Obstet Gynecol Sci.
2024 Sep;67(5):497-505. 10.5468/ogs.22316.
Does it affect the live birth rates to have a maximum endometrial thickness of 7, 8, or 9 mm in in-vitro fertilization-embryo transfer cycles?
- Affiliations
-
- 1Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, MUHC Reproductive Center, McGill University, Montreal, QC, Canada
- 2Department of Faculty of Medicine, Technion-Israel Institute of Technology, Haifa, Israel
- KMID: 2559481
- DOI: http://doi.org/10.5468/ogs.22316
Abstract
Objective
To assess the effect of endometrial thickness (EMT) on live birth rates (LBR) in women with endometrial lining between 7.0-9.9 mm.
Methods
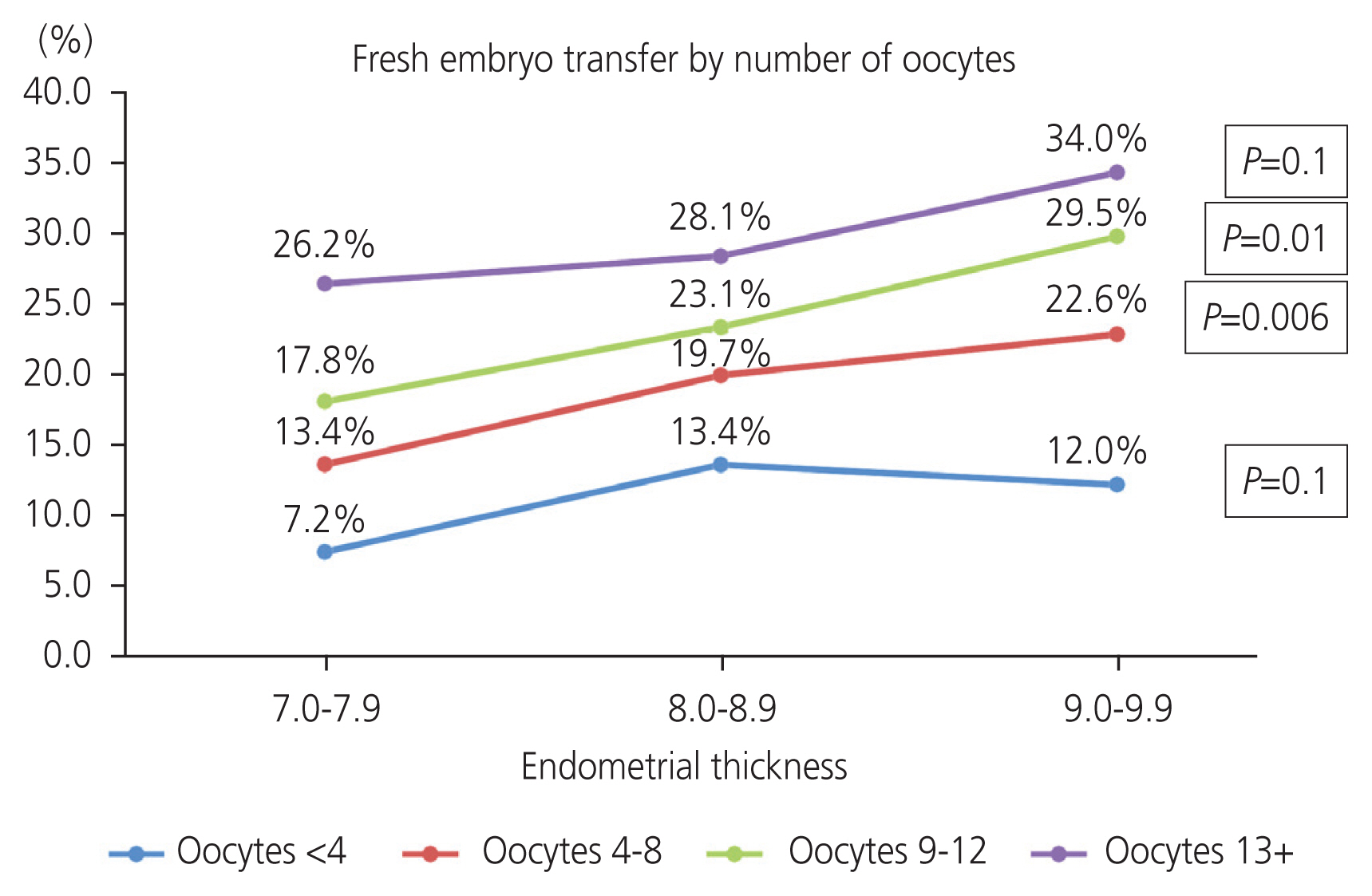
This retrospective cohort study included women who underwent fresh and frozen embryo transfers between 2008 and 2018, grouped according to their maximum EMT; group 1, 7.0-7.9 mm; group 2, 8.0-8.9 mm; and group 3, 9.0-9.9 mm and underwent blastocyst transfer.
