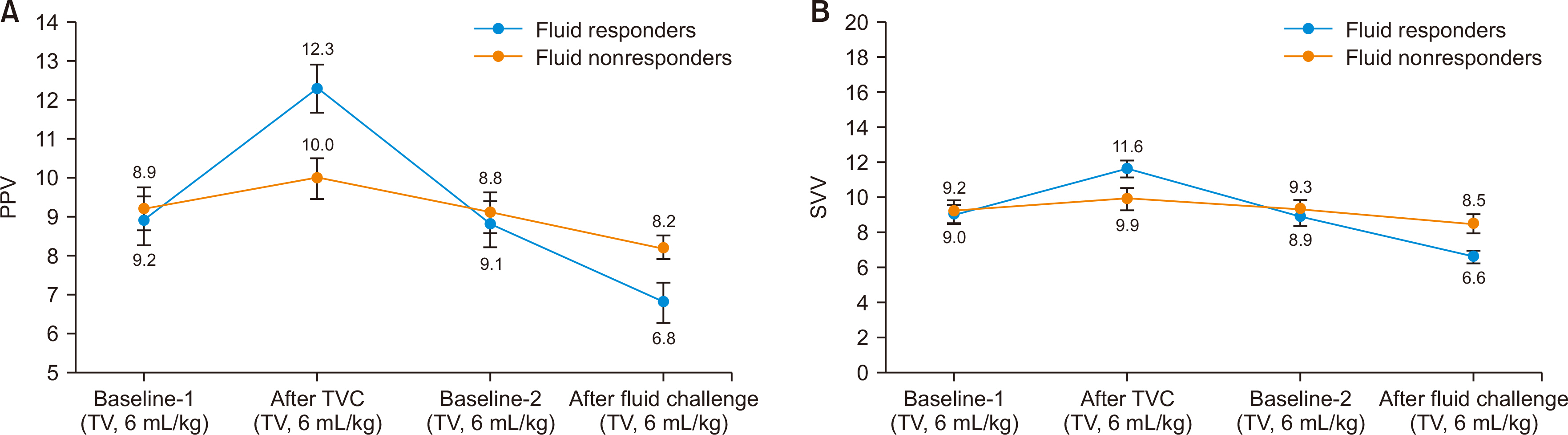
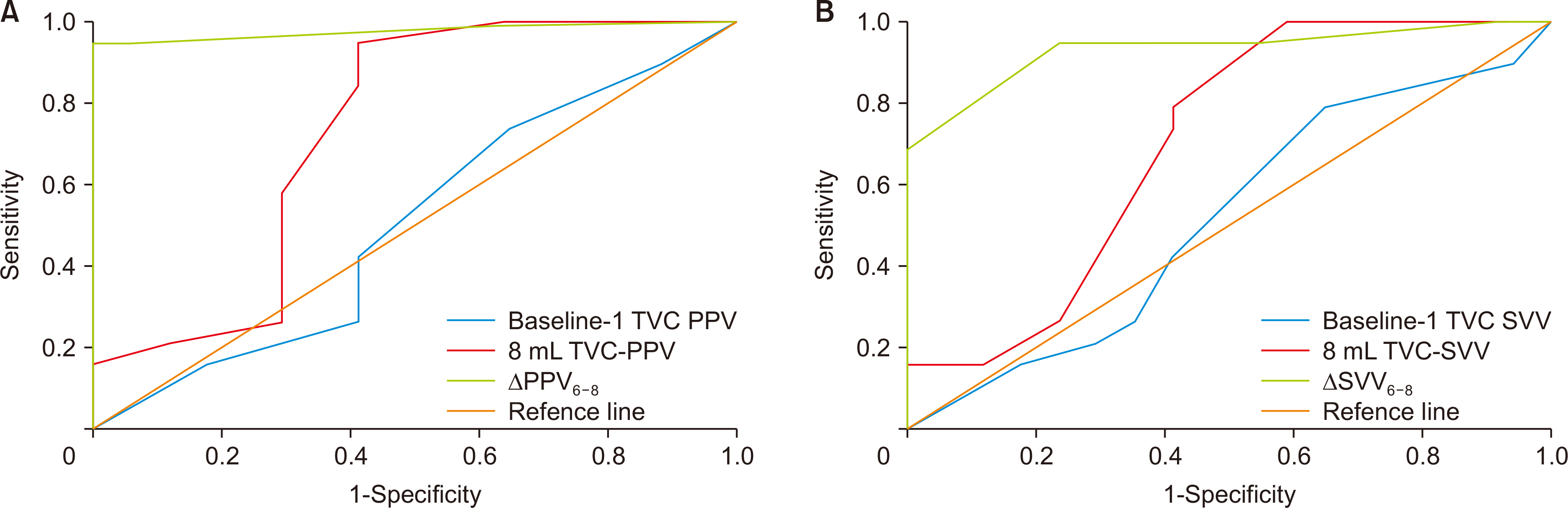
The analysis included 36 patients, of whom 19 (52.8%) were responders and 17 (47.2%) were nonresponders. Among responders, the mean ∆PPV 6-8 (calculated as PPV at a TV of 8 mL/kg predicted body weight [PBW] minus that at 6 mL/kg PBW) was 3.32±0.75 and ∆SVV 6-8 was 2.58±0.77, compared to 0.82±0.53 and 0.70±0.92 for nonresponders, respectively. ∆PPV 6-8 exhibited an area under the curve (AUC) of 0.97 95% confidence interval [CI], 0.93–1.00; P≤0.001), with an optimal cutoff value of 1.5, sensitivity of 94.7%, and specificity of 94.1%. ∆SVV 6-8 displayed an AUC of 0.93 (95% CI, 0.84–1.00; P≤0.001) at the same cutoff value of 1.5, with a sensitivity of 94.7% and a specificity of 76.5%.
