Clin Endosc.
2024 Sep;57(5):571-580. 10.5946/ce.2023.160.
Endoscopic stenting for malignant gastric outlet obstruction: focusing on comparison of endoscopic stenting and surgical gastrojejunostomy
- Affiliations
-
- 1Department of Gastroenterology, Ajou University School of Medicine, Suwon, Korea
- 2Center for Gastric Cancer, National Cancer Center, Goyang, Korea
- KMID: 2559205
- DOI: http://doi.org/10.5946/ce.2023.160
Abstract
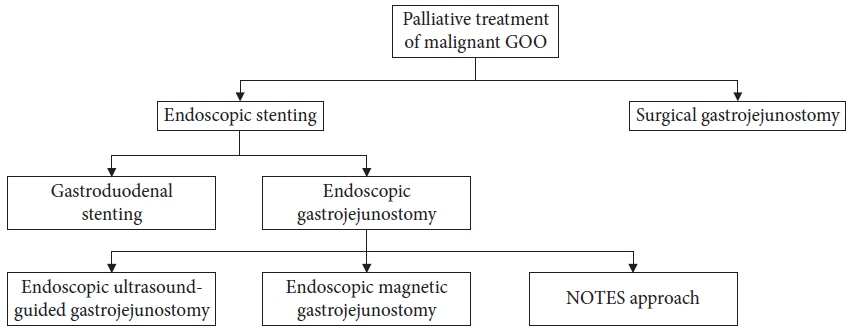
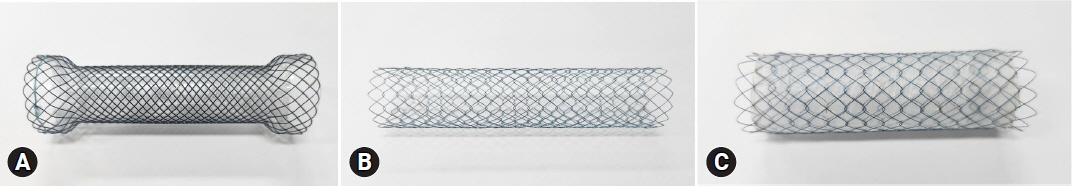
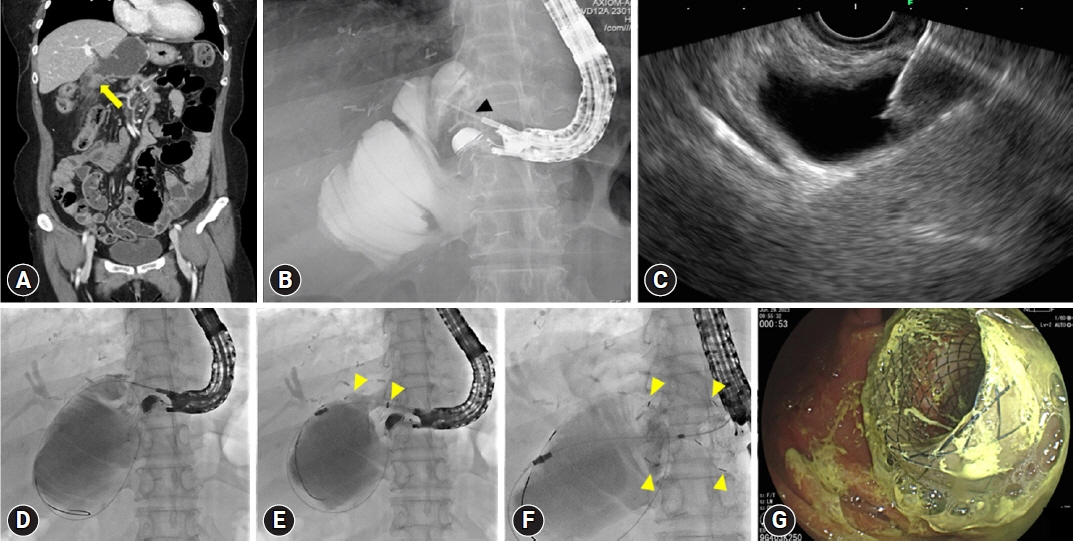
- Malignant gastric outlet obstruction (GOO) is a condition characterized by blockage or narrowing where the stomach empties its contents into the small intestine due to primary malignant tumors or metastatic diseases. This condition leads to various symptoms such as nausea, vomiting, abdominal pain, and weight loss. To manage malignant GOO, different treatment options have been employed, including surgical gastrojejunostomy (SGJ), gastroduodenal stenting (GDS) using self-expandable metallic stent (SEMS), and endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ). This review focuses on comparing the clinical outcomes of endoscopic stenting (GDS and EUS-GJ) with SGJ for malignant GOO. Studies have shown that GDS with SEMS provides comparable clinical outcomes and safety for the palliation of obstructive symptoms. The choice between covered and uncovered SEMS remains controversial, as different studies have reported varying results. EUS-GJ, performed via endoscopic ultrasound guidance, has shown promising efficacy and safety in managing malignant GOO, but further studies are needed to establish it as the primary treatment option. Comparative analyses suggest that GDS has higher recurrence and reintervention rates compared to EUS-GJ and SGJ, with similar overall procedural complications. However, bleeding rates were lower with GDS than with SGJ. Randomized controlled trials are required to determine the optimal treatment approach for malignant GOO.
Keyword
Figure
Reference
-
1. Chekan EG, Clark L, Wu J, et al. Laparoscopic biliary and enteric bypass. Semin Surg Oncol. 1999; 16:313–320.2. Mintziras I, Miligkos M, Wächter S, et al. Palliative surgical bypass is superior to palliative endoscopic stenting in patients with malignant gastric outlet obstruction: systematic review and meta-analysis. Surg Endosc. 2019; 33:3153–3164.3. Itoi T, Ishii K, Ikeuchi N, et al. Prospective evaluation of endoscopic ultrasonography-guided double-balloon-occluded gastrojejunostomy bypass (EPASS) for malignant gastric outlet obstruction. Gut. 2016; 65:193–195.4. Tyberg A, Perez-Miranda M, Sanchez-Ocaña R, et al. Endoscopic ultrasound-guided gastrojejunostomy with a lumen-apposing metal stent: a multicenter, international experience. Endosc Int Open. 2016; 4:E276–E281.5. Cheung SL, Teoh AY. Optimal management of gastric outlet obstruction in unresectable malignancies. Gut Liver. 