Clin Endosc.
2024 Sep;57(5):656-665. 10.5946/ce.2023.244.
Puncture angle on an endoscopic ultrasound image is independently associated with unsuccessful guidewire manipulation of endoscopic ultrasound-guided hepaticogastrostomy: a retrospective study in Japan
- Affiliations
-
- 1Department of Medicine and Bioregulatory Science, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan
- 2Department of Gastroenterology, Clinical Research Institute, National Hospital Organization Kyushu Medical Center, Fukuoka, Japan
- KMID: 2559217
- DOI: http://doi.org/10.5946/ce.2023.244
Abstract
- Background/Aims
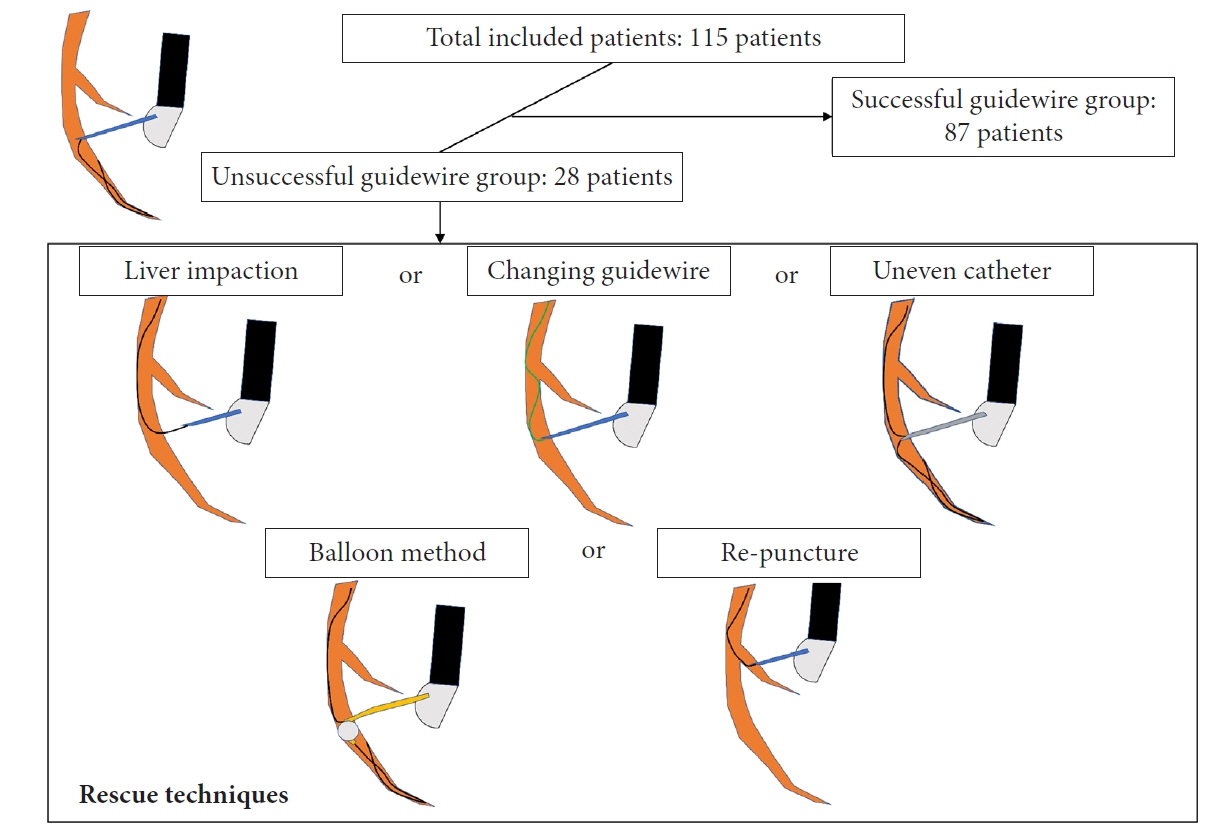
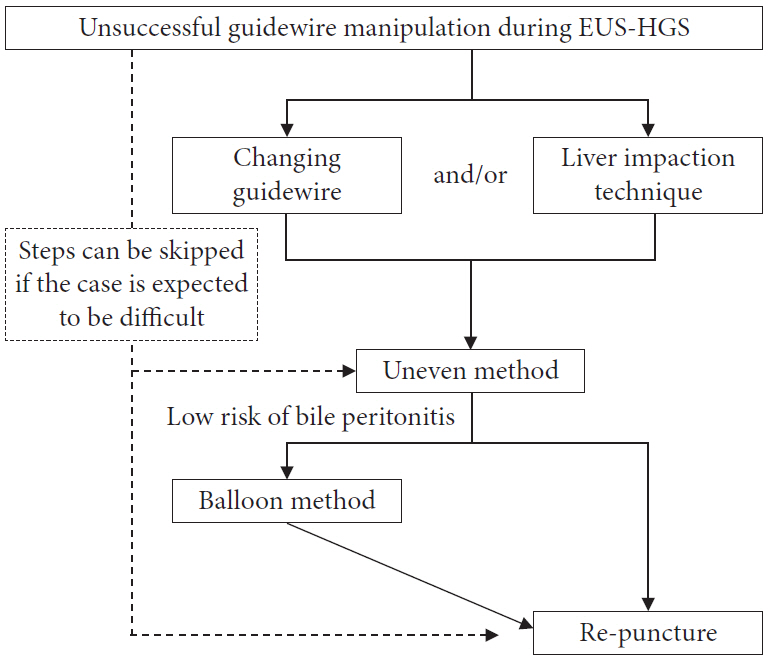
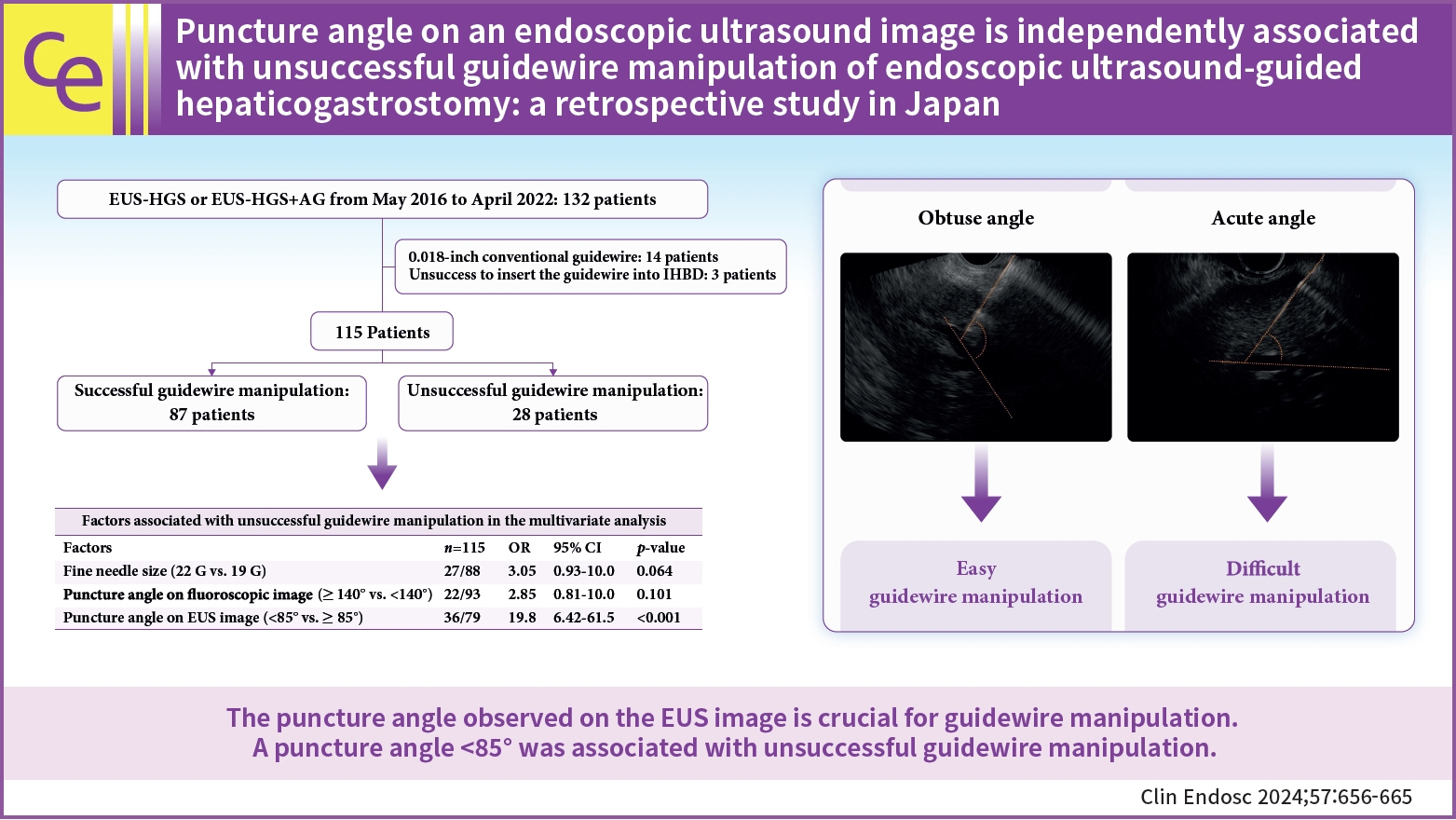
Although endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) is performed globally, the procedure remains challenging. Guidewire manipulation is the most difficult step, and there are few reports on the factors associated with unsuccessful guidewire manipulation. This