Clin Exp Otorhinolaryngol.
2024 Aug;17(3):217-225. 10.21053/ceo.2024.00034.
Positional Obstructive Sleep Apnea and Periodic Limb Movements During Sleep: A Large Multicenter Study
- Affiliations
-
- 1Seoul National University College of Medicine, Seoul, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Cheonan, Korea
- 3OUaR LaB Inc., Seoul, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Pharmacology, Seoul National University College of Medicine, Seoul, Korea
- 6Department of Biomedical Sciences, Seoul National University College of Medicine, Seoul, Korea
- 7Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 8Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul, Korea
- 9Sensory Organ Research Institute, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2558838
- DOI: http://doi.org/10.21053/ceo.2024.00034
Abstract
Objectives
. The relationships among positional obstructive sleep apnea (POSA), obstructive sleep apnea (OSA), and periodic limb movements during sleep (PLMS) remain unclear. We investigated these relationships with respect to the severity of OSA and explored the underlying mechanisms.
Methods
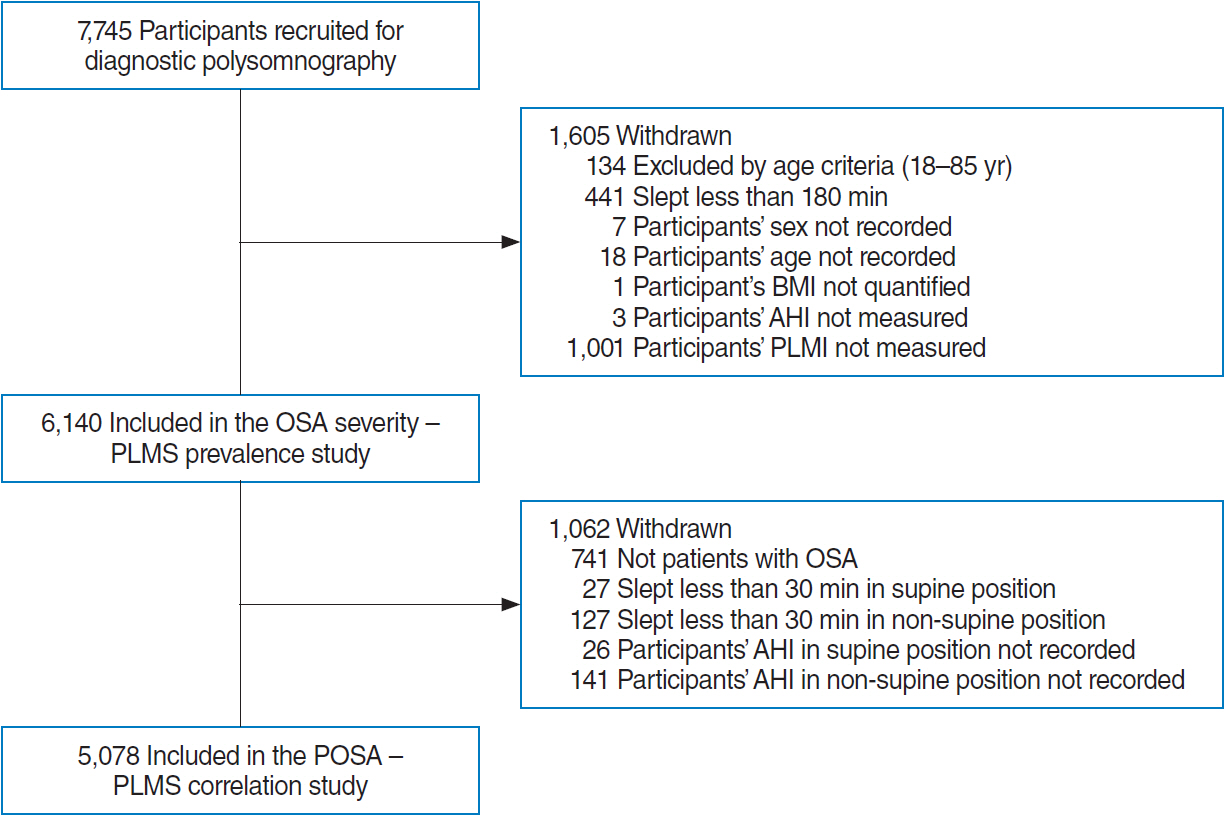
. We retrospectively reviewed 6,140 eligible participants who underwent full-night diagnostic polysomnography at four clinical centers over a 5-year period, utilizing event-synchronized analysis. We evaluated the periodic limb movement index (PLMI) and the periodic limb movement with arousal index (PLMAI). The impacts of POSA on the PLMI, PLMAI, and PLMS were analyzed in relation to the severity of OSA.
