Anat Cell Biol.
2024 Sep;57(3):363-369. 10.5115/acb.23.305.
Surgical anatomy of transversus abdominis muscle for transversus abdominis release
- Affiliations
-
- 1Department of Anatomy, Christian Medical College, Affiliated to the Tamil Nadu Dr. MGR Medical University, Vellore, India
- 2Department of General Surgery, Christian Medical College, Affiliated to the Tamil Nadu Dr. MGR Medical University, Vellore, India
- KMID: 2559749
- DOI: http://doi.org/10.5115/acb.23.305
Abstract
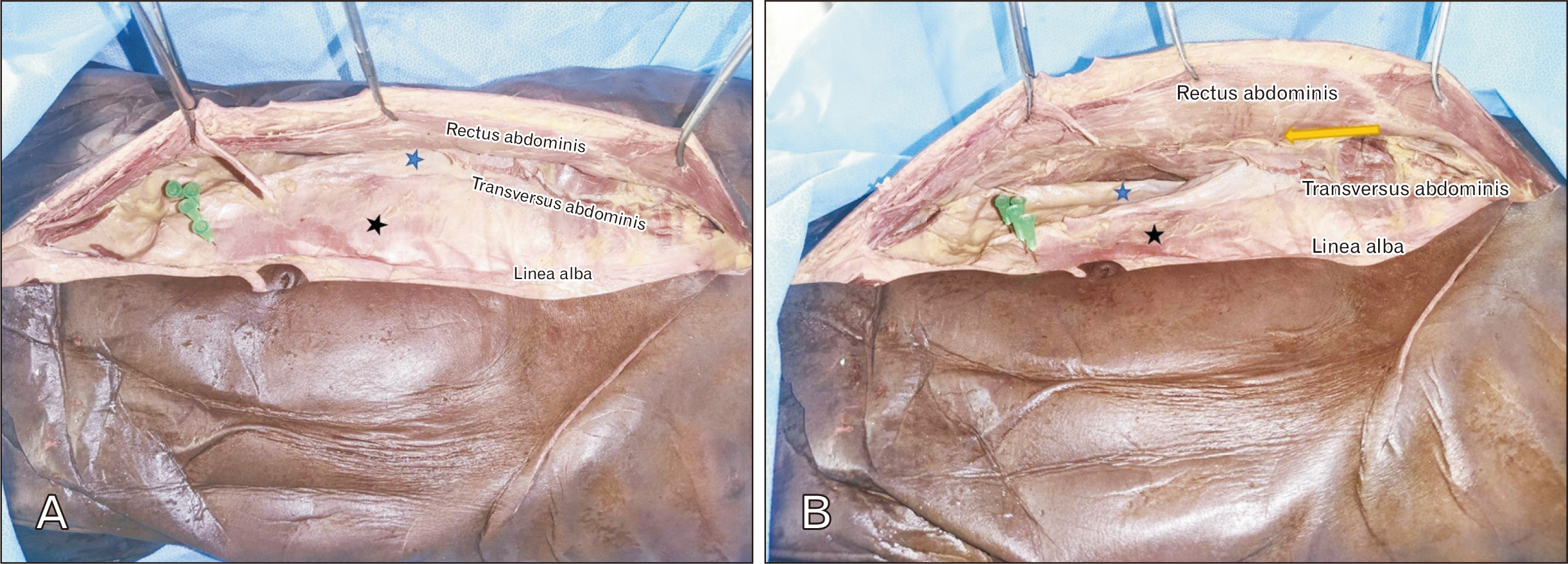
