J Korean Neurosurg Soc.
2024 Sep;67(5):560-567. 10.3340/jkns.2023.0214.
Two-Day Fraction Gamma Knife Radiosurgery for Large Brain Metastasis
- Affiliations
-
- 1Brain Tumor Clinic & Gamma Knife Center, Department of Neurosurgery, Chonnam National University Hwasun Hospital, Hwasun, Korea
- KMID: 2558681
- DOI: http://doi.org/10.3340/jkns.2023.0214
Abstract
Objective
: We investigated how treating large brain metastasis (LBM) using 2-day fraction Gamma Knife radiosurgery (GKRS) affects tumor control and patient survival. A prescription dose of 10.3 Gy was applied for 2 consecutive days, with a biologically effective dose equivalent to a tumor single-fraction dose of 16.05 Gy and a brain single-fraction dose of 15.12 Gy.
Methods
: Between November 2017 and December 2021, 42 patients (mean age, 68.3 years; range, 50–84 years; male, 29 [69.1%]; female, 13 [30.9%]) with 44 tumors underwent 2-day fraction GKRS to treat large volume brain metastasis. The main cancer types were non-small cell lung cancer (n=16), small cell lung cancer (n=7), colorectal cancer (n=7), breast cancer (n=3), gastric cancer (n=2), and other cancers (n=7). Twenty-one patients (50.0%) had a single LBM, 19 (46.3%) had a single LBM and other metastases, and two had two (4.7%) large brain metastases. At the time of the 2-day fraction GKRS, the tumors had a mean volume of 23.1 mL (range, 12.5–67.4). On each day, radiation was administered at a dose of 10.3 Gy, mainly using a 50% isodose-line.
Results
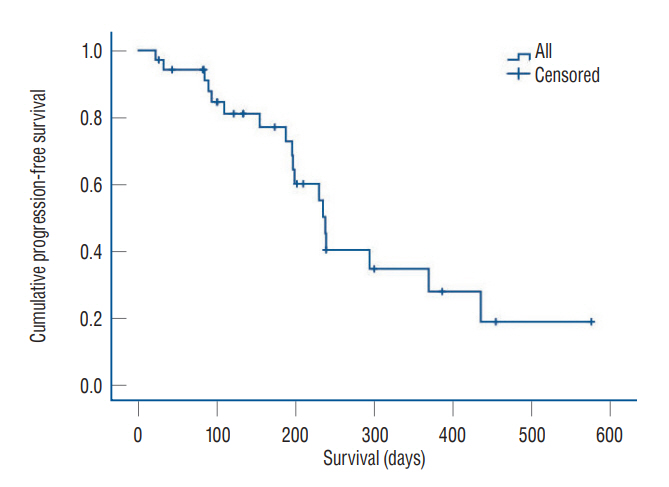
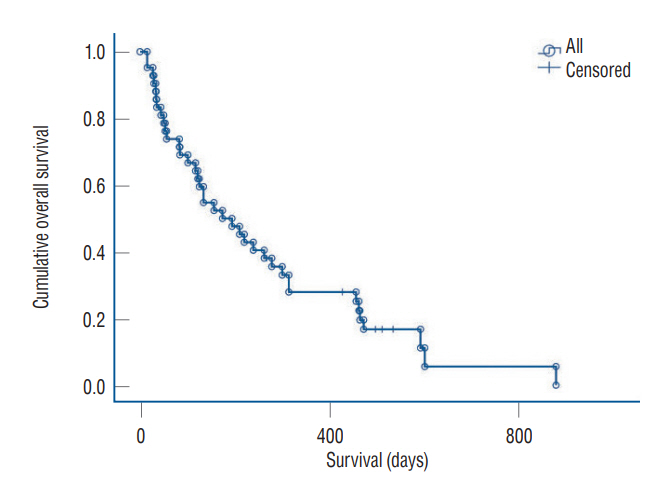
: We obtained clinical and magnetic resonance imaging follow-up data for 34 patients (81%) with 35 tumors, who had undergone 2-day fraction GKRS. These patients did not experience acute or late radiation-induced complications during follow-up. The median and mean progression-free survival (PFS) periods were 188 and 194 days, respectively. The local control rates at 6, 9, and 12 months were 77%, 40%, and 34%, respectively. The prognostic factors related to PFS were prior radiotherapy (p=0.019) and lung cancer origin (p=0.041). Other factors such as tumor volumes, each isodose volumes, and peri-GKRS systemic treatment were not significantly related to PFS. The overall survival period of the 44 patients following repeat stereotactic radiosurgery (SRS) ranged from 15–878 days (median, 263±38 days; mean, 174±43 days) after the 2-day fraction GKRS. Eight patients (18.2%) were still alive.
