Clin Exp Otorhinolaryngol.
2024 Aug;17(3):253-262. 10.21053/ceo.2024.00157.
The Search for an Ideal Definitive Treatment of Sinonasal Squamous Cell Carcinoma With Orbit Invasion
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Chungnam National University Sejong Hospital, Sejong, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2558842
- DOI: http://doi.org/10.21053/ceo.2024.00157
Abstract
Objectives
. Sinonasal squamous cell carcinoma (SqCC) often invades the orbit. The treatment approach for sinonasal cancer that has spread to the orbit varies across medical centers and depends on the extent of the invasion. The decision to preserve the orbit in the treatment strategy is made on a case-by-case basis and results in varying outcomes. Currently, a multimodal treatment regimen, which may include surgery, chemotherapy, radiotherapy (RT), or concurrent chemoradiotherapy (CCRT), is commonly adopted for managing sinonasal cancers. This study aims to assess the prognosis of sinonasal SqCC with orbital invasion from various perspectives.
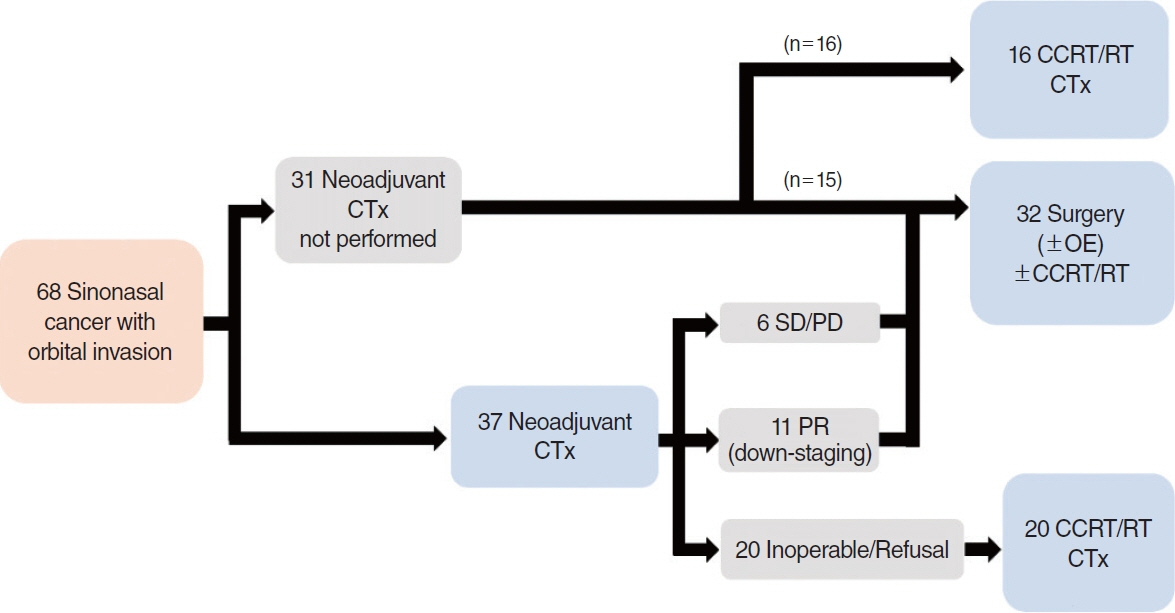
Methods
. We conducted a retrospective review of patients with primary sinonasal SqCC invading the orbit who were treated at Seoul National University Hospital and Seoul National University Bundang Hospital between 2009 and 2018. The extent of the tumor, orbital invasion, treatment strategies, recurrence rates, and survival rates were analyzed.