study aimed to assess the significance of the puncture angle on EUS images and identify the most effective guidewire rescue method for patients with unsuccessful guidewire manipulation.
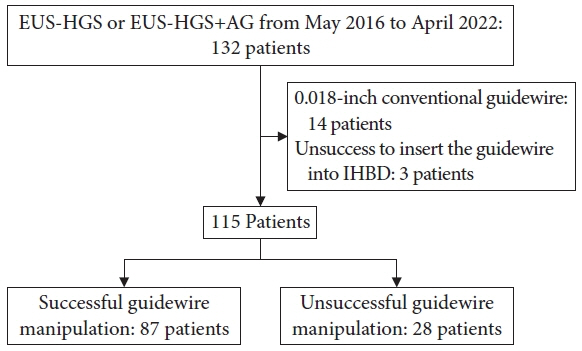
Methods
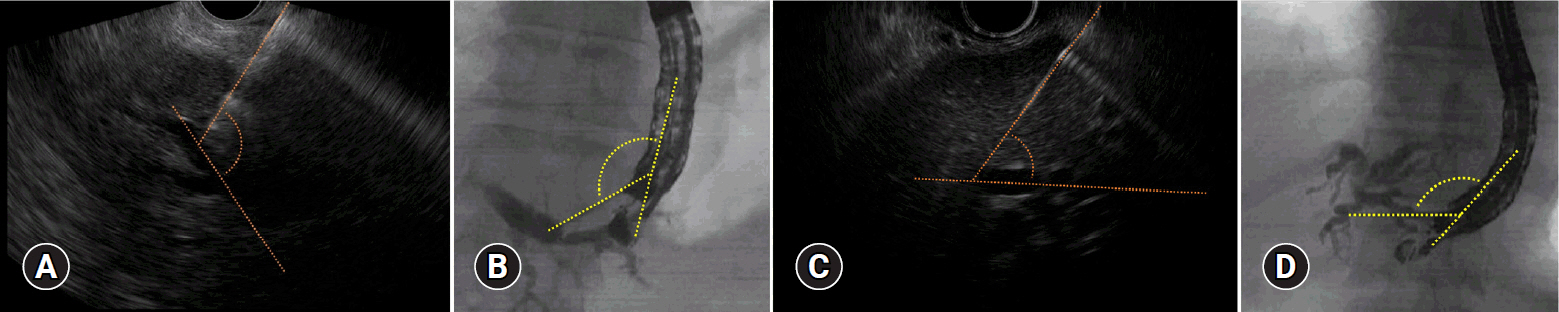
We retrospectively enrolled 115 patients who underwent EUS-HGS between May 2016 and April 2022 at two centers. The puncture angle between the needle and the intrahepatic bile duct was measured through EUS movie records.
