J Korean Med Sci.
2024 Oct;39(38):e257. 10.3346/jkms.2024.39.e257.
Validity and Reliability of the Korean Version of Reduced Morningness– Eveningness Questionnaire: Results From a General Population-Based Sample
- Affiliations
-
- 1Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Neurology, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 3Department of Convergence Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 4Department of Neurology, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- KMID: 2559783
- DOI: http://doi.org/10.3346/jkms.2024.39.e257
Abstract
- Background
Chronotype refers to individual variations in diurnal preferences that manifest as everyday behaviors, including sleep patterns. Traditionally, the Horne & Östberg Morningness–Eveningness Questionnaire (MEQ), which comprises of 19 items, has been the standard for determining chronotype. However, its length makes it cumbersome for widespread application. To address this issue, the reduced MEQ (rMEQ), a concise version containing only five items from the MEQ, was developed for a more practical approach to chronotype assessment. This study aimed to evaluate the validity and reliability of Korean version of rMEQ in a sample from the general Korean population.
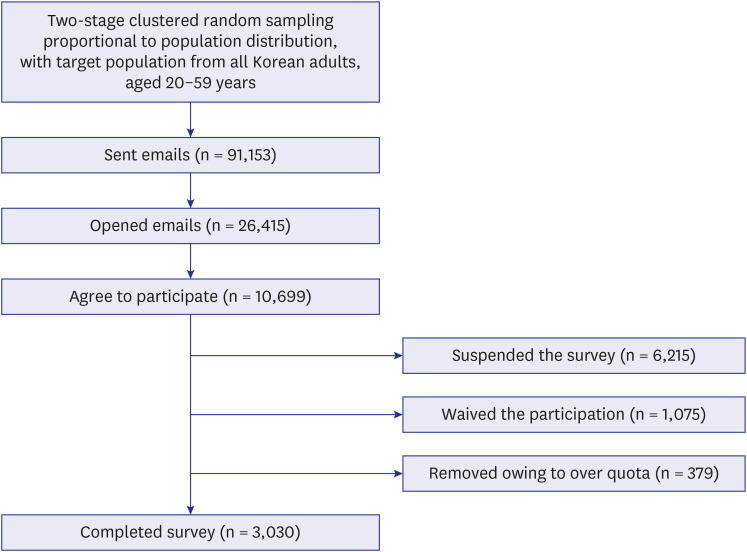
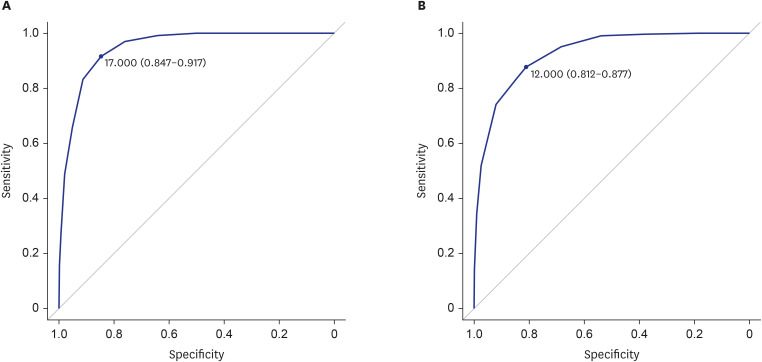
Methods
The Korean version of the rMEQ comprises of items 1, 7, 10, 18, and 19 of the original MEQ. The validity of the rMEQ was assessed by correlating its scores with those of the MEQ and Munich Chronotype Questionnaire (MCTQ). Its reliability was determined by calculating internal consistency.
Results
A total of 3,030 individuals participated in the study, yielding an average rMEQ score of 14.0 ± 3.4. There was a substantial positive correlation between the rMEQ and MEQ scores (r = 0.859, P < 0.001). Furthermore, the rMEQ scores were significantly negatively correlated with the midpoint of sleep on free days corrected for sleep debt as measured by the MCTQ (r = −0.388, P < 0.001), indicating a robust association with chronotype. The internal consistency of rMEQ, measured using Cronbach’s alpha, was 0.609.
Conclusion
This study finds the Korean version of the rMEQ to be a valid and reliable instrument for assessing chronotype in the general population.