Results
. The mean PLMI, the mean PLMAI, and the prevalence of PLMS were significantly lower in participants with severe OSA compared to the mild and moderate OSA groups. The mean PLMI among those with mild OSA exceeded that of control participants. Furthermore, the mean PLMI (4.8±12.7 vs. 2.6±9.8 events/hr, P<0.001), the mean PLMAI (0.9±3.7 vs. 0.5±3.3 events/hr, P<0.001), and the prevalence of PLMS (11% vs. 5.3%, P<0.001) were higher in patients with POSA than in those with non-positional OSA. This PLMS finding was particularly pronounced among those with severe OSA (odds ratio [OR], 1.554; 95% confidence interval [CI], 1.065–2.267) and was less evident in the mild (OR, 0.559; 95% CI, 0.303–1.030) and moderate (OR, 1.822; 95% CI, 0.995–3.339) groups.
Conclusion
. Patients with POSA, especially those with severe OSA, exhibit a comparatively high prevalence of PLMS. In cases involving prominent PLMS, the diagnosis and treatment of POSA and OSA should be considered.
Keyword
Figure
Reference
-
1. Aurora RN, Kristo DA, Bista SR, Rowley JA, Zak RS, Casey KR, et al. The treatment of restless legs syndrome and periodic limb movement disorder in adults: an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses. An American Academy of Sleep Medicine Clinical Practice Guideline. Sleep. 2012; Aug. 35(8):1039–62.2. Ferri R, Rundo F, Zucconi M, Manconi M, Bruni O, Ferini-Strambi L, et al. An evidence-based analysis of the association between periodic leg movements during sleep and arousals in restless legs syndrome. Sleep. 2015; Jun. 38(6):919–24.3. Gingras JL, Gaultney JF, Picchietti DL. Pediatric periodic limb movement disorder: sleep symptom and polysomnographic correlates compared to obstructive sleep apnea. J Clin Sleep Med. 2011; Dec. 7(6):603–9A.4. Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lesperance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov Disord. 1997; Jan. 12(1):61–5.5. Fantini ML, Michaud M, Gosselin N, Lavigne G, Montplaisir J. Periodic leg movements in REM sleep behavior disorder and related autonomic and EEG activation. Neurology. 2002; Dec. 59(12):1889–94.6. Budhiraja R, Javaheri S, Pavlova MK, Epstein LJ, Omobomi O, Quan SF. Prevalence and correlates of periodic limb movements in OSA and the effect of CPAP therapy. Neurology. 2020; Apr. 94(17):e1820–7.7. Rye DB, Trotti LM. Restless legs syndrome and periodic leg movements of sleep. Neurol Clin. 2012; Nov. 30(4):1137–66.8. Drakatos P, Olaithe M, Verma D, Ilic K, Cash D, Fatima Y, et al. Periodic limb movements during sleep: a narrative review. J Thorac Dis. 2021; Nov. 13(11):6476–94.9. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014; Nov. 146(5):1387–94.10. Joseph V, Nagalli S. Periodic limb movement disorder [Internet]. StatPearls Publishing; 2023 [cited 2024 May 20]. Available from: https://pubmed.ncbi.nlm.nih.gov/32809562/.11. Hornyak M, Feige B, Riemann D, Voderholzer U. Periodic leg movements in sleep and periodic limb movement disorder: prevalence, clinical significance and treatment. Sleep Med Rev. 2006; Jun. 10(3):169–77.12. Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002; Jul. 53(1):547–54.13. Figorilli M, Puligheddu M, Congiu P, Ferri R. The clinical importance of periodic leg movements in sleep. Curr Treat Options Neurol. 2017; Mar. 19(3):10.14. Tiseo C, Vacca A, Felbush A, Filimonova T, Gai A, Glazyrina T, et al. Migraine and sleep disorders: a systematic review. J Headache Pain. 2020; Oct. 21(1):126.15. Laratta CR, Ayas NT, Povitz M, Pendharkar SR. Diagnosis and treatment of obstructive sleep apnea in adults. CMAJ. 2017; Dec. 189(48):E1481–8.16. Huang W, Zhang X, Wang X, Zhou T, Zhao X, Xu H, et al. Effects of obstructive sleep apnea during rapid eye movement sleep on cardiac autonomic dysfunction: results from the Shanghai sleep health study cohort. J Sleep Res. 2023; Oct. 32(5):e13904.17. Malhotra A, Ayappa I, Ayas N, Collop N, Kirsch D, Mcardle N, et al. Metrics of sleep apnea severity: beyond the apnea-hypopnea index. Sleep. 