Conclusion
: Considering the unsatisfactory tumor control, a higher prescription dose should be needed in this procedure as a salvage management. Moreover, in the treatment for LBM with fractionated SRS, using different isodoses and prescription doses at the treatment planning for LBMs should be important. However, this report might be a basic reference with the same fraction number and prescription dose in the treatment for LBMs with frame-based SRS.
Keyword
Figure
Reference
-
References
1. Angelov L, Mohammadi AM, Bennett EE, Abbassy M, Elson P, Chao ST, et al. Impact of 2-staged stereotactic radiosurgery for treatment of brain metastases ≥ 2 cm. J Neurosurg. 129:366–382. 2018.
Article2. Arvold ND, Lee EQ, Mehta MP, Margolin K, Alexander BM, Lin NU, et al. Updates in the management of brain metastases. Neuro Oncol. 18:1043–1065. 2016.
Article3. Barendsen GW. Dose fractionation, dose rate and iso-effect relationships for normal tissue responses. Int J Radiat Oncol Biol Phys. 8:1981–1997. 1982.
Article4. Cui T, Weiner J, Danish S, Chundury A, Ohri N, Yue N, et al. Evaluation of biological effective dose in gamma knife staged stereotactic radiosurgery for large brain metastases. Front Oncol. 12:892139. 2022.
Article5. Eaton BR, LaRiviere MJ, Kim S, Prabhu RS, Patel K, Kandula S, et al. Hypofractionated radiosurgery has a better safety profile than single fraction radiosurgery for large resected brain metastases. J Neurooncol. 123:103–111. 2015.
Article6. Feuvret L, Vinchon S, Martin V, Lamproglou I, Halley A, Calugaru V, et al. Stereotactic radiotherapy for large solitary brain metastases. Cancer Radiother. 18:97–106. 2014.7. Fokas E, Henzel M, Surber G, Kleinert G, Hamm K, Engenhart-Cabillic R. Stereotactic radiosurgery and fractionated stereotactic radiotherapy: comparison of efficacy and toxicity in 260 patients with brain metastases. J Neurooncol. 109:91–98. 2012.
Article8. Fowler JF. Dose response curves for organ function or cell survival. Br J Radiol. 56:497–500. 1983.
Article9. Fowler JF. The linear-quadratic formula and progress in fractionated radiotherapy. Br J Radiol. 62:679–694. 1989.
Article10. Han JH, Kim DG, Chung HT, Paek SH, Park CK, Jung HW. Radiosurgery for large brain metastases. Int J Radiat Oncol Biol Phys. 83:113–120. 2012.
Article11. Higuchi Y, Serizawa T, Nagano O, Matsuda S, Ono J, Sato M, et al. Three-staged stereotactic radiotherapy without whole brain irradiation for large metastatic brain tumors. Int J Radiat Oncol Biol Phys. 74:1543–1548. 2009.12. Inoue HK, Sato H, Suzuki Y, Saitoh J, Noda SE, Seto K, et al. Optimal hypofractionated conformal radiotherapy for large brain metastases in patients with high risk factors: a single-institutional prospective study. Radiat Oncol. 9:231. 2014.
Article13. Jeong WJ, Park JH, Lee EJ, Kim JH, Kim CJ, Cho YH. Efficacy and safety of fractionated stereotactic radiosurgery for large brain metastases. J Korean Neurosurg Soc. 58:217–224. 2015.
Article14. Jiang XS, Xiao JP, Zhang Y, Xu YJ, Li XP, Chen XJ, et al. Hypofractionated stereotactic radiotherapy for brain metastases larger than three centimeters. Radiat Oncol. 7:36. 2012.
Article15. Kim KH, Kong DS, Cho KR, Lee MH, Choi JW, Seol HJ, et al. Outcome evaluation of patients treated with fractionated gamma knife radiosurgery for large (> 3 cm) brain metastases: a dose-escalation study. J Neurosurg. 133:675–684. 2019.
Article16. Kirkpatrick JP, Soltys SG, Lo SS, Beal K, Shrieve DC, Brown PD. The radiosurgery fractionation quandary: single fraction or hypofractionation? Neuro Oncol. 19(suppl_2):ii38–ii49. 2017.
Article17. Lee CC, Yen CP, Xu Z, Schlesinger D, Sheehan J. Large intracranial metastatic tumors treated by gamma knife surgery: outcomes and prognostic factors. J Neurosurg. 120:52–59. 2014.18. Lim TK, Kim WK, Yoo CJ, Kim EY, Kim MJ, Yee GT. Fractionated stereotactic radiosurgery for brain metastases using the Novalis Tx® system. J Korean Neurosurg Soc. 61:525–529. 2018.
Article19. Lippitz B, Lindquist C, Paddick I, Peterson D, O’Neill K, Beaney R. Stereotactic radiosurgery in the treatment of brain metastases: the current evidence. Cancer Treat Rev. 40:48–59. 2014.