Conclusions
TVC-induced changes in PPV and SVV are predictive of fluid responsiveness in renal transplant recipients who receive intraoperative lung-protective ventilation.
Figure
Reference
-
1. Lemmens HJ. 2004; Kidney transplantation: recent developments and recommendations for anesthetic management. Anesthesiol Clin North Am. 22:651–62. DOI: 10.1016/j.atc.2004.05.007. PMID: 15541928.2. Calixto Fernandes MH, Schricker T, Magder S, Hatzakorzian R. 2018; Perioperative fluid management in kidney transplantation: a black box. Crit Care. 22:14. DOI: 10.1186/s13054-017-1928-2. PMID: 29368625. PMCID: PMC5784708.3. Wagener G, Bezinover D, Wang C, Kroepfl E, Diaz G, Giordano C, et al. 2021; Fluid management during kidney transplantation: a consensus statement of the committee on transplant anesthesia of the American Society of Anesthesiologists. Transplantation. 105:1677–84. DOI: 10.1097/TP.0000000000003581. PMID: 33323765.4. Messina A, Longhini F, Coppo C, Pagni A, Lungu R, Ronco C, et al. 2017; Use of the fluid challenge in critically ill adult patients: a systematic review. Anesth Analg. 125:1532–43. DOI: 10.1213/ANE.0000000000002103. PMID: 28514324.5. Cavaleri M, Veroux M, Palermo F, Vasile F, Mineri M, Palumbo J, et al. 2019; Perioperative goal-directed therapy during kidney transplantation: an impact evaluation on the major postoperative complications. J Clin Med. 8:80. DOI: 10.3390/jcm8010080. PMID: 30642015. PMCID: PMC6351933.6. Goyal VK, Gupta P, Baj B, Garg VK. 2021; A randomized comparison between pulse pressure variation and central venous pressure in patients undergoing renal transplantation. J Anaesthesiol Clin Pharmacol. 37:628–32. DOI: 10.4103/joacp.JOACP_23_20. PMID: 35340962. PMCID: PMC8944348.7. Kannan G, Loganathan S, Kajal K, Hazarika A, Sethi S, Sen IM, et al. 2022; The effect of pulse pressure variation compared with central venous pressure on intraoperative fluid management during kidney transplant surgery: a randomized controlled trial. Can J Anaesth. 69:62–71. DOI: 10.1007/s12630-021-02130-y. PMID: 34750747.8. Biais M, Ehrmann S, Mari A, Conte B, Mahjoub Y, Desebbe O, et al. 2014; Clinical relevance of pulse pressure variations for predicting fluid responsiveness in mechanically ventilated intensive care unit patients: the grey zone approach. Crit Care. 18:587. DOI: 10.1186/s13054-014-0587-9. PMID: 25658489. PMCID: PMC4240833.9. De Cassai A, Bond O, Marini S, Panciera G, Furian L, Neri F, et al. 2020; Pulse pressure variation guided fluid therapy during kidney transplantation: a randomized controlled trial. Braz J Anesthesiol. 70:194–201. DOI: 10.1016/j.bjan.2020.02.008. PMID: 32534731. PMCID: PMC9373208.10. Eikermann M, Kurth T. 2015; Apply protective mechanical ventilation in the operating room in an individualized approach to perioperative respiratory care. Anesthesiology. 123:12–4. DOI: 10.1097/ALN.0000000000000707. PMID: 25978325.11. Myatra SN, Prabu NR, Divatia JV, Monnet X, Kulkarni AP, Teboul JL. 2017; The changes in pulse pressure variation or stroke volume variation after a "tidal volume challenge" reliably predict fluid responsiveness during low tidal volume ventilation. Crit Care Med. 45:415–21. DOI: 10.1097/CCM.0000000000002183.12. Alvarado Sánchez JI, Caicedo Ruiz JD, Diaztagle Fernández JJ, Amaya Zuñiga WF, Ospina-Tascón GA, Cruz Martínez LE. 2021; Predictors of fluid responsiveness in critically ill patients mechanically ventilated at low tidal volumes: systematic review and