J Korean Neurosurg Soc.
2024 Sep;67(5):578-585. 10.3340/jkns.2023.0026.
Surgical Thrombectomy for Extensive Cerebral Venous Sinus Thrombosis after COVID-19 Vaccination : A Novel Surgical Technique and Literature Review
- Affiliations
-
- 1Department of Medicine, Graduate School, Kyung Hee University, Seoul, Korea
- 2Department of Neurosurgery, Kyung Hee University Hospital, Seoul, Korea
- KMID: 2558683
- DOI: http://doi.org/10.3340/jkns.2023.0026
Abstract
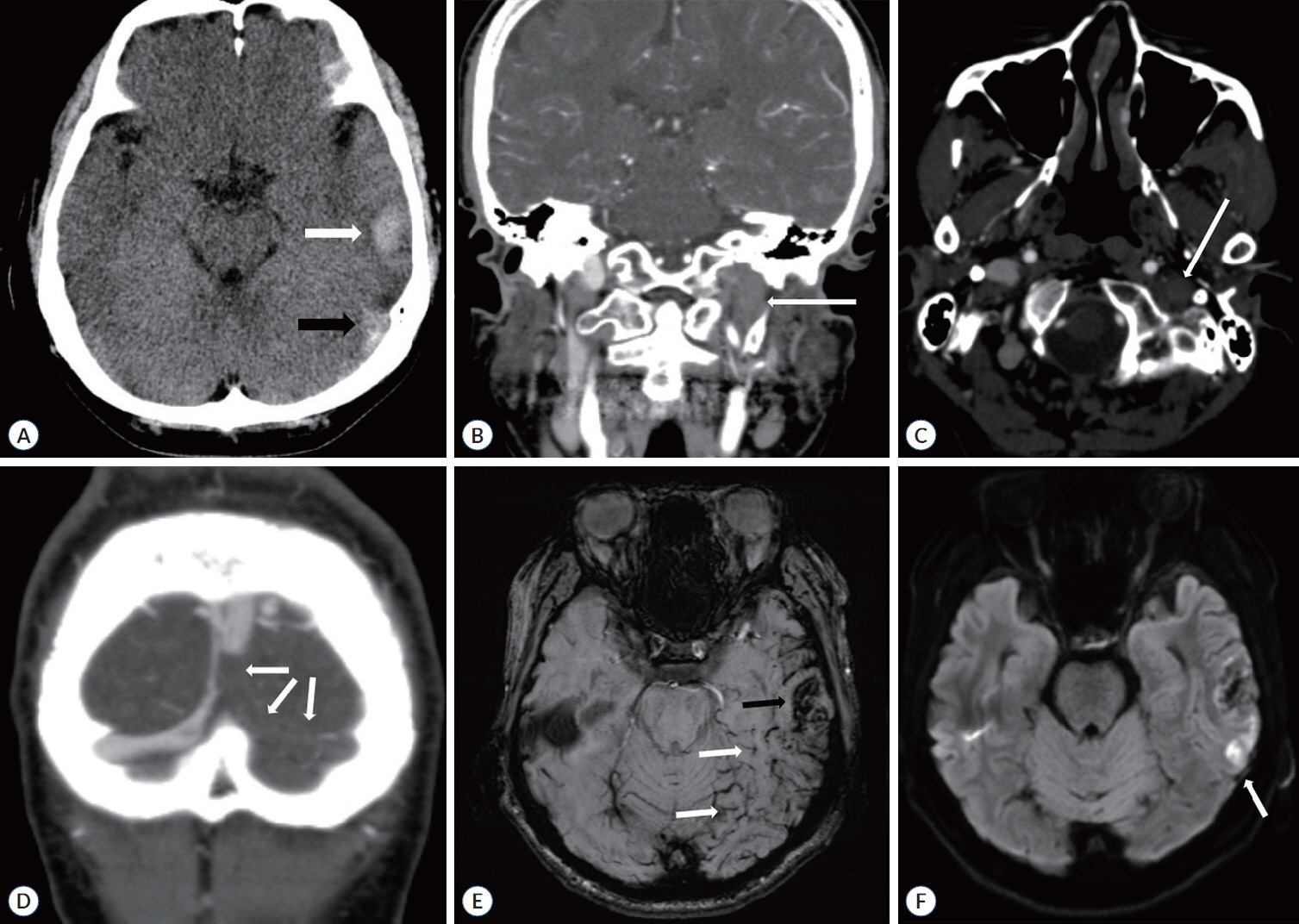
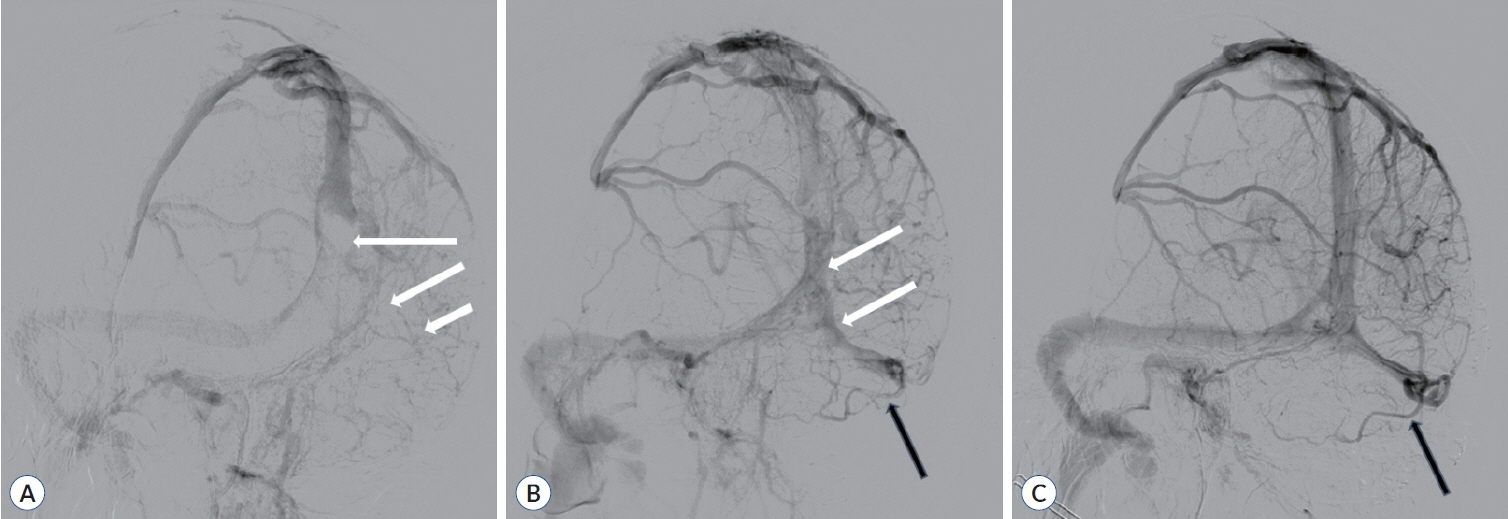
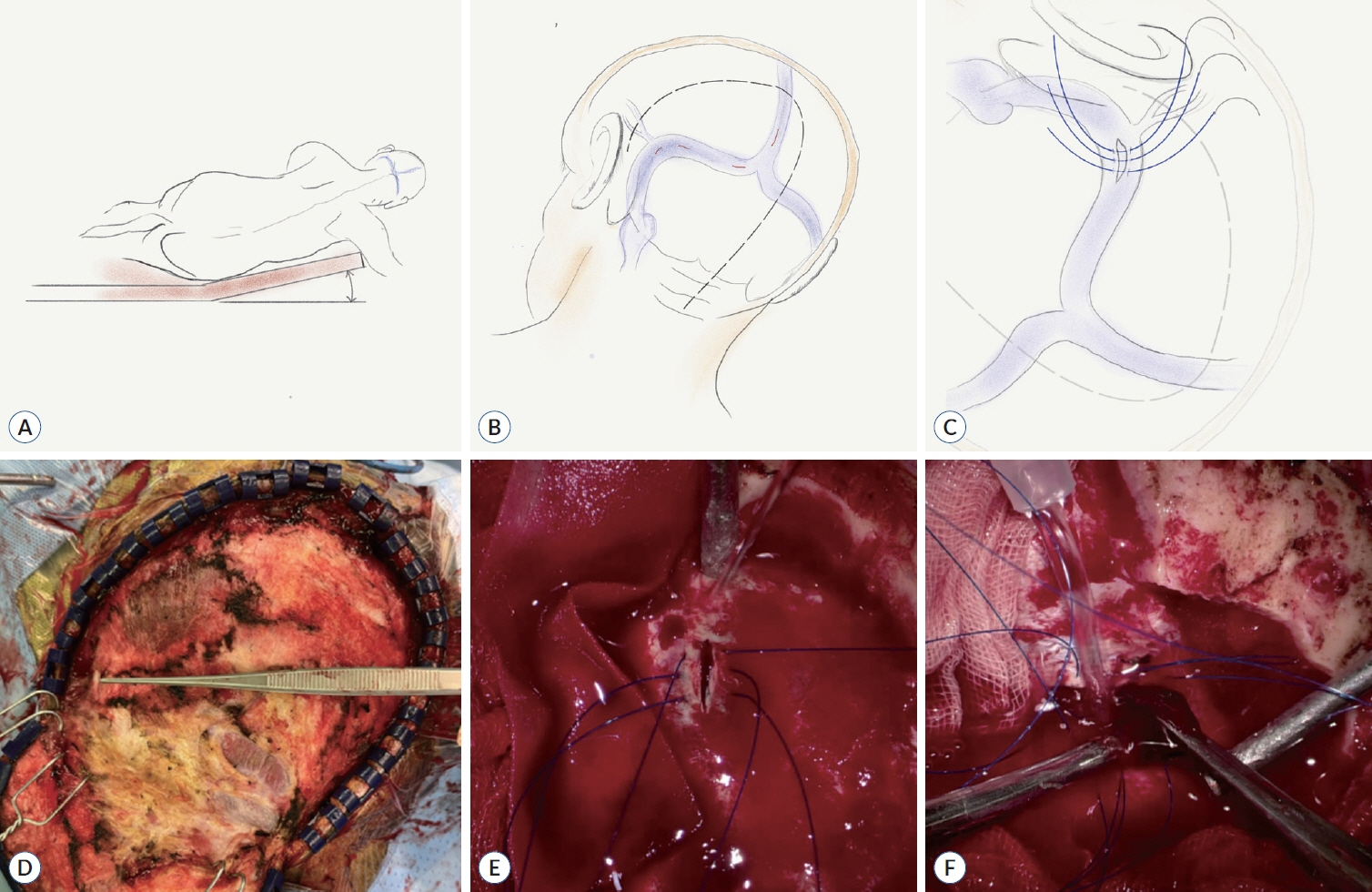
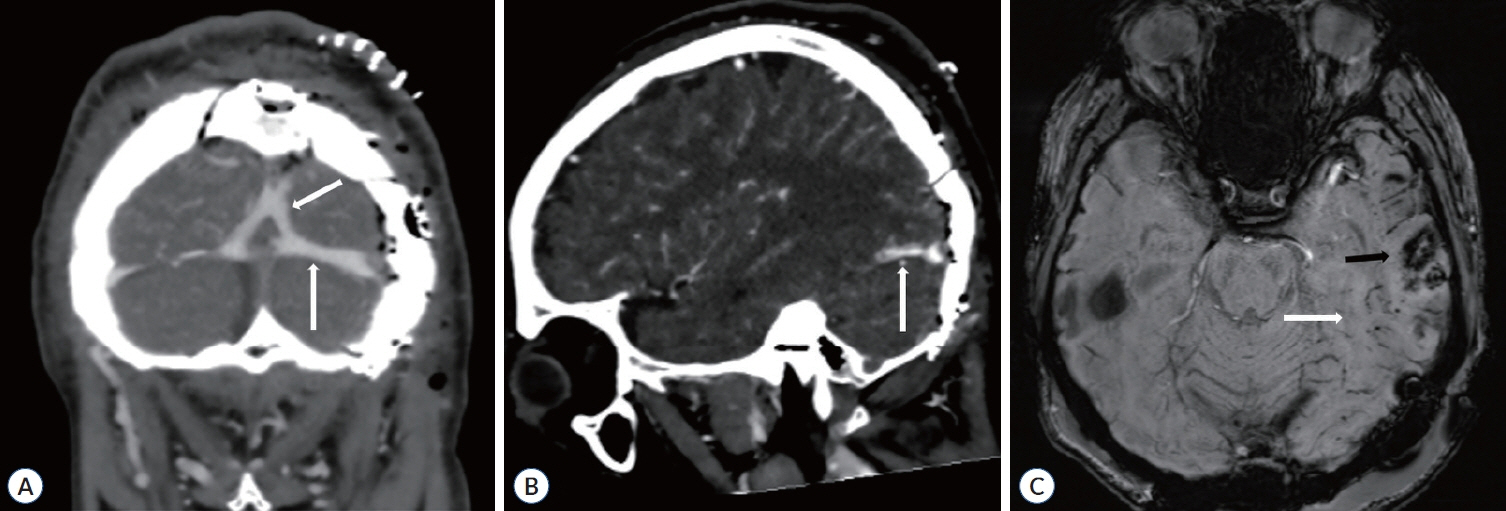
- Surgical treatment of refractory and extensive cerebral venous sinus thrombosis (CVST) has limited applications. Here, we describe an open, direct