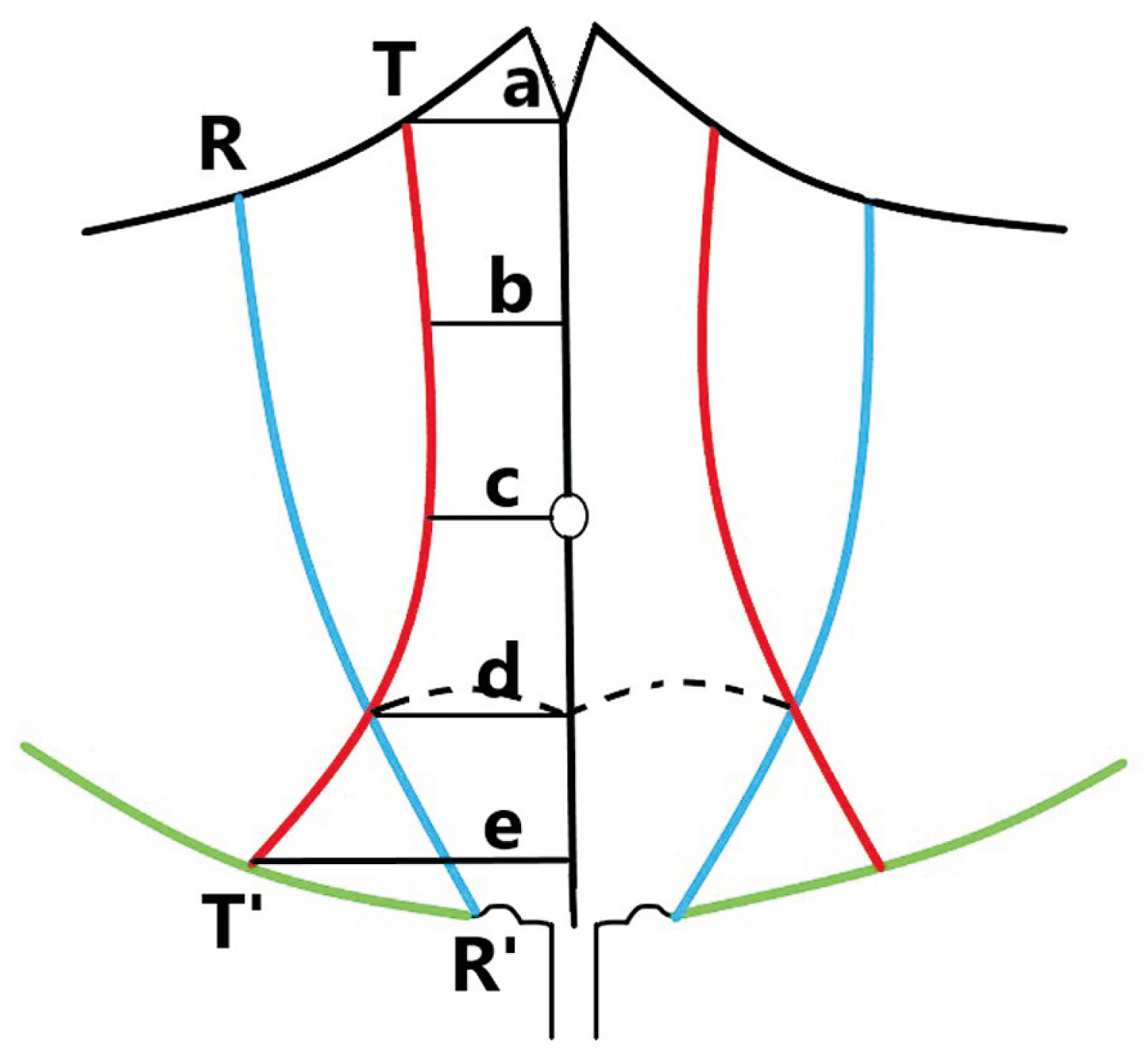
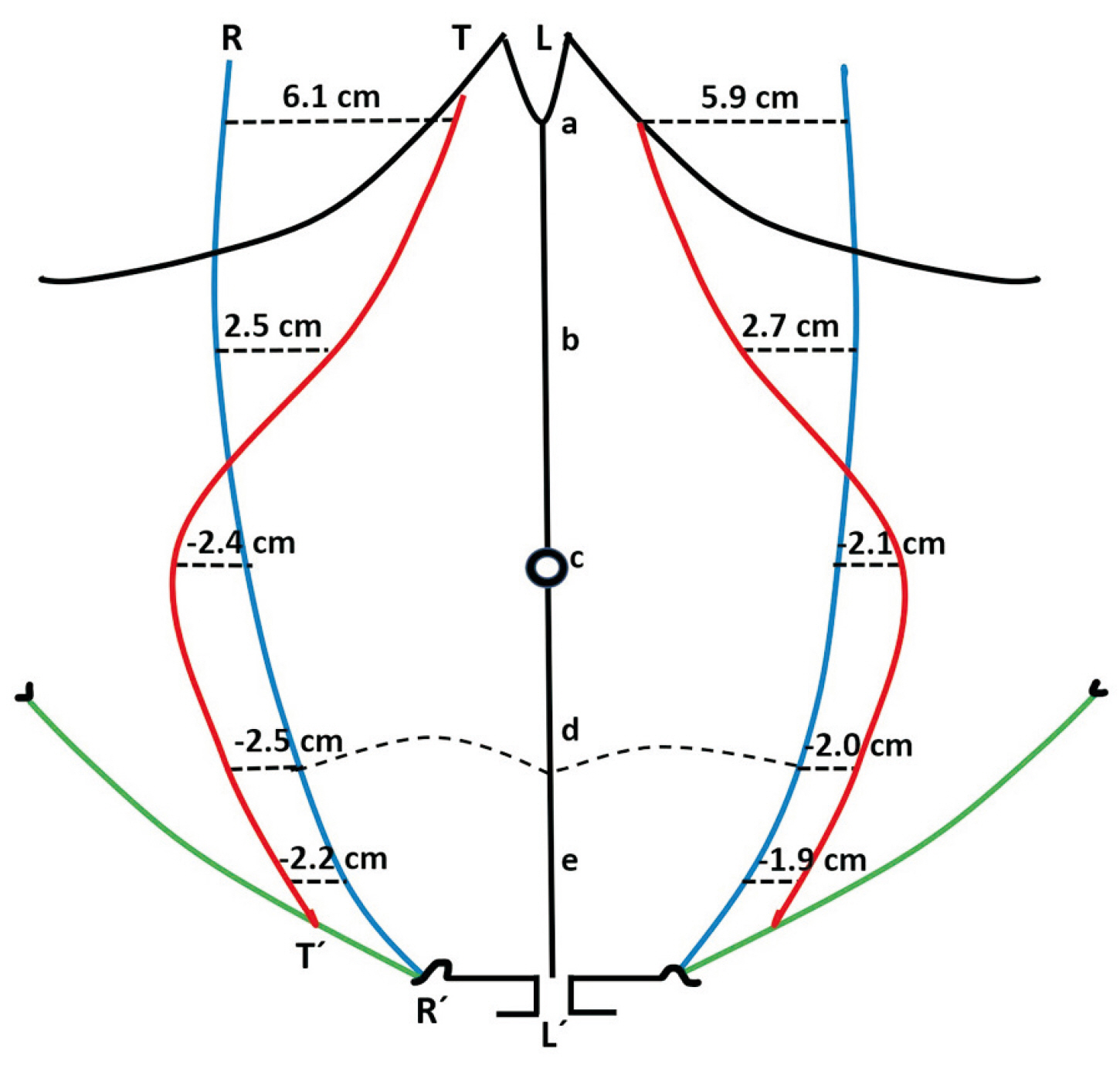
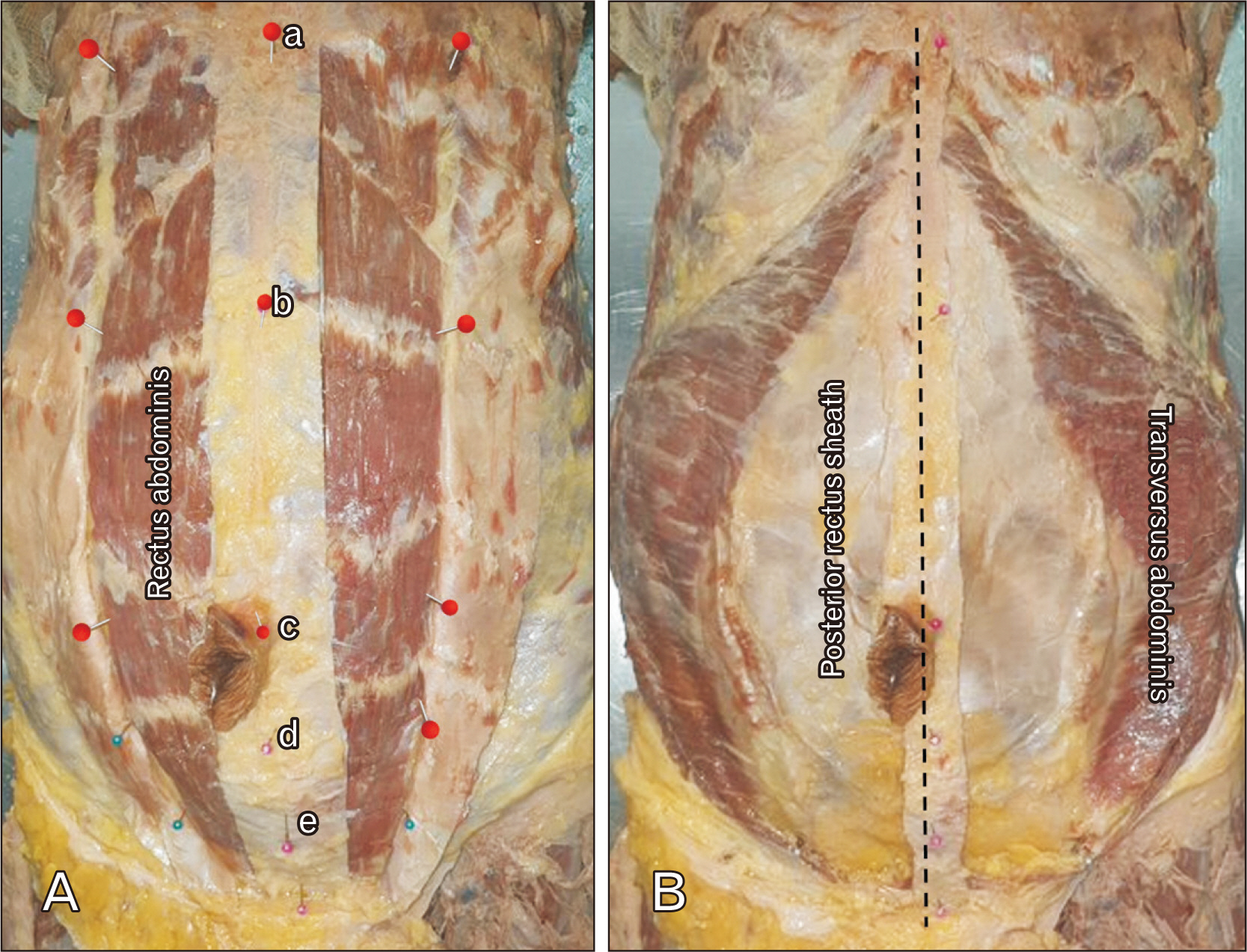
- Transversus abdominis release (TAR) is a myofascial release technique which helps in surgical repair of large ventral abdominal wall defects. In this procedure, the medial margin of muscular part of transversus abdominis (TA) is of great importance. Hence, the authors sought to describe the extent of medial margin of TA muscle. The surgical steps of TAR were performed in 10 formalin-fixed cadavers and distance between medial margin of TA muscle, lateral margin of rectus abdominis, to linea alba at five anatomical levels were documented respectively. The distance between the inferior epigastric vessels and the medial border of TA muscle was also noted. The TA muscle was within the posterior rectus sheath in all cadavers, at the xiphisternum (R, 61.6 mm; L, 58.9 mm), and at midway between xiphisternum and umbilicus (R, 25.4 mm; L, 27.1 mm). The TA muscle exited the posterior rectus sheath between this point and the umbilicus. The mean incongruity at the next three levels were –24.6 mm, –24.9 mm, and –22.9 mm respectively on the right and –21.4 mm, –19.9 mm, and –18.9 mm respectively on the left. The mean distance between the medial border of TA and inferior epigastric vessels was 18.9 mm on the right and 17.2 mm on the left. The muscular part of TA was incorporated within the posterior rectus sheath above the umbilicus, and it completely exited the rectus sheath at the umbilicus. This is contrary to the traditional understanding of posterior rectus sheath formation.