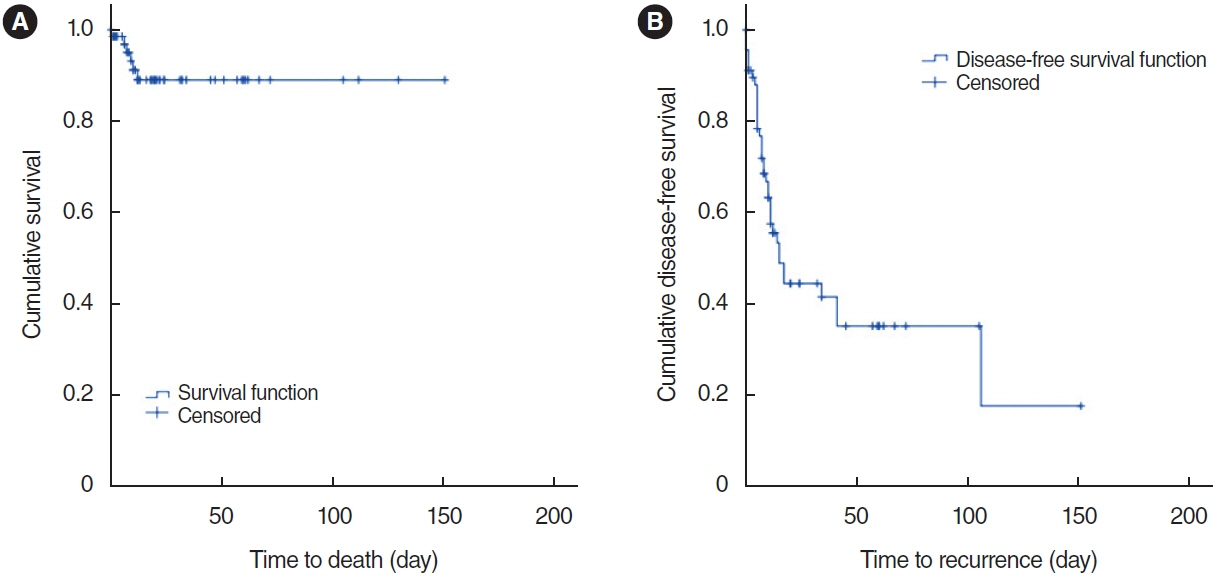
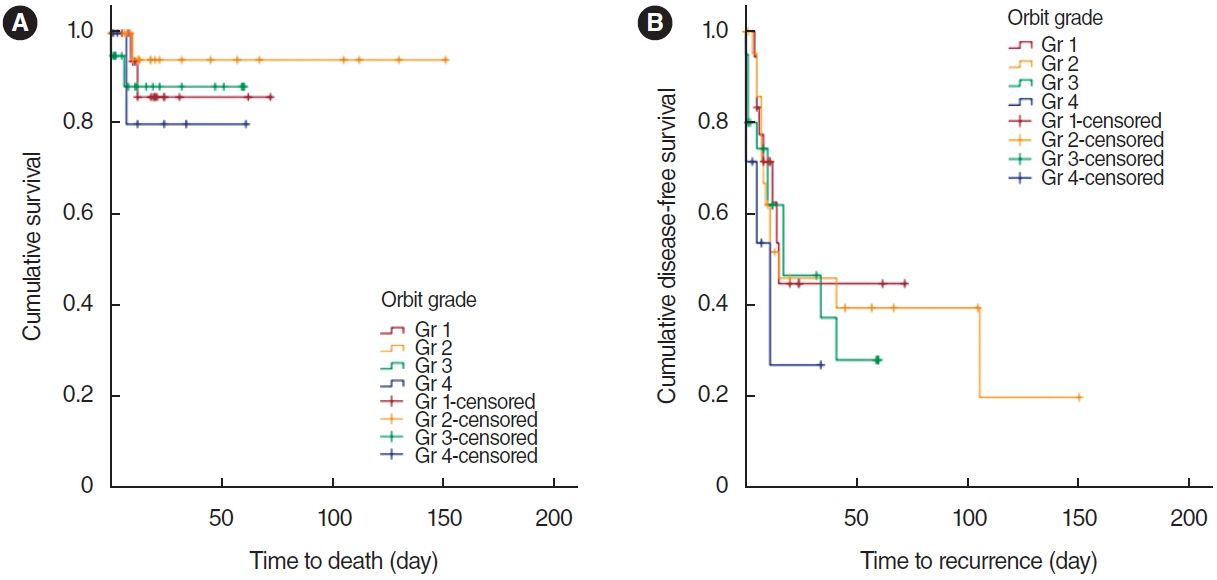
Results
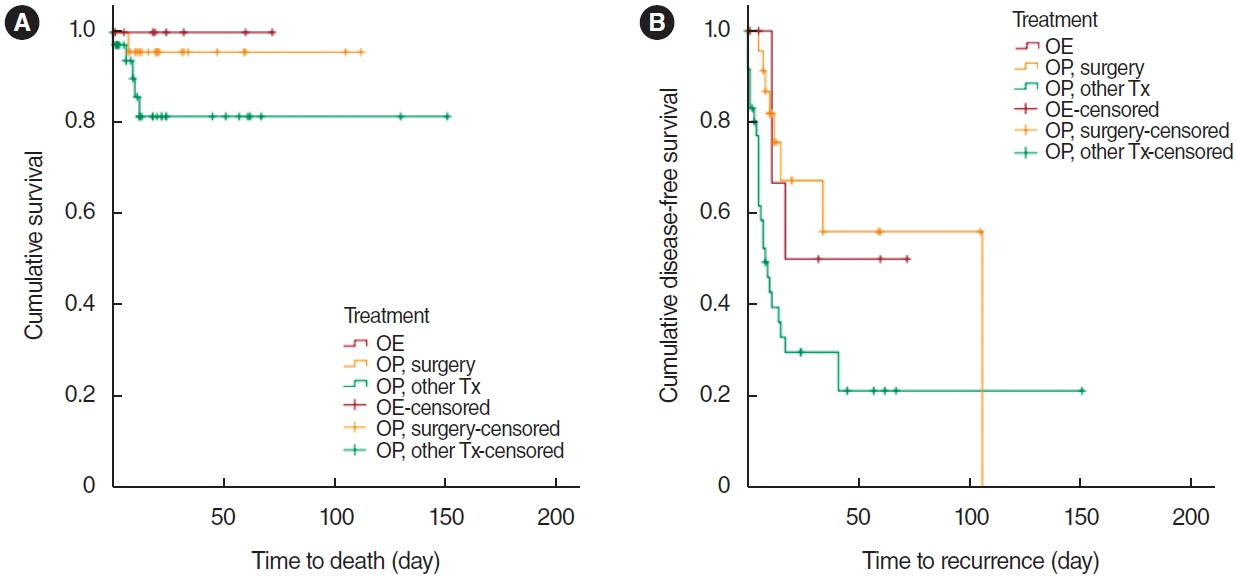
. Overall survival and disease-free survival (DFS) rates showed no significant differences based on the grade of orbital invasion. When tumor resection with orbit preservation was employed as the definitive treatment, DFS was significantly extended compared to cases where surgery was not the definitive treatment (RT or CCRT). Additionally, there was no significant difference in DFS between patients who underwent orbit exenteration and those who underwent tumor resection with orbit preservation as the definitive treatment.
Conclusion
. Tumor resection with orbit preservation as the definitive treatment appears to be the preferred approach, prolonging DFS and increasing the likelihood of longer-term survival in cases of SqCC with orbital invasion.