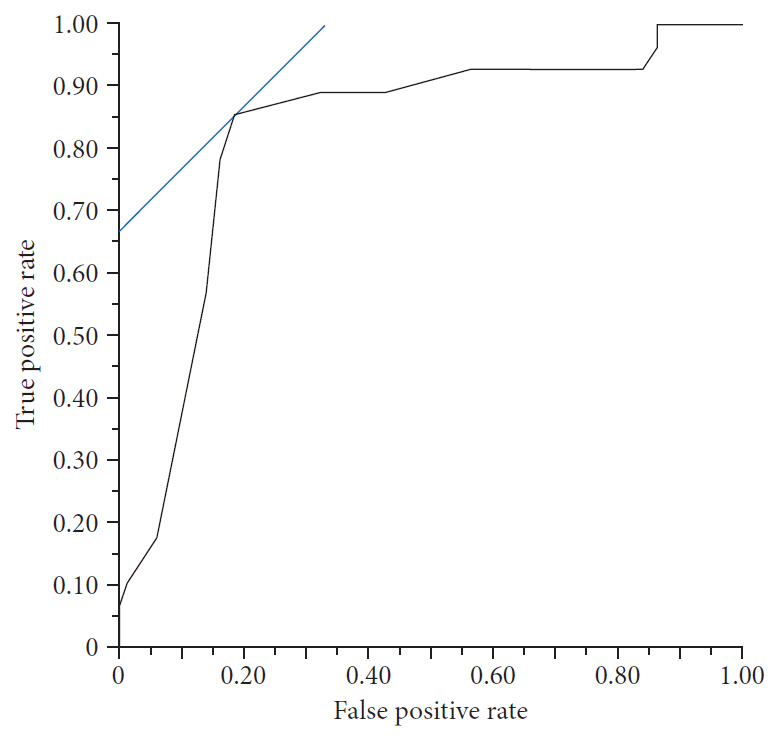
Results
Guidewire manipulation was unsuccessful in 28 patients. Receiver operating characteristic (ROC) curves identified an optimal puncture angle cutoff value of 85° (cutoff value, 85°; area under the ROC curve, 0.826; sensitivity, 85.7%; specificity, 81.6%). Multivariate analysis demonstrated that a puncture angle <85° was a significant risk factor for unsuccessful guidewire manipulation (odds ratio, 19.8; 95% confidence interval, 6.42–61.5; p<0.001). Among the 28 unsuccessful cases, 24 patients (85.7%) achieved successful guidewire manipulation using various rescue methods.
Conclusions
The puncture angle observed on EUS is crucial for guidewire manipulation. A puncture angle of <85° was associated with unsuccessful guidewire manipulation.