Article20. Luther N, Kondziolka D, Kano H, Mousavi SH, Engh JA, Niranjan A, et al. Predicting tumor control after resection bed radiosurgery of brain metastases. Neurosurgery. 73:1001–1006. discussion 1006. 2013.
Article21. Minniti G, D’Angelillo RM, Scaringi C, Trodella LE, Clarke E, Matteucci P, et al. Fractionated stereotactic radiosurgery for patients with brain metastases. J Neurooncol. 117:295–301. 2014.
Article22. Minniti G, Scaringi C, Paolini S, Lanzetta G, Romano A, Cicone F, et al. Single-fraction versus multifraction (3 × 9 Gy) stereotactic radiosurgery for large (>2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiat Oncol Biol Phys. 95:1142–1148. 2016.23. Murai T, Ogino H, Manabe Y, Iwabuchi M, Okumura T, Matsushita Y, et al. Fractionated stereotactic radiotherapy using CyberKnife for the treatment of large brain metastases: a dose escalation study. Clin Oncol (R Coll Radiol). 26:151–158. 2014.
Article24. Narayana A, Chang J, Yenice K, Chan K, Lymberis S, Brennan C, et al. Hypofractionated stereotactic radiotherapy using intensity-modulated radiotherapy in patients with one or two brain metastases. Stereotact Funct Neurosurg. 85:82–87. 2007.
Article25. Navarria P, Pessina F, Cozzi L, Ascolese AM, De Rose F, Fogliata A, et al. Hypo-fractionated stereotactic radiotherapy alone using volumetric modulated arc therapy for patients with single, large brain metastases unsuitable for surgical resection. Radiat Oncol. 11:76. 2016.
Article26. Ogura K, Mizowaki T, Ogura M, Sakanaka K, Arakawa Y, Miyamoto S, et al. Outcomes of hypofractionated stereotactic radiotherapy for metastatic brain tumors with high risk factors. J Neurooncol. 109:425–432. 2012.
Article27. Park HR, Park KW, Lee JM, Kim JH, Jeong SS, Kim JW, et al. Frameless fractionated gamma knife radiosurgery with ICON™ for large metastatic brain tumors. J Korean Med Sci. 34:e57. 2019.28. Pessina F, Navarria P, Cozzi L, Ascolese AM, Maggi G, Rossi M, et al. Role of surgical resection in patients with single large brain metastases: feasibility, morbidity, and local control evaluation. World Neurosurg. 94:6–12. 2016.
Article29. Redmond KJ, Gui C, Benedict S, Milano MT, Grimm J, Vargo JA, et al. Tumor control probability of radiosurgery and fractionated stereotactic radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys. 110:53–67. 2021.
Article30. Serizawa T, Higuchi Y, Yamamoto M, Matsunaga S, Nagano O, Sato Y, et al. Comparison of treatment results between 3- and 2-stage gamma knife radiosurgery for large brain metastases: a retrospective multiinstitutional study. J Neurosurg. 131:227–237. 2018.
Article31. Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, et al. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys. 47:291–298. 2000.
Article32. Wegner RE, Leeman JE, Kabolizadeh P, Rwigema JC, Mintz AH, Burton SA, et al. Fractionated stereotactic radiosurgery for large brain metastases. Am J Clin Oncol. 38:135–139. 2015.33. Wiggenraad R, Verbeek-de Kanter A, Kal HB, Taphoorn M, Vissers T, Struikmans H. Dose-effect relation in stereotactic radiotherapy for brain metastases. A systematic review. Radiother Oncol. 98:292–297. 2011.
Article34. Wiggenraad R, Verbeek-de Kanter A, Mast M, Molenaar R, Kal HB, Lycklama à Nijeholt G, et al. Local progression and pseudo progression after single fraction or fractionated stereotactic radiotherapy for large brain metastases. A single centre study. Strahlenther Onkol. 188:696–701. 2012.
Article35. Yomo S, Hayashi M. A minimally invasive treatment option for large metastatic brain tumors: long-term results of two-session gamma knife stereotactic radiosurgery. Radiat Oncol. 9:132. 2014.
Article36. Yomo S, Hayashi M, Nicholson C. A prospective pilot study of two-session gamma knife surgery for large metastatic brain tumors. J Neurooncol. 109:159–165. 2012.
Article37. Zimmerman AL, Murphy ES, Suh JH, Vogelbaum MA, Barnett GH, Angelov L, et al. Treatment of large brain metastases with stereotactic radiosurgery. Technol Cancer Res Treat. 15:186–195. 2016.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to use Leksell GammaPlan
- Clinical Analysis of Gamma Knife Radiosurgery for Brain Metastases
- Letters to the Editor: Gamma Knife Radiosurgery for Brain Metastases in Patients Harboring Four or More Lesions : Survival and Prognostic Factors
- Stereotactic radiosurgery for brain metastases
- Normal pressure hydrocephalus after gamma knife radiosurgery in a patient with vestibular schwannoma