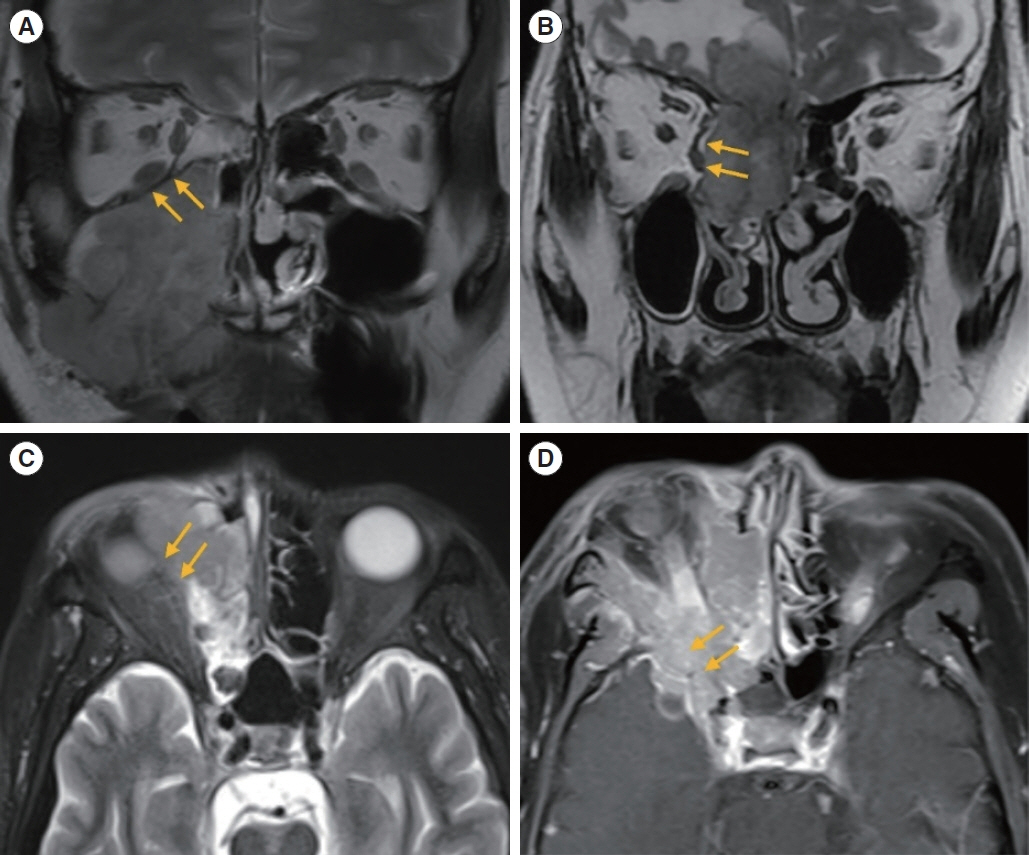
Figure
Reference
-
1. Maghami E, Kraus DH. Cancer of the nasal cavity and paranasal sinuses. Expert Rev Anticancer Ther. 2004; Jun. 4(3):411–24.2. Turri-Zanoni M, Battaglia P, Lambertoni A, Giovannardi M, Schreiber A, Volpi L, et al. Treatment strategies for primary early-stage sinonasal adenocarcinoma: a retrospective bi-institutional case-control study. J Surg Oncol. 2015; Oct. 112(5):561–7.3. Dulguerov P, Jacobsen MS, Allal AS, Lehmann W, Calcaterra T. Nasal and paranasal sinus carcinoma: are we making progress?: a series of 220 patients and a systematic review. Cancer. 2001; Dec. 92(12):3012–29.4. Waldron J, Witterick I. Paranasal sinus cancer: caveats and controversies. World J Surg. 2003; Jul. 27(7):849–55.5. Pignon JP, le Maitre A, Maillard E, Bourhis J; MACH-NC Collaborative Group. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiother Oncol. 2009; Jul. 92(1):4–14.6. Haddad RI, Shin DM. Recent advances in head and neck cancer. N Engl J Med. 2008; Sep. 359(11):1143–54.7. Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, Morrison W, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med. 2003; Nov. 349(22):2091–8.8. Tobias JS, Monson K, Gupta N, Macdougall H, Glaholm J, Hutchison I, et al. Chemoradiotherapy for locally advanced head and neck cancer: 10-year follow-up of the UK Head and Neck (UKHAN1) trial. Lancet Oncol. 2010; Jan. 11(1):66–74.9. Kuo YH, Lin CS. Regression of advanced maxillary sinus cancer with orbital invasion by combined chemotherapy and immunotherapy: a one-year follow-up case report. Mol Clin Oncol. 2022; Apr. 16(4):94.10. Ock CY, Keam B, Kim TM, Han DH, Won TB, Lee SH, et al. Induction chemotherapy in head and neck squamous cell carcinoma of the paranasal sinus and nasal cavity: a role in organ preservation. Korean J Intern Med. 2016; May. 31(3):570–8.11. Ganly I, Patel SG, Singh B, Kraus DH, Bridger PG, Cantu G, et al. Craniofacial resection for malignant paranasal sinus tumors: report of an International Collaborative Study. Head Neck. 2005; Jul. 27(7):575–84.12. Carrillo JF, Guemes A, Ramirez-Ortega MC, Onate-Ocana LF. Prognostic factors in maxillary sinus and nasal cavity carcinoma. Eur J Surg Oncol. 2005; Dec. 31(10):1206–12.13. Suarez C, Llorente JL, Fernandez De Leon R, Maseda E, Lopez A. Prognostic factors in sinonasal tumors involving the anterior skull base. Head Neck. 2004; Feb. 26(2):136–44.14. Lisan Q, Kolb F, Temam S, Tao Y, Janot F, Moya-Plana A. Management of orbital invasion in sinonasal malignancies. Head Neck. 2016; Nov. 38(11):1650–6.15. Imola MJ, Schramm VL Jr. Orbital preservation in surgical management of sinonasal malignancy. Laryngoscope. 