2022; 16:190–197.6. Krishnamoorthi R, Bomman S, Benias P, et al. Efficacy and safety of endoscopic duodenal stent versus endoscopic or surgical gastrojejunostomy to treat malignant gastric outlet obstruction: systematic review and meta-analysis. Endosc Int Open. 2022; 10:E874–E897.7. Medina-Franco H, Abarca-Pérez L, España-Gómez N, et al. Morbidity-associated factors after gastrojejunostomy for malignant gastric outlet obstruction. Am Surg. 2007; 73:871–875.8. Wong YT, Brams DM, Munson L, et al. Gastric outlet obstruction secondary to pancreatic cancer: surgical vs endoscopic palliation. Surg Endosc. 2002; 16:310–312.9. Yim HB, Jacobson BC, Saltzman JR, et al. Clinical outcome of the use of enteral stents for palliation of patients with malignant upper GI obstruction. Gastrointest Endosc. 2001; 53:329–332.10. Del Piano M, Ballarè M, Montino F, et al. Endoscopy or surgery for malignant GI outlet obstruction? Gastrointest Endosc. 2005; 61:421–426.11. Jeurnink SM, Steyerberg EW, van Hooft JE, et al. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010; 71:490–499.12. Zheng B, Wang X, Ma B, et al. Endoscopic stenting versus gastrojejunostomy for palliation of malignant gastric outlet obstruction. Dig Endosc. 2012; 24:71–78.13. Jeurnink SM, van Eijck CH, Steyerberg EW, et al. Stent versus gastrojejunostomy for the palliation of gastric outlet obstruction: a systematic review. BMC Gastroenterol. 2007; 7:18.14. Kang HW, Kim SG. Upper gastrointestinal stent insertion in malignant and benign disorders. Clin Endosc. 2015; 48:187–193.15. Lim SG, Kim JH, Lee KM, et al. Conformable covered versus uncovered self-expandable metallic stents for palliation of malignant gastroduodenal obstruction: a randomized prospective study. Dig Liver Dis. 2014; 46:603–608.16. Kim CG, Choi IJ, Lee JY, et al. Covered versus uncovered self-expandable metallic stents for palliation of malignant pyloric obstruction in gastric cancer patients: a randomized, prospective study. Gastrointest Endosc. 2010; 72:25–32.17. Maetani I, Mizumoto Y, Shigoka H, et al. Placement of a triple-layered covered versus uncovered metallic stent for palliation of malignant gastric outlet obstruction: a multicenter randomized trial. Dig Endosc. 2014; 26:192–199.18. Lee H, Min BH, Lee JH, et al. Covered metallic stents with an anti-migration design vs. uncovered stents for the palliation of malignant gastric outlet obstruction: a multicenter, randomized trial. Am J Gastroenterol. 2015; 110:1440–1449.19. van Hooft J, Mutignani M, Repici A, et al. First data on the palliative treatment of patients with malignant gastric outlet obstruction using the WallFlex enteral stent: a retrospective multicenter study. Endoscopy. 2007; 39:434–439.20. van Hooft JE, Uitdehaag MJ, Bruno MJ, et al. Efficacy and safety of the new WallFlex enteral stent in palliative treatment of malignant gastric outlet obstruction (DUOFLEX study): a prospective multicenter study. Gastrointest Endosc. 2009; 69:1059–1066.21. Havemann MC, Adamsen S, Wøjdemann M. Malignant gastric outlet obstruction managed by endoscopic stenting: a prospective single-centre study. Scand J Gastroenterol. 