Keyword
Figure
Reference
-
1. Roenneberg T, Merrow M. The circadian clock and human health. Curr Biol. 2016; 26(10):R432–R443. PMID: 27218855.2. Kreitzman L, Foster R. The Rhythms of Life: The Biological Clocks That Control the Daily Lives of Every Living Thing. London, UK: Profile Books;2011.3. Potter GD, Skene DJ, Arendt J, Cade JE, Grant PJ, Hardie LJ. Circadian rhythm and sleep disruption: causes, metabolic consequences, and countermeasures. Endocr Rev. 2016; 37(6):584–608. PMID: 27763782.4. Levandovski R, Sasso E, Hidalgo MP. Chronotype: a review of the advances, limits and applicability of the main instruments used in the literature to assess human phenotype. Trends Psychiatry Psychother. 2013; 35(1):3–11. PMID: 25923181.5. Fabbian F, Zucchi B, De Giorgi A, Tiseo R, Boari B, Salmi R, et al. Chronotype, gender and general health. Chronobiol Int. 2016; 33(7):863–882. PMID: 27148626.6. Juda M, Vetter C, Roenneberg T. Chronotype modulates sleep duration, sleep quality, and social jet lag in shift-workers. J Biol Rhythms. 2013; 28(2):141–151. PMID: 23606613.7. Di Milia L, Adan A, Natale V, Randler C. Reviewing the psychometric properties of contemporary circadian typology measures. Chronobiol Int. 2013; 30(10):1261–1271. PMID: 24001393.8. Roveda E, Vitale J, Montaruli A, Galasso L, Carandente F, Caumo A. Predicting the actigraphy-based acrophase using the Morningness-Eveningness Questionnaire (MEQ) in college students of North Italy. Chronobiol Int. 2017; 34(5):551–562. PMID: 28276851.9. Adán AG, Almirall H. Horne & Östberg Morningness-Eveningness Questionnaire: a reduced scale. Pers Individ Dif. 1991; 12(3):241–253.10. Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, et al. Epidemiology of the human circadian clock. Sleep Med Rev. 2007; 11(6):429–438. PMID: 17936039.11. Zavada A, Gordijn MC, Beersma DG, Daan S, Roenneberg T. Comparison of the Munich Chronotype Questionnaire with the Horne-Ostberg’s Morningness-Eveningness score. Chronobiol Int. 2005; 22(2):267–278. PMID: 16021843.12. Burgess HJ, Savic N, Sletten T, Roach G, Gilbert SS, Dawson D. The relationship between the dim light melatonin onset and sleep on a regular schedule in young healthy adults. Behav Sleep Med. 2003; 1(2):102–114. PMID: 15600132.13. Kantermann T, Sung H, Burgess HJ. Comparing the Morningness-Eveningness Questionnaire and Munich ChronoType Questionnaire to the dim light melatonin onset. J Biol Rhythms. 2015; 30(5):449–453. PMID: 26243627.14. Kitamura S, Hida A, Aritake S, Higuchi S, Enomoto M, Kato M, et al. Validity of the Japanese version of the Munich ChronoType Questionnaire. Chronobiol Int. 2014; 31(7):845–850. PMID: 24824747.15. Lewy AJ. Melatonin and human chronobiology. Cold Spring Harb Symp Quant Biol. 2007; 72(1):623–636. PMID: 18419322.16. Kim KM, Kim BK, Lee W, Hwang H, Heo K, Chu MK. Prevalence and impact of visual aura in migraine and probable migraine: a population study. Sci Rep. 2022; 12(1):426. PMID: 35013446.17. Horne JA, Ostberg O. A self-assessment questionnaire to determine Morningness-Eveningness in human circadian rhythms. Int J Chronobiol. 1976; 4(2):97–110. PMID: 1027738.18. Lee JH, Kim SJ, Lee SY, Jang KH, Kim IS, Duffy JF. Reliability and validity of the Korean version of Morningness-Eveningness Questionnaire in adults aged 20-39 years. Chronobiol Int. 2014; 31(4):479–486. PMID: 24467306.19. Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms. 2003; 18(1):80–90. PMID: 12568247.20. Suh S, Kim SH, Ryu H, Choi SJ, Joo EY. Validation of the Korean Munich Chronotype Questionnaire. Sleep Breath. 2018; 22(3):773–779. PMID: 29340848.21. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193–213. PMID: 2748771.22. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001; 2(4):297–307. PMID: 11438246.23. Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V, Randler C. Circadian typology: a comprehensive review. Chronobiol Int. 2012; 29(9):1153–1175. PMID: 23004349.24. Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012; 16(3):803–812. PMID: 21901299.25. Cho YW, Song ML, Morin CM. Validation of a Korean version of the insomnia severity index. J Clin Neurol. 2014; 10(3):210–215. PMID: 25045373.26. Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002; 32(9):509–515.27. Park SJ, Choi HR, Choi JH, Kim KW, Hong JP. Reliability and validity of the Korean version of the Patient Health Questionnaire-9 (PHQ-9). Anxiety Mood. 2010; 6(2):119–124.28. Kim HY. Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor Dent Endod. 