Results
The study included 7,091 in-vitro fertilization cycles: 1,385 in group 1, 3,000 in group 2, and 2,706 in group 3. The combined LBR was 22.2%. The mean age of women at oocyte retrieval day was 36.7±4.5 years. There was no difference in female age at oocyte retrieval or in the quality of embryos transferred between the three groups. Group 1 had more diagnoses of diminished ovarian reserve (25.8% vs. 19.5% and 19.1%; p<0.001) and less male factor infertility compared with group 2 and 3, respectively (25.0% vs. 28.8% and 28.5%; P=0.024). LBR was higher with increasing endometrial thickness, group 2 vs. group 1 (22.0% vs. 17.4%; P=0.0004), group 3 vs. group 1 (25.0% vs. 17.2%; p<0.001), and group 3 vs. group 2 (25.0% vs. 22.0%; P=0.008). After controlling for confounding factors, these three groups did not differ in LBR (group 1 vs. group 2, odds ratio [OR], 1.08; 95% confidence interval [CI], 0.83-1.4; P=0.54 and group 1 vs. group 3, OR, 1.16; 95% CI, 0.90-1.51; P=0.24).
Conclusion
Live birth rates in women with endometrial thickness between 7.0-9.9 mm were not affected by different cut-offs when blastocyst transfer was performed.
Keyword
Figure
Reference
-
References
1. Shakerian B, Turkgeldi E, Yildiz S, Keles I, Ata B. Endometrial thickness is not predictive for live birth after embryo transfer, even without a cutoff. Fertil Steril. 2021; 116:130–7.
Article2. Liu KE, Hartman M, Hartman A, Luo ZC, Mahutte N. The impact of a thin endometrial lining on fresh and frozenthaw IVF outcomes: an analysis of over 40 000 embryo transfers. Hum Reprod. 2018; 33:1883–8.
Article3. Yuan X, Saravelos SH, Wang Q, Xu Y, Li TC, Zhou C. Endometrial thickness as a predictor of pregnancy outcomes in 10787 fresh IVF-ICSI cycles. Reprod Biomed Online. 2016; 33:197–205.
Article4. Bu Z, Hu L, Su Y, Guo Y, Zhai J, Sun YP. Factors related to early spontaneous miscarriage during IVF/ICSI treatment: an analysis of 21,485 clinical pregnancies. Reprod Biomed Online. 2020; 40:201–6.5. Gao G, Cui X, Li S, Ding P, Zhang S, Zhang Y. Endometrial thickness and IVF cycle outcomes: a meta-analysis. Reprod Biomed Online. 2020; 40:124–33.
Article6. Bu Z, Sun Y. The impact of endometrial thickness on the day of human chorionic gonadotrophin (hCG) administration on ongoing pregnancy rate in patients with different ovarian response. PLoS One. 2015; 10:e0145703.
Article7. Richter KS, Bugge KR, Bromer JG, Levy MJ. Relationship between endometrial thickness and embryo implantation, based on 1,294 cycles of in vitro fertilization with transfer of two blastocyst-stage embryos. Fertil Steril. 2007; 87:53–9.
Article8. Gallos ID, Khairy M, Chu J, Rajkhowa M, Tobias A, Campbell A, et al. Optimal endometrial thickness to maximize live births and minimize pregnancy losses: analysis of 25,767 fresh embryo transfers. Reprod Biomed Online. 2018; 37:542–8.