2009; 44:248–251.22. Kim YW, Choi CW, Kang DH, et al. A double-layered (comvi) self-expandable metal stent for malignant gastroduodenal obstruction: a prospective multicenter study. Dig Dis Sci. 2011; 56:2030–2036.23. Isayama H, Sasaki T, Nakai Y, et al. Management of malignant gastric outlet obstruction with a modified triple-layer covered metal stent. Gastrointest Endosc. 2012; 75:757–763.24. Sasaki T, Isayama H, Maetani I, et al. Japanese multicenter estimation of WallFlex duodenal stent for unresectable malignant gastric outlet obstruction. Dig Endosc. 2013; 25:1–6.25. van den Berg MW, Haijtink S, Fockens P, et al. First data on the evolution duodenal stent for palliation of malignant gastric outlet obstruction (DUOLUTION study): a prospective multicenter study. Endoscopy. 2013; 45:174–181.26. Jung K, Ahn JY, Jung HY, et al. Outcomes of endoscopically inserted self-expandable metal stents in malignancy according to the type of stent and the site of obstruction. Surg Endosc. 2016; 30:4001–4010.27. Hori Y, Naitoh I, Hayashi K, et al. Predictors of outcomes in patients undergoing covered and uncovered self-expandable metal stent placement for malignant gastric outlet obstruction: a multicenter study. Gastrointest Endosc. 2017; 85:340–348.28. Lee KM, Choi SJ, Shin SJ, et al. Palliative treatment of malignant gastroduodenal obstruction with metallic stent: prospective comparison of covered and uncovered stents. Scand J Gastroenterol. 2009; 44:846–852.29. Park KB, Do YS, Kang WK, et al. Malignant obstruction of gastric outlet and duodenum: palliation with flexible covered metallic stents. Radiology. 2001; 219:679–683.30. Seo EH, Jung MK, Park MJ, et al. Covered expandable nitinol stents for malignant gastroduodenal obstructions. J Gastroenterol Hepatol. 2008; 23(7 Pt 1):1056–1062.31. Tringali A, Costa D, Anderloni A, et al. Covered versus uncovered metal stents for malignant gastric outlet obstruction: a systematic review and meta-analysis. Gastrointest Endosc. 2020; 92:1153–1163.32. Shi D, Ji F, Bao YS, et al. A multicenter randomized controlled trial of malignant gastric outlet obstruction: tailored partially covered stents (placed fluoroscopically) versus standard uncovered stents (placed endoscopically). Gastroenterol Res Pract. 2014; 2014:309797.33. Park CI, Kim JH, Lee YC, et al. What is the ideal stent as initial intervention for malignant gastric outlet obstruction? Dig Liver Dis. 2013; 45:33–37.34. Telford JJ, Carr-Locke DL, Baron TH, et al. Palliation of patients with malignant gastric outlet obstruction with the enteral Wallstent: outcomes from a multicenter study. Gastrointest Endosc. 2004; 60:916–920.35. Kim JH, Song HY, Shin JH, et al. Metallic stent placement in the palliative treatment of malignant gastroduodenal obstructions: prospective evaluation of results and factors influencing outcome in 213 patients. Gastrointest Endosc. 2007; 66:256–264.36. Cho YK, Kim SW, Hur WH, et al. Clinical outcomes of self-expandable metal stent and prognostic factors for stent patency in gastric outlet obstruction caused by gastric cancer. Dig Dis Sci. 2010; 55:668–674.37. Kim CG, Park SR, Choi IJ, et al. Effect of chemotherapy on the outcome of self-expandable metallic stents in gastric cancer patients with malignant outlet obstruction. Endoscopy. 