Figure
Reference
-
References
1. Standring S. Gray's anatomy: the anatomical basis of clinical practice. 42nd ed. Elsevier;2020. p. 1078.2. Sinnatamby CS, editor. Abdomen. Last's Anatomy: Regional and Applied. 12th ed. Elsevier;2011. p. 221–6.3. Snell RS, editor. Abdominal wall. Clinical Anatomy by Regions. 9th ed. Lippincott Williams & Wilkins;2012. p. 126–134.4. Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ. 2012; Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg. 204:709–16. DOI: 10.1016/j.amjsurg.2012.02.008. PMID: 22607741.5. Carbonell AM, Cobb WS, Chen SM. 2008; Posterior components separation during retromuscular hernia repair. Hernia. 12:359–62. DOI: 10.1007/s10029-008-0356-2. PMID: 18293053.6. Poulose BK. 2016; Transversus abdominis muscle release: innovations in technique can still happen. Ann Surg. 264:233–4. DOI: 10.1097/SLA.0000000000001734. PMID: 27414154.7. Punekar IRA, Khouri JS, Catanzaro M, Shaikh AL, Langstein HN. 2018; Redefining the rectus sheath: implications for abdominal wall repair. Plast Reconstr Surg. 141:473–9. DOI: 10.1097/PRS.0000000000004043. PMID: 29068903.8. Skandalakis JE, editor. Abdominal wall and hernias. Skandalakis' Surgical Anatomy: the Embryologic and Anatomic Basis of Modern Surgery. Paschalidis Medical Publications;2004. p. 405–407.9. Como JJ, Gunter OL, Diaz JJ, Ho VP, Miller PR. 2019; Use of posterior component separation and transversus abdominis release in trauma and emergency general surgery patients: a case report and review of the literature. Trauma Surg Acute Care Open. 4:e000268. DOI: 10.1136/tsaco-2018-000268. PMID: 30793037. PMCID: PMC6350719.10. Majumder A, Miller HJ, Del Campo LM, Soltanian H, Novitsky YW. 2018; Assessment of myofascial medialization following posterior component separation via transversus abdominis muscle release in a cadaveric model. Hernia. 22:637–44. DOI: 10.1007/s10029-018-1771-7. PMID: 29713832.11. Pauli EM, Rosen MJ. 2013; Open ventral hernia repair with component separation. Surg Clin North Am. 93:1111–33. DOI: 10.1016/j.suc.2013.06.010. PMID: 24035078.12. Ramirez OM, Ruas E, Dellon AL. 1990; "Components separation" method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 86:519–26. DOI: 10.1097/00006534-199009000-00023. PMID: 2143588.13. Parnaby CN, Nicholls D, Docherty JG. 2011; Inferior epigastric artery false aneurysm following incisional hernia repair. Int J Surg Case Rep. 2:178–80. DOI: 10.1016/j.ijscr.2011.05.005. PMID: 22096720. PMCID: PMC3199627.14. Balachandran P, Pandian S, V C S, T S S, Chordia DA. 2022; Pseudoaneurysm of the inferior epigastric artery following laparoscopic extended totally extraperitoneal repair for inguinal hernia. Cureus. 14:e23377. DOI: 10.7759/cureus.23377. PMID: 35475070. PMCID: PMC9021683.15. Alam N, Sheen AJ. 2021; Total extraperitoneal hernia repair and its associated pitfalls. Mini-invasive Surg. 5:48. DOI: 10.20517/2574-1225.2021.65.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transversus abdominis plane block as a sole anesthetic technique for evacuation of rectus abdominis muscle hematoma - A case report -
- Comparison of the effectiveness of subcostal transversus abdominis plane and rectus sheath blocks in postoperative analgesia in major open gynecological cancer surgeries: a prospective randomized study
- Anterior Diaphragm Below the Xiphoid Process: CT Finding
- Development of the Rectus Abdominis and Its Sheath in the Human Fetus
- Response to "Comment on Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: a randomized comparative trial"