2013; 38(1):52–54. PMID: 23495371.29. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013; 48(3):452–458. PMID: 23208313.30. Cerny BA, Kaiser HF. A study of a measure of sampling adequacy for factor-analytic correlation matrices. Multivariate Behav Res. 1977; 12(1):43–47. PMID: 26804143.31. Shrestha N. Factor analysis as a tool for survey analysis. Am J Appl Math Stat. 2021; 9(1):4–11.32. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951; 16(3):297–334.33. Kuder GF, Richardson MW. The theory of the estimation of test reliability. Psychometrika. 1937; 2(3):151–160.34. Byrne BM. Factor analytic models: viewing the structure of an assessment instrument from three perspectives. J Pers Assess. 2005; 85(1):17–32. PMID: 16083381.35. Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods. 1999; 4(3):272–299.36. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999; 6(1):1–55.37. Kim H, Ku B, Kim JY, Park YJ, Park YB. Confirmatory and exploratory factor analysis for validating the Phlegm pattern questionnaire for healthy subjects. Evid Based Complement Alternat Med. 2016; 2016:2696019. PMID: 27051447.38. Thorndike RM. Book Review: Psychometric Theory (3rd ed.) by Jum Nunnally and Ira Bernstein. Appl Psychol Meas. 1995; 19(3):303–305.39. Danielsson K, Sakarya A, Jansson-Fröjmark M. The reduced Morningness-Eveningness Questionnaire: psychometric properties and related factors in a young Swedish population. Chronobiol Int. 2019; 36(4):530–540. PMID: 30614272.40. Jankowski K. Polish version of the reduced Morningness–Eveningness Questionnaire. Biol Rhythm Res. 2013; 44(3):427–433.41. Rahafar AJ, Sadeghpour A, Heidari Z, Kasaeian A. Psychometric properties of the Persian version of the reduced Morningness-Eveningness Questionnaire: further evidence: Persian rMEQ; further evidence. Sleep Biol Rhythms. 2015; 13(2):112–116.42. Paciello LM, Quante M, Weidenauer C, Rueschman M, Nieratschker V, Poets CF, et al. Validity of chronotype questionnaires in adolescents: correlations with actigraphy. J Sleep Res. 2022; 31(5):e13576. PMID: 35246881.43. Caci H, Deschaux O, Adan A, Natale V. Comparing three morningness scales: age and gender effects, structure and cut-off criteria. Sleep Med. 2009; 10(2):240–245. PMID: 18387342.44. Ryu H, Joo EY, Choi SJ, Suh S. Validation of the Munich ChronoType Questionnaire in Korean older adults. Psychiatry Investig. 2018; 15(8):775–782.45. Reis C, Madeira SG, Lopes LV, Paiva T, Roenneberg T. Validation of the portuguese variant of the Munich Chronotype Questionnaire (MCTQPT). Front Physiol. 2020; 11:795. PMID: 32760292.46. Chen CH, Huang MC, Chiu YH, Chen IM, Chen CH, Lu ML, et al. Stress susceptibility moderates the relationship between eveningness preference and poor sleep quality in non-acute mood disorder patients and healthy controls. Nat Sci Sleep. 2022; 14:711–723. PMID: 35450221.47. Taillard J, Philip P, Bioulac B. Morningness/eveningness and the need for sleep. J Sleep Res. 1999; 8(4):291–295. PMID: 10646169.48. Chung MH, Chang FM, Yang CC, Kuo TB, Hsu N. Sleep quality and morningness-eveningness of shift nurses. J Clin Nurs. 2009; 18(2):279–284. PMID: 19120754.49. Li SX, Chan NY, Man Yu MW, Lam SP, Zhang J, Yan Chan JW, et al. Eveningness chronotype, insomnia symptoms, and emotional and behavioural problems in adolescents. Sleep Med. 2018; 47:93–99. PMID: 29778920.50. Chan NY, Zhang J, Tsang CC, Li AM, Chan JW, Wing YK, et al. The associations of insomnia symptoms and chronotype with daytime sleepiness, mood symptoms and suicide risk in adolescents. Sleep Med. 2020; 74:124–131. PMID: 32853897.51. Koo DL, Yang KI, Kim JH, Kim D, Sunwoo JS, Hwangbo Y, et al. Association between morningness-eveningness, sleep duration, weekend catch-up sleep and depression among Korean high-school students. J Sleep Res. 2021; 30(1):e13063. PMID: 32391631.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Preliminary Study of Reliability and Validity on the Korean Version of Personality Disorder Questionnaire-4+ (PDQ-4+)
- The Validity and Reliability of a Korean Version of the Summary of Diabetes Self-Care Activities Questionnaire for Older Patients with Type 2 Diabetes
- Psychometric Evaluation of the Korean version of the Penn State Worry Questionnaire with a Sample of University Students
- Teleworking Survey in Saudi Arabia: Reliability and Validity of Arabic Version of the Questionnaire
- Morningness-Eveningness Affects the Depressive Mood and Day Time Sleepiness of Obstructive Sleep Apnea Syndrome Patient