2012; 44:807–812.38. Swain CP, Mills TN. Anastomosis at flexible endoscopy: an experimental study of compression button gastrojejunostomy. Gastrointest Endosc. 1991; 37:628–631.39. Kantsevoy SV, Jagannath SB, Niiyama H, et al. Endoscopic gastrojejunostomy with survival in a porcine model. Gastrointest Endosc. 2005; 62:287–292.40. Bergström M, Ikeda K, Swain P, et al. Transgastric anastomosis by using flexible endoscopy in a porcine model (with video). Gastrointest Endosc. 2006; 63:307–312.41. Chopita N, Vaillaverde A, Cope C, et al. Endoscopic gastroenteric anastomosis using magnets. Endoscopy. 2005; 37:313–317.42. van Hooft JE, Vleggaar FP, Le Moine O, et al. Endoscopic magnetic gastroenteric anastomosis for palliation of malignant gastric outlet obstruction: a prospective multicenter study. Gastrointest Endosc. 2010; 72:530–535.43. Ryou M, Cantillon-Murphy P, Azagury D, et al. Smart Self-Assembling MagnetS for ENdoscopy (SAMSEN) for transoral endoscopic creation of immediate gastrojejunostomy (with video). Gastrointest Endosc. 2011; 73:353–359.44. Song TJ, Seo DW, Kim SH, et al. Endoscopic gastrojejunostomy with a natural orifice transluminal endoscopic surgery technique. World J Gastroenterol. 2013; 19:3447–3452.45. Yi SW, Chung MJ, Jo JH, et al. Gastrojejunostomy by pure natural orifice transluminal endoscopic surgery using a newly designed anastomosing metal stent in a porcine model. Surg Endosc. 2014; 28:1439–1446.46. Chen YI, Itoi T, Baron TH, et al. EUS-guided gastroenterostomy is comparable to enteral stenting with fewer re-interventions in malignant gastric outlet obstruction. Surg Endosc. 2017; 31:2946–2952.47. Ge PS, Young JY, Dong W, et al. EUS-guided gastroenterostomy versus enteral stent placement for palliation of malignant gastric outlet obstruction. Surg Endosc. 2019; 33:3404–3411.48. Kerdsirichairat T, Irani S, Yang J, et al. Durability and long-term outcomes of direct EUS-guided gastroenterostomy using lumen-apposing metal stents for gastric outlet obstruction. Endosc Int Open. 2019; 7:E144–E150.49. Kastelijn JB, Moons LM, Garcia-Alonso FJ, et al. Patency of endoscopic ultrasound-guided gastroenterostomy in the treatment of malignant gastric outlet obstruction. Endosc Int Open. 2020; 8:E1194–E1201.50. Xu G, Shen Y, Lv Y, et al. Safety and efficacy of endoscopic ultrasound-guided gastroenterostomy using double balloon occlusion methods: a clinical retrospective study in 36 patients with malignant gastric outlet obstruction. Endosc Int Open. 2020; 8:E1690–E1697.51. Hindryckx P, Degroote H. Lumen-apposing metal stents for approved and off-label indications: a single-centre experience. Surg Endosc. 2021; 35:6013–6020.52. Kouanda A, Binmoeller K, Hamerski C, et al. Endoscopic ultrasound-guided gastroenterostomy versus open surgical gastrojejunostomy: clinical outcomes and cost effectiveness analysis. Surg Endosc. 