meta-analysis. Ann Intensive Care. 11:28. DOI: 10.1186/s13613-021-00817-5. PMID: 33555488. PMCID: PMC7870741.13. Wang X, Liu S, Gao J, Zhang Y, Huang T. 2023; Does tidal volume challenge improve the feasibility of pulse pressure variation in patients mechanically ventilated at low tidal volumes? A systematic review and meta-analysis. Crit Care. 27:45. DOI: 10.1186/s13054-023-04336-6. PMID: 36732851. PMCID: PMC9893685.14. Yonis H, Bitker L, Aublanc M, Perinel Ragey S, Riad Z, Lissonde F, et al. 2017; Change in cardiac output during Trendelenburg maneuver is a reliable predictor of fluid responsiveness in patients with acute respiratory distress syndrome in the prone position under protective ventilation. Crit Care. 21:295. DOI: 10.1186/s13054-017-1881-0. PMID: 29208025. PMCID: PMC5718075.15. Jun JH, Chung RK, Baik HJ, Chung MH, Hyeon JS, Lee YG, et al. 2019; The tidal volume challenge improves the reliability of dynamic preload indices during robot-assisted laparoscopic surgery in the Trendelenburg position with lung-protective ventilation. BMC Anesthesiol. 19:142. DOI: 10.1186/s12871-019-0807-6. PMID: 31390982. PMCID: PMC6686427.16. Shi R, Ayed S, Moretto F, Azzolina D, De Vita N, Gavelli F, et al. 2022; Tidal volume challenge to predict preload responsiveness in patients with acute respiratory distress syndrome under prone position. Crit Care. 26:219. DOI: 10.1186/s13054-022-04087-w. PMID: 35850771. PMCID: PMC9294836.17. Xu Y, Guo J, Wu Q, Chen J. 2022; Efficacy of using tidal volume challenge to improve the reliability of pulse pressure variation reduced in low tidal volume ventilated critically ill patients with decreased respiratory system compliance. BMC Anesthesiol. 22:137. DOI: 10.1186/s12871-022-01676-8. PMID: 35508962. PMCID: PMC9066736.18. Messina A, Montagnini C, Cammarota G, De Rosa S, Giuliani F, Muratore L, et al. 2019; Tidal volume challenge to predict fluid responsiveness in the operating room: an observational study. Eur J Anaesthesiol. 36:583–91. DOI: 10.1097/EJA.0000000000000998. PMID: 31021879.19. Messina A, Montagnini C, Cammarota G, Giuliani F, Muratore L, Baggiani M, et al. 2020; Assessment of fluid responsiveness in prone neurosurgical patients undergoing protective ventilation: role of dynamic indices, tidal volume challenge, and end-expiratory occlusion test. Anesth Analg. 130:752–61. DOI: 10.1213/ANE.0000000000004494. PMID: 31651455.20. Cannesson M, Le Manach Y, Hofer CK, Goarin JP, Lehot JJ, Vallet B, et al. 2011; Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a "gray zone" approach. Anesthesiology. 115:231–41. DOI: 10.1097/ALN.0b013e318225b80a.21. Messina A, Sotgiu G, Saderi L, Puci M, Negri K, Robba C, et al. 2023; Phenotypes of hemodynamic response to fluid challenge during anesthesia: a cluster analysis. Minerva Anestesiol. 89:653–62. DOI: 10.23736/S0375-9393.23.16992-6. PMID: 36943710.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validity of Corrected Flow Time (FTc) as a Predictor of Fluid Responsiveness in Patients with Sepsis-induced Hypotension
- Predictors of fluid responsiveness in the operating room: a narrative review
- Hemodynamic Response to a Rapid Fluid Challenge in End-Stage Liver Disease
- Ability of dynamic preload indices to predict fluid responsiveness in a high femoral-to-radial arterial pressure gradient: a retrospective study
- Comparison between the Set and the Measured Tidal Volume in the Pediatric Patients Using the Adult Volume-Limited Ventilator