2021; Jul. 44(7):zsab030.18. Wang Q, Li Y, Li J, Wang J, Shen J, Wu H, et al. Low arousal threshold: a potential bridge between OSA and periodic limb movements of sleep. Nat Sci Sleep. 2021; Feb. 13:229–38.19. Warnes H, Dinner DS, Kotagal P, Burgess RC. Periodic limb movements and sleep apnoea. J Sleep Res. 1993; Mar. 2(1):38–44.20. Lee SA, Kim SJ, Lee SY, Kim HJ. Periodic limb movements during sleep are associated with poor health-related quality of life in patients with obstructive sleep apnea. Sleep Breath. 2022; Sep. 26(3):1045–52.21. Joosten SA, O’Driscoll DM, Berger PJ, Hamilton GS. Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev. 2014; Feb. 18(1):7–17.22. Sabil A, Blanchard M, Trzepizur W, Goupil F, Meslier N, Paris A, et al. Positional obstructive sleep apnea within a large multicenter French cohort: prevalence, characteristics, and treatment outcomes. J Clin Sleep Med. 2020; Dec. 16(12):2037–46.23. Lee CH, Shin HW, Han DH, Mo JH, Yoon IY, Chung S, et al. The implication of sleep position in the evaluation of surgical outcomes in obstructive sleep apnea. Otolaryngol Head Neck Surg. 2009; Apr. 140(4):531–5.24. Skarpsno ES, Mork PJ, Nilsen TI, Holtermann A. Sleep positions and nocturnal body movements based on free-living accelerometer recordings: association with demographics, lifestyle, and insomnia symptoms. Nat Sci Sleep. 2017; Nov. 9:267–75.25. Bara-Jimenez W, Aksu M, Graham B, Sato S, Hallett M. Periodic limb movements in sleep: state-dependent excitability of the spinal flexor reflex. Neurology. 2000; Apr. 54(8):1609–16.26. Megia-Garcia A, Serrano-Munoz D, Comino-Suarez N, Del-Ama AJ, Moreno JC, Gil-Agudo A, et al. Effect of posture and body weight loading on spinal posterior root reflex responses. Eur J Neurosci. 2021; Oct. 54(7):6575–86.27. Berry RB, Gamaldo CE, Harding SM, Brooks R, Lloyd RM, Vaughn BV, et al. AASM scoring manual version 2.2 updates: new chapters for scoring infant sleep staging and home sleep apnea testing. J Clin Sleep Med. 2015; Nov. 11(11):1253–4.28. Szentkiralyi A, Stefani A, Hackner H, Czira M, Teismann IK, Volzke H, et al. Prevalence and associated risk factors of periodic limb movement in sleep in two German population-based studies. Sleep. 2019; Mar. 42(3):zsy237.29. Haba-Rubio J, Marti-Soler H, Marques-Vidal P, Tobback N, Andries D, Preisig M, et al. Prevalence and determinants of periodic limb movements in the general population. Ann Neurol. 2016; Mar. 79(3):464–74.30. Berry RB, Brooks R, Gamaldo C, Harding SM, Lloyd RM, Quan SF, et al. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. American Academy of Sleep Medicine. 2012.31. Oulhaj A, Al Dhaheri S, Su BB, Al-Houqani M. Discriminating between positional and non-positional obstructive sleep apnea using some clinical characteristics. Sleep Breath. 2017; Dec. 21(4):877–84.32. Shingala MC, Rajyaguru A. Comparison of post hoc tests for unequal variance. Int J New Techn Sci Eng. 2015; Nov. 2(5):22–33.33. Leary EB, Moore HE, Schneider LD, Finn LA, Peppard PE, Mignot E. Periodic limb movements in sleep: prevalence and associated sleepiness in the Wisconsin Sleep Cohort. Clin Neurophysiol. 2018; Nov. 129(11):2306–14.34. Claman DM, Ewing SK, Redline S, Ancoli-Israel S, Cauley JA, Stone KL, et al. Periodic leg movements are associated with reduced sleep quality in older men: the MrOS Sleep Study. J Clin Sleep Med. 2013; Nov. 9(11):1109–17.35. Marcus CL, Traylor J, Gallagher PR, Brooks LJ, Huang J, Koren D, et al. Prevalence of periodic limb movements during sleep in normal children. Sleep. 