J Cerebrovasc Endovasc Neurosurg.
2024 Sep;26(3):274-283. 10.7461/jcen.2024.E2023.11.001.
Contributing factors of spontaneous intracerebral hemorrhage development in young adults
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Neurosurgery, Chung-Ang University Hospital, Seoul, Korea
- KMID: 2559437
- DOI: http://doi.org/10.7461/jcen.2024.E2023.11.001
Abstract
Objective
The incidence of spontaneous intracerebral hemorrhage (ICH) in young people is relatively low; however, it leads to devastating lifelong neurologic deficits. We focused on spontaneous ICH occurring in young adults between 30 and 50 years of age.
Methods
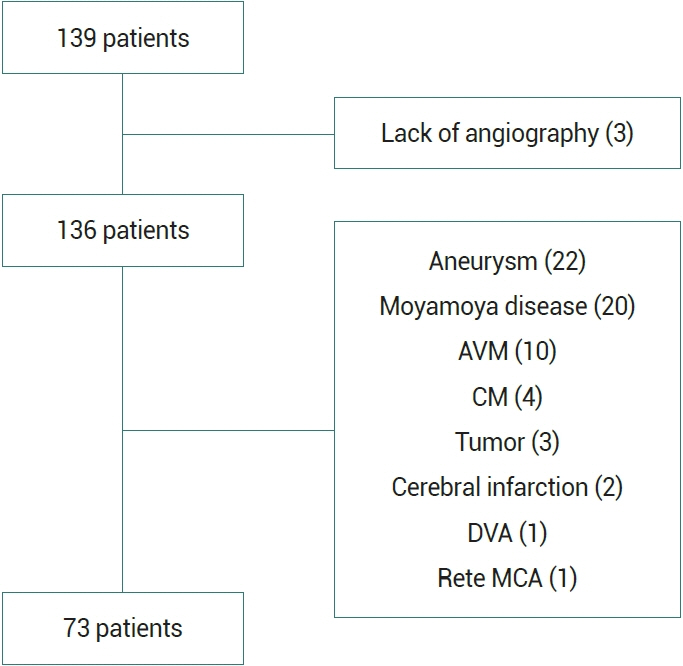
We retrospectively reviewed the records of 139 patients, aged 30–50 years, diagnosed with spontaneous ICH between 2011 and 2021. Cases of ICH attributable to discernible causative lesions were excluded. Demographic data, laboratory results, image findings, and clinical outcome were analyzed.
Results
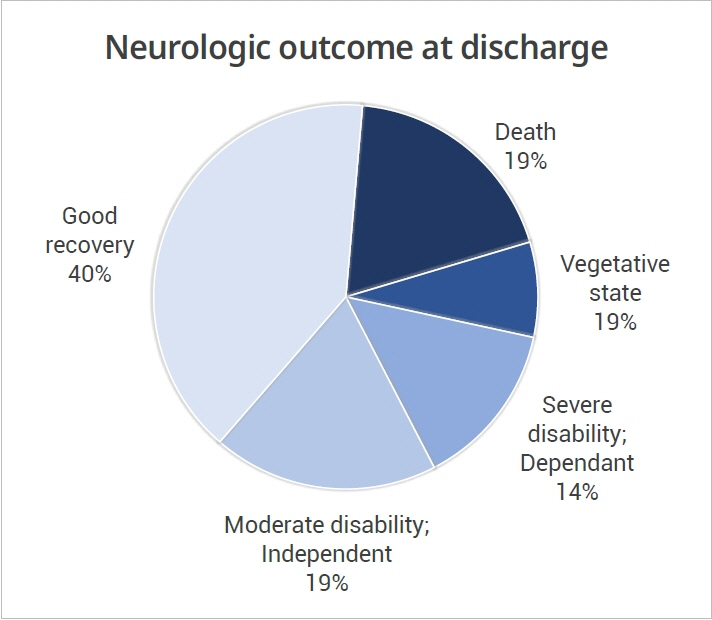
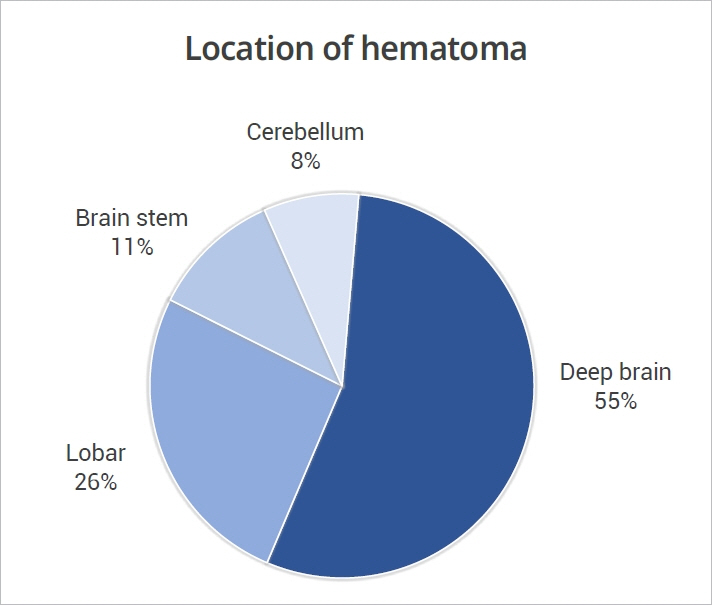
After exclusions, 73 patients were included in this study. Common characteristics among the study patients included male sex (83.6%), high body mass index (>25 kg/m2, 45.8%), smoking history (47.2%), heavy alcohol consumption (30.6%), previously diagnosed hypertension (41.1%), high serum triglyceride level (>150 mg/dL, 33.3%), and microbleeds or white matter changes observed on magnetic resonance images (51.3%). In the multivariate analysis, previously diagnosed hypertension was the sole significant risk factor for cerebral small vessel (OR 7.769, P=0.031). Age, brain stem location, Glasgow Coma Scale score at admission, and hematoma volume were associated with poor outcomes.