Figure
Reference
-
1. Lee TH, Choi JH, Park do H, et al. Similar efficacies of endoscopic ultrasound-guided transmural and percutaneous drainage for malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2016; 14:1011–1019.2. Sharaiha RZ, Khan MA, Kamal F, et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017; 85:904–914.3. Artifon EL, Marson FP, Gaidhane M, et al. Hepaticogastrostomy or choledochoduodenostomy for distal malignant biliary obstruction after failed ERCP: is there any difference? Gastrointest Endosc. 2015; 81:950–959.4. Uemura RS, Khan MA, Otoch JP, et al. EUS-guided choledochoduodenostomy versus hepaticogastrostomy: a systematic review and meta-analysis. J Clin Gastroenterol. 2018; 52:123–130.5. Wang K, Zhu J, Xing L, et al. Assessment of efficacy and safety of EUS-guided biliary drainage: a systematic review. Gastrointest Endosc. 2016; 83:1218–1227.6. Khan MA, Akbar A, Baron TH, et al. Endoscopic ultrasound-guided biliary drainage: a systematic review and meta-analysis. Dig Dis Sci. 2016; 61:684–703.7. Moole H, Bechtold ML, Forcione D, et al. A meta-analysis and systematic review: success of endoscopic ultrasound guided biliary stenting in patients with inoperable malignant biliary strictures and a failed ERCP. Medicine (Baltimore). 2017; 96:e5154.8. Vila JJ, Pérez-Miranda M, Vazquez-Sequeiros E, et al. Initial experience with EUS-guided cholangiopancreatography for biliary and pancreatic duct drainage: a Spanish national survey. Gastrointest Endosc. 2012; 76:1133–1141.9. Ogura T, Nishioka N, Ueno S, et al. Effect of echoendoscope angle on success of guidewire manipulation during endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2021; 53:369–375.10. Ogura T, Masuda D, Takeuchi T, et al. Liver impaction technique to prevent shearing of the guidewire during endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2015; 47(S 01):E583–E584.11. Kawakami H, Kubota Y, Makiyama H, et al. Uneven double-lumen cannula for rescue guidewire technique in endoscopic ultrasonography-guided hepaticogastrostomy. Endoscopy. 2017; 49:E264–E265.12. Ohno A, Kaku T, Fujimori N. Balloon guidewire technique during EUS-guided hepaticogastrostomy. Endosc Ultrasound. 2022; 11:330–331.13. Ohno A, Fujimori N, Kaku T, et al. Feasibility and efficacy of endoscopic ultrasound-guided hepaticogastrostomy without dilation: a propensity score matching analysis. Dig Dis Sci. 2022; 67:5676–5684.14. Ogura T, Okuda A, Ueno S, et al. Prospective comparison study between 19-gauge needle with .025-inch guidewire and 22-gauge needle with novel .018-inch guidewire during EUS-guided transhepatic biliary drainage (with video). Gastrointest Endosc. 2022; 96:262–268.15. Hara K, Okuno N, Haba S, et al. How to perform EUS-guided hepaticogastrostomy easier and safer. J Hepatobiliary Pancreat Sci. 2020; 27:563–564.16. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.17. Isayama H, Hamada T, Yasuda I, et al. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015; 27:259–264.18. Oh D, Park DH, Song TJ, et al. Optimal biliary access point and learning curve for endoscopic ultrasound-guided hepaticogastrostomy with transmural stenting. Therap Adv Gastroenterol. 2017; 10:42–53.19. Fugazza A, Colombo M, Spadaccini M, et al. Relief of jaundice in malignant biliary obstruction: when should we consider endoscopic ultrasonography-guided hepaticogastrostomy as an option? Hepatobiliary Pancreat Dis Int. 2022; 21:234–240.20. Matsubara S, Nakagawa K, Suda K, et al. Practical tips for safe and successful endoscopic ultrasound-guided hepaticogastrostomy: a state-of-the-art technical review. J Clin Med. 2022; 11:1591.21. Ueno S, Ogura T, Higuchi K. Moving scope technique for guidewire insertion during endoscopic ultrasound-guided hepaticogastrostomy. Dig Endosc. 2021; 33:e109–e110.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Technical Review of Developments in Endoscopic Ultrasound-Guided Hepaticogastrostomy
- Shearing of guidewire coating by the tip of the electrocautery dilator during endoscopic ultrasound-guided gallbladder drainage
- Endoscopic Ultrasound-Guided Hepaticogastrostomy: Technical Review and Tips to Prevent Adverse Events
- Recent development of endoscopic ultrasound-guided biliary drainage
- Technical tips for endoscopic ultrasound-guided pancreatic duct access and drainage