sinus thrombectomy in the early phase of extensive CVST. A 49-year-old man with extensive CVST that occurred after the coronavirus disease 2019 (COVID-19) vaccination and affected the drainage of the Labbé vein presented with clinical deterioration and left temporal hemorrhagic infarction. Since the patient had extensive CVST, we determined that systemic anticoagulation and endovascular treatment were not suitable treatment options. Therefore, we decided on an emergency surgical treatment and performed direct surgical thrombectomy. We followed extended suboccipital approach and made multiple incisions on the sinuses, exposing the posterior superior sagittal sinus to the transverse sigmoid junction. Consequently, the clinical condition of the patient dramatically improved, resulting in a favorable outcome with a modified Rankin scale score of 0. Performing emergency open surgical thrombectomy was a technically feasible treatment option that recanalize obstructed sinuses. Importantly, the patient recovered with a good clinical outcome. Early maximal surgical thrombectomy can be an effective and lifesaving method to treat extensive CVST with hemorrhagic infarction.
Keyword
Figure
Reference
-
References
1. Azin H, Ashjazadeh N. Cerebral venous sinus thrombosis--clinical features, predisposing and prognostic factors. Acta Neurol Taiwan. 17:82–87. 2008.2. Boncoraglio G, Carriero MR, Chiapparini L, Ciceri E, Ciusani E, Erbetta A, et al. Hyperhomocysteinemia and other thrombophilic risk factors in 26 patients with cerebral venous thrombosis. Eur J Neurol. 11:405–409. 2004.3. Boukobza M, Crassard I, Bousser MG, Chabriat H. Labbé vein thrombosis. Neuroradiology. 62:935–945. 2020.
Article4. Ekseth K, Boström S, Vegfors M. Reversibility of severe sagittal sinus thrombosis with open surgical thrombectomy combined with local infusion of tissue plasminogen activator: technical case report. Neurosurgery. 43:960–965. 1998.
Article5. Ferro JM, Bousser MG, Canhão P, Coutinho JM, Crassard I, Dentali F, et al. European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis - endorsed by the European Academy of Neurology. Eur J Neurol. 2:1203–1213. 2017.
Article6. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F; ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 35:664–670. 2004.