Conclusions
Hypertension, obesity, smoking, and cerebral small vessel disease were important factors associated with non-lesional spontaneous intracerebral hemorrhage in young patients. Radiologic changes corresponding to cerebral small vessel disease appeared in young patients (in their 30s) and they were associated with hypertension.
Figure
Reference
-
1. An SJ, Kim TJ, Yoon BW. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: An update. J Stroke. 2017; Jan. 19(1):3–10.
Article2. Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-touse predictor of 30-day mortality. Stroke. 1993; Jul. 24(7):987–93.
Article3. Brott T, Broderick J, Kothari R, Barsan W, Tomsick T, Sauerbeck L, et al. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke. 1997; Jan. 28(1):1–5.
Article4. Bukhari S, Yaghi S, Bashir Z. Stroke in young adults. J Clin Med. 2023; Jul. 29. 12(15):49999.
Article5. Charidimou A, Jäger HR. Developing biomarkers for cerebral amyloid angiopathy trials: do potential disease phenotypes hold promise? Lancet Neurol. 2014; Jun. 13(6):538–40.6. Chen CY, Lin PT, Wang YH, Syu RW, Hsu SL, Chang LH, et al. Etiology and risk factors of intracranial hemorrhage and ischemic stroke in young adults. J Chin Med Assoc. 2021; Oct. 84(10):930–6.
Article7. Cuadrado-Godia E, Dwivedi P, Sharma S, Ois Santiago A, Roquer Gonzalez J, Balcells M, et al. Cerebral small vessel disease: A review focusing on pathophysiology, biomarkers, and machine learning strategies. J Stroke. 2018; Sep. 20(3):302–20.
Article8. Elmegiri M, Koivunen RJ, Tatlisumak T, Putaala J, Martola J. MRI characterization of non-traumatic intracerebral hemorrhage in young adults. Front Neurol. 2020; Oct. 29. 11:558680.
Article9. Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987; Aug. 149(2):351–6.
Article10. Hinton TC, Adams ZH, Baker RP, Hope KA, Paton JFR, Hart EC, et al. Investigation and treatment of high blood pressure in young people: Too much medicine or appropriate risk reduction? Hypertension. 2020; Jan. 75(1):16–22.11. Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975; Mar. 1(7905):480–4.12. Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996; Aug. 27(8):1304–5.
Article13. Mailles A, De Broucker T, Costanzo P, Martinez-Almoyna L, Vaillant V, Stahl JP. Long-term outcome of patients presenting with acute infectious encephalitis of various causes in France. Clin Infect Dis. 2012; May. 54(10):1455–64.
Article14. Norrving B. Evolving concept of small vessel disease through advanced brain imaging. J Stroke. 2015; May. 17(2):94–100.
Article15. Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010; Jul. 9(7):689–701.16. Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001; May. 344(19):1450–60.
Article17. Ruíz-Sandoval JL, Cantú C, Barinagarrementeria F. Intracerebral hemorrhage in young people: analysis of risk factors, location, causes, and prognosis. Stroke. 1999; Mar. 30(3):537–41.18. Smajlović D. Strokes in young adults: epidemiology and prevention. Vasc Health Risk Manag. 2015; Feb. 11:157–64.19. Sundström J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: Cohort study of Swedish male conscripts. BMJ. 2011; Feb. 22. 342:d643.
Article20. van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010; Feb. 9(2):167–76.21. Yano Y, Reis JP, Colangelo LA, Shimbo D, Viera AJ, Allen NB, et al. Association of blood pressure classification in young adults using the 2017 American college of cardiology/American heart association blood pressure guideline with cardiovascular events later in life. JAMA. 2018; Nov. 6. 320(17):1774–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Spontaneous Intracerebral Hematoma without Presenting Risk Factors
- Computed Tomographic Findings and Clinical Observation of Spontaneous Intracerebral Hemorrhage
- The Outcomes of Spontaneous Intracerebral Hemorrhage in Young Adults - A Clinical Study
- A Case of Spontaneous Intracerebral Hematoma in Childhood
- Clinical Analysis of Stereotactic aspiration in the Management of Spontaneous Intracerebral Hemorrhage