2021; 35:7058–7067.53. Khashab MA, Bukhari M, Baron TH, et al. International multicenter comparative trial of endoscopic ultrasonography-guided gastroenterostomy versus surgical gastrojejunostomy for the treatment of malignant gastric outlet obstruction. Endosc Int Open. 2017; 5:E275–E281.54. Perez-Miranda M, Tyberg A, Poletto D, et al. EUS-guided gastrojejunostomy versus laparoscopic gastrojejunostomy: an international collaborative study. J Clin Gastroenterol. 2017; 51:896–899.55. Tonozuka R, Tsuchiya T, Mukai S, et al. Endoscopic ultrasonography-guided gastroenterostomy techniques for treatment of malignant gastric outlet obstruction. Clin Endosc. 2020; 53:510–518.56. Rizzo GE, Carrozza L, Quintini D, et al. A systematic review of endoscopic treatments for concomitant malignant biliary obstruction and malignant gastric outlet obstruction and the outstanding role of endoscopic ultrasound-guided therapies. Cancers (Basel). 2023; 15:2585.57. Fiori E, Lamazza A, Volpino P, et al. Palliative management of malignant antro-pyloric strictures: gastroenterostomy vs. endoscopic stenting: a randomized prospective trial. Anticancer Res. 2004; 24:269–271.58. Maetani I, Akatsuka S, Ikeda M, et al. Self-expandable metallic stent placement for palliation in gastric outlet obstructions caused by gastric cancer: a comparison with surgical gastrojejunostomy. J Gastroenterol. 2005; 40:932–937.59. Espinel J, Sanz O, Vivas S, et al. Malignant gastrointestinal obstruction: endoscopic stenting versus surgical palliation. Surg Endosc. 2006; 20:1083–1087.60. Keymling M, Wagner HJ, Vakil N, et al. Relief of malignant duodenal obstruction by percutaneous insertion of a metal stent. Gastrointest Endosc. 1993; 39:439–441.61. Mosler P, Mergener KD, Brandabur JJ, et al. Palliation of gastric outlet obstruction and proximal small bowel obstruction with self-expandable metal stents: a single center series. J Clin Gastroenterol. 2005; 39:124–128.62. ASGE Standards of Practice Committee, Jue TL, Storm AC, et al. ASGE guideline on the role of endoscopy in the management of benign and malignant gastroduodenal obstruction. Gastrointest Endosc. 2021; 93:309–322.63. Şentürk H, Köker İH, Koçhan K, et al. Endoscopic ultrasound-guided gastrojejunostomy with a direct technique without previous intestinal filling using a tubular fully covered self-expandable metallic stent. Clin Endosc. 2024; 57:209–216.64. Vedantam S, Shah R, Bhalla S, et al. No difference in outcomes with 15 mm vs. 20 mm lumen-apposing metal stents for endoscopic ultrasound-guided gastroenterostomy for gastric outlet obstruction: a meta-analysis. Clin Endosc. 2023; 56:298–307.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal Management of Gastric Outlet Obstruction in Unresectable Malignancies
- Palliative Management of Gastric Cancer with Outlet Obstruction: Stent versus Bypass
- Percutaneous transhepatic access to allow per-oral enteric stent insertion for malignant duodenal obstruction following failed endoscopic attempt
- Treatment Strategies for Gastric Cancer Patients with Gastric Outlet Obstruction
- Recent developments in endoscopic ultrasonography-guided gastroenterostomy