2002; Aug. 112(8 Pt 1):1357–65.16. Howard DJ, Lund VJ, Wei WI. Craniofacial resection for tumors of the nasal cavity and paranasal sinuses: a 25-year experience. Head Neck. 2006; Oct. 28(10):867–73.17. Shin CH, Lee HJ, Chung YS, Kim JH. Treatment outcomes of sinonasal malignancies involving the orbit. J Neurol Surg B Skull Base. 2021; May. 83(Suppl 2):e430–7.18. Iannetti G, Valentini V, Rinna C, Ventucci E, Marianetti TM. Ethmoido-orbital tumors: our experience. J Craniofac Surg. 2005; Nov. 16(6):1085–91.19. Wu X, Tang P, Qi Y. Management of the orbital contents in radical surgery for squamous cell carcinoma of the maxillary sinus. Chin Med J (Engl). 1995; Feb. 108(2):123–5.20. Carrau RL, Segas J, Nuss DW, Snyderman CH, Janecka IP, Myers EN, et al. Squamous cell carcinoma of the sinonasal tract invading the orbit. Laryngoscope. 1999; Feb. 109(2 Pt 1):230–5.21. Lund VJ, Howard DJ, Wei WI, Cheesman AD. Craniofacial resection for tumors of the nasal cavity and paranasal sinuses: a 17-year experience. Head Neck. 1998; Mar. 20(2):97–105.22. Reyes C, Mason E, Solares CA, Bush C, Carrau R. To preserve or not to preserve the orbit in paranasal sinus neoplasms: a meta-analysis. J Neurol Surg B Skull Base. 2015; Mar. 76(2):122–8.23. Wang EW, Zanation AM, Gardner PA, Schwartz TH, Eloy JA, Adappa ND, et al. ICAR: endoscopic skull-base surgery. Int Forum Allergy Rhinol. 2019; Jul. 9(S3):S145–365.24. Turri-Zanoni M, Lambertoni A, Margherini S, Giovannardi M, Ferrari M, Rampinelli V, et al. Multidisciplinary treatment algorithm for the management of sinonasal cancers with orbital invasion: a retrospective study. Head Neck. 2019; Aug. 41(8):2777–88.25. Salfrant M, Garcia GC, Guichard JP, Bidault F, Reizine D, Auperin A, et al. Imaging of skull base and orbital invasion in sinonasal cancer: correlation with histopathology. Cancers (Basel). 2021; Oct. 13(19):4963.26. Safi AF, Behn L, Rothamel D, Guntinas-Lichius O, Beutner D, Nickenig HJ, et al. Therapy of sinonasal malignancies invading the orbitorbital exenteration versus preservation of the orbit plus radiotherapy. J Craniomaxillofac Surg. 2017; Feb. 45(2):258–61.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hybrid verrucous squamous cell carcinoma of sinonasal tract: a case report
- Surgical Management of Sinonasal Cancer
- Squamous Cell Carcinoma Involving Lacrimal Apparatus
- Expression of p53, p21, Cycin D1, and Ki-67 in Sinonasal Tumors
- Clinical Characteristics of the Adenoid Cystic Carcinoma of the Sinonasal Tracts