J Korean Neurosurg Soc.
2024 Sep;67(5):541-549. 10.3340/jkns.2024.0095.
Surgical Results with Low-Grade Arteriovenous Malformations : A Single Center 14-Year Experience
- Affiliations
-
- 1Department of Neurosurgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2558679
- DOI: http://doi.org/10.3340/jkns.2024.0095
Abstract
Objective
: Advancements in AVM surgical techniques for cerebral arteriovenous malformation (AVM) underscore its efficacy. Our research aims to showcase the positive outcomes of treating low-grade AVMs surgically, focusing on safety and effectiveness.
Methods
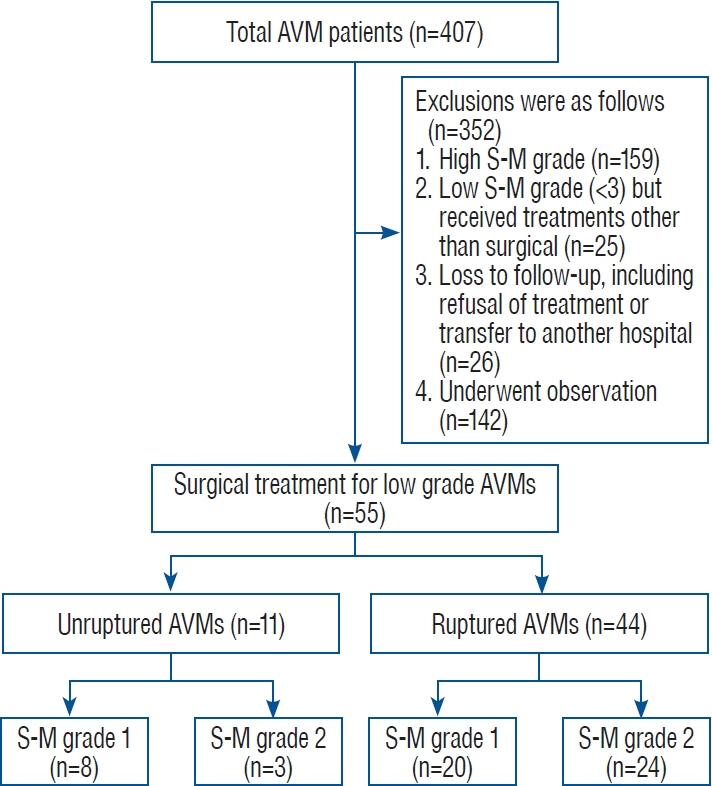
: We retrospectively reviewed 55 patients (36 males and 19 females; average age 37.4 years) with Spetzler-Martin (S-M) grade 1 and 2 AVMs who underwent surgical resection between January 2009 and December 2022.
Results
: In our study, 55 patients with S-M grade 1 and 2 AVMs underwent surgical resection, evenly divided between grades 1 (50.9%) and 2 (49.1%). Intracranial hemorrhage was the primary symptom in 74.5% of cases. Pre-operative Glasgow coma scale (GCS) scores revealed 69.1% of patients scored above 13, with 18% below 8. Successful resection was achieved in 87.3%. Postoperatively, 95.5% of ruptured and 90.9% of unruptured AVM patients showed lower or same modified Rankin scale scores. Poorer outcomes were significantly linked to lower GCS scores and intranidal/flow-related aneurysms through multivariate logistic regression. Postoperative seizures noted in nine patients, were exclusive to the ruptured AVM group.
Conclusion
: Our findings indicate surgical resection as a beneficial treatment for low-grade AVMs, yielding high cure rates and positive functional outcomes in both ruptured and unruptured cases. Preoperative GCS scores and the presence of associated aneurysms are predictive of postoperative functional status. Additionally, managing postoperative seizures effectively is key to enhancing prognosis.