2014; Aug. 37(8):1349–52.36. Scofield H, Roth T, Drake C. Periodic limb movements during sleep: population prevalence, clinical correlates, and racial differences. Sleep. 2008; Sep. 31(9):1221–7.37. Kang S, Yoon I. The prevalence and impact on sleep of periodic limb movements during sleep in the elderly. Sleep Med. 2013; Dec. 14(Suppl 1):e165–6.38. Huang W, Wang X, Xu C, Xu H, Zhu H, Liu S, et al. Prevalence, characteristics, and respiratory arousal threshold of positional obstructive sleep apnea in China: a large scale study from Shanghai Sleep Health Study cohort. Respir Res. 2022; Sep. 23(1):240.39. Chada A, Hoque R. Images: periodic limb movements during sleep noted on ventral thigh surface electromyography in an above-theknee amputated stump. J Clin Sleep Med. 2019; Aug. 15(8):1183–4.40. Danner SM, Krenn M, Hofstoetter US, Toth A, Mayr W, Minassian K. Body position influences which neural structures are recruited by lumbar transcutaneous spinal cord stimulation. PLoS One. 2016; 11(1):e0147479.41. Klarner T, Zehr EP. Sherlock Holmes and the curious case of the human locomotor central pattern generator. J Neurophysiol. 2018; Jul. 120(1):53–77.42. Calancie B, Needham-Shropshire B, Jacobs P, Willer K, Zych G, Green BA. Involuntary stepping after chronic spinal cord injury: evidence for a central rhythm generator for locomotion in man. Brain. 1994; Oct. 117(Pt 5):1143–59.43. Guertin PA. Central pattern generator for locomotion: anatomical, physiological, and pathophysiological considerations. Front Neurol. 2013; Feb. 3:183.44. Kakkar RK, Berry RB. Positive airway pressure treatment for obstructive sleep apnea. Chest. 2007; Sep. 132(3):1057–72.45. Stuck BA, Leitzbach S, Maurer JT. Effects of continuous positive airway pressure on apnea-hypopnea index in obstructive sleep apnea based on long-term compliance. Sleep Breath. 2012; Jun. 16(2):467–71.46. Jonas DE, Amick HR, Feltner C, Weber RP, Arvanitis M, Stine A, et al. Screening for obstructive sleep apnea in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017; Jan. 317(4):415–33.47. Baran AS, Richert AC, Douglass AB, May W, Ansarin K. Change in periodic limb movement index during treatment of obstructive sleep apnea with continuous positive airway pressure. Sleep. 2003; Sep. 26(6):717–20.48. Lin TC, Zeng BY, Wu MN, Chen TY, Chen YW, Yeh PY, et al. Changes in periodic limb movements of sleep after the use of continuous positive airway pressure therapy: a meta-analysis. Front Neurol. 2022; Jun. 13:817009.49. Hedli LC, Christos P, Krieger AC. Unmasking of periodic limb movements with the resolution of obstructive sleep apnea during continuous positive airway pressure application. J Clin Neurophysiol. 2012; Aug. 29(4):339–44.50. Lee SA, Kim SJ, Lee SY, Kim HJ. Clinical characteristics of periodic limb movements during sleep categorized by continuous positive airway pressure titration polysomnography in patients with obstructive sleep apnea. Sleep Breath. 2022; Mar. 26(1):251–7.51. Sforza E, Haba-Rubio J. Night-to-night variability in periodic leg movements in patients with restless legs syndrome. Sleep Med. 2005; May. 6(3):259–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Significance of Periodic Limb Movements During Sleep in Various Sleep Disorders
- The Clinical Characteristics Between the Positional Obstructive Sleep Apnea Patients with the Non-positional Obstructive Sleep Apnea Patients
- The Effects of Obstructive Sleep Apnea Syndrome on Periodic Limb Movements in Sleep
- Sex Differences in Excessive Daytime Sleepiness Among Patients With Obstructive Sleep Apnea
- A Review on Sleep Disorders Similar to REM Sleep Behavior Disorder