Article9. Ma NZ, Chen L, Dai W, Bu ZQ, Hu LL, Sun YP. Influence of endometrial thickness on treatment outcomes following in vitro fertilization/intracytoplasmic sperm injection. Reprod Biol Endocrinol. 2017; 15:5.10. Liu C, Li Y, Jiang H, Liu Y, Song X. The clinical outcomes of fresh versus frozen embryos transfer in women ≥40 years with poor ovarian response. Obstet Gynecol Sci. 2021; 64:284–92.
Article11. El-Toukhy T, Coomarasamy A, Khairy M, Sunkara K, Seed P, Khalaf Y, et al. The relationship between endometrial thickness and outcome of medicated frozen embryo replacement cycles. Fertil Steril. 2008; 89:832–9.
Article12. Bu Z, Wang K, Dai W, Sun Y. Endometrial thickness significantly affects clinical pregnancy and live birth rates in frozen-thawed embryo transfer cycles. Gynecol Endocrinol. 2016; 32:524–8.
Article13. Mahutte N, Hartman M, Meng L, Lanes A, Luo ZC, Liu KE. Optimal endometrial thickness in fresh and frozenthaw in vitro fertilization cycles: an analysis of live birth rates from 96,000 autologous embryo transfers. Fertil Steril. 2022; 117:792–800.
Article14. Weissman A. Results: frozen-thawed embryo transfer [Internet]. Tel Aviv: IVF Worldwide;c2020. [cited 2022 Jul 5]. Available from: https://ivf-worldwide.com/survey/frozen-thawed-embryo-transfer/results-frozen-thawedembryo-transfer.html.15. Dahan MH, Agdi M, Shehata F, Son W, Tan SL. A comparison of outcomes from in vitro fertilization cycles stimulated with either recombinant luteinizing hormone (LH) or human chorionic gonadotropin acting as an LH analogue delivered as human menopausal gonadotropins, in subjects with good or poor ovarian reserve: a retrospective analysis. Eur J Obstet Gynecol Reprod Biol. 2014; 172:70–3.
Article16. Gardner DK, Surrey E, Minjarez D, Leitz A, Stevens J, Schoolcraft WB. Single blastocyst transfer: a prospective randomized trial. Fertil Steril. 2004; 81:551–5.
Article17. Vaegter KK, Lakic TG, Olovsson M, Berglund L, Brodin T, Holte J. Which factors are most predictive for live birth after in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) treatments? Analysis of 100 prospectively recorded variables in 8,400 IVF/ICSI single-embryo transfers. Fertil Steril. 2017; 107:641–8e2.18. Simeonov M, Sapir O, Lande Y, Ben-Haroush A, Oron G, Shlush E, et al. The entire range of trigger-day endometrial thickness in fresh IVF cycles is independently correlated with live birth rate. Reprod Biomed Online. 2020; 41:239–47.
Article19. De Geyter C, Schmitter M, De Geyter M, Nieschlag E, Holzgreve W, Schneider HP. Prospective evaluation of the ultrasound appearance of the endometrium in a cohort of 1,186 infertile women. Fertil Steril. 2000; 73:106–13.20. Groenewoud ER, Cohlen BJ, Al-Oraiby A, Brinkhuis EA, Broekmans FJM, de Bruin JP, et al. Influence of endometrial thickness on pregnancy rates in modified natural cycle frozen-thawed embryo transfer. Acta Obstet Gynecol Scand. 2018; 97:808–15.
Article21. Weissman A, Gotlieb L, Casper RF. The detrimental effect of increased endometrial thickness on implantation and pregnancy rates and outcome in an in vitro fertilization program. Fertil Steril. 1999; 71:147–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Endometrial Thickness and Pattern in Ovum Donation and Cryopreserved - Thawed Embryo Transfer Program
- Reproductive outcomes of retransferring retained embryos in blastocyst transfer cycles
- The effect of embryo catheter loading technique on the live birth rate
- A Case of Congenital Diaphragmatic Hernia that Occurred Following In Vitro Fertilization and Embryo Transfer
- Blastocyst Transfer Ameliorates Live Birth Rate Compared with Cleavage-Stage Embryos Transfer in Fresh In Vitro Fertilization or Intracytoplasmic Sperm Injection Cycles: Reviews and Meta-Analysis