Article7. Furie KL, Cushman M, Elkind MSV, Lyden PD, Saposnik G; American Heart Association/American Stroke Association Stroke Council Leadership. Diagnosis and management of cerebral venous sinus thrombosis with vaccine-induced immune thrombotic thrombocytopenia. Stroke. 52:2478–2482. 2021.
Article8. Gazioglu S, Eyuboglu I, Yildirim A, Aydin CO, Alioglu Z. Cerebral venous sinus thrombosis: clinical features, long-term outcome and recanalization. J Clin Neurosci. 45:248–251. 2017.
Article9. Guenther G, Arauz A. Cerebral venous thrombosis: a diagnostic and treatment update. Neurologia. 26:488–498. 2011.
Article10. Khealani BA, Wasay M, Saadah M, Sultana E, Mustafa S, Khan FS, et al. Cerebral venous thrombosis: a descriptive multicenter study of patients in Pakistan and Middle East. Stroke. 39:2707–2711. 2008.11. Kourtopoulos H, Christie M, Rath B. Open thrombectomy combined with thrombolysis in massive intracranial sinus thrombosis. Acta Neurochir (Wien). 128:171–173. 1994.
Article12. Lechanoine F, Janot K, Herbreteau D, Maldonado IL, Velut S. Surgical thrombectomy combined with bilateral decompressive craniectomy in a life-threatening case of coma from cerebral venous sinus thrombosis: case report and literature review. World Neurosurg. 120:485–489. 2018.
Article13. Lee DJ, Ahmadpour A, Binyamin T, Dahlin BC, Shahlaie K, Waldau B. Management and outcome of spontaneous cerebral venous sinus thrombosis in a 5-year consecutive single-institution cohort. J Neurointerv Surg. 9:34–38. 2017.
Article14. Lee DJ, Latchaw RE, Dahlin BC, Dong PR, Verro P, Muizelaar JP, et al. Antegrade rheolytic thrombectomy and thrombolysis for superior sagittal sinus thrombosis using burr hole access. BMJ Case Rep. 2014; bcr2013011087. 2014.
Article15. Persson L, Lilja A. Extensive dural sinus thrombosis treated by surgical removal and local streptokinase infusion. Neurosurgery. 26:117–121. 1990.
Article16. Pongmoragot J, Saposnik G. Intracerebral hemorrhage from cerebral venous thrombosis. Curr Atheroscler Rep. 14:382–389. 2012.
Article17. Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 42:1158–1192. 2011.
Article18. See I, Su JR, Lale A, Woo EJ, Guh AY, Shimabukuro TT, et al. US case reports of cerebral venous sinus thrombosis with thrombocytopenia after Ad26.COV2.S vaccination, March 2 to April 21, 2021. JAMA. 325:2448–2456. 2021.
Article19. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 352:1791–1798. 2005.
Article20. Taquet M, Husain M, Geddes JR, Luciano S, Harrison PJ. Cerebral venous thrombosis: a retrospective cohort study of 513,284 confirmed COVID-19 cases and a comparison with 489,871 people receiving a COVID-19 mRNA vaccine. medRxiv. 2021; [Epub ahead of print].
Article21. Westwick HJ, Obaid S, Bordeleau-Roy F, Truffer E, Weil AG. Surgical superior sagittal sinus thrombectomy in refractory thrombosis: a technical note. Pediatr Neurosurg. 54:212–217. 2019.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracerebral Hemorrhage due to Thrombosis with Thrombocytopenia Syndrome after Vaccination against COVID-19: the First Fatal Case in Korea
- Treatment of the Superior Sagittal Sinus Thrombosis with the Mechanical Thrombectomy Using Stent-Retriever Device
- Cerebral Venous Thrombosis without Thrombocytopenia after COVID-19 Vaccination
- Cerebral Venous Sinus Thrombosis After Pfizer-BioNTech COVID-19 (BNT162b2) Vaccination
- Fatal Case of Acute Pulmonary Embolism due to Venous Thrombosis after COVID-19 Vaccination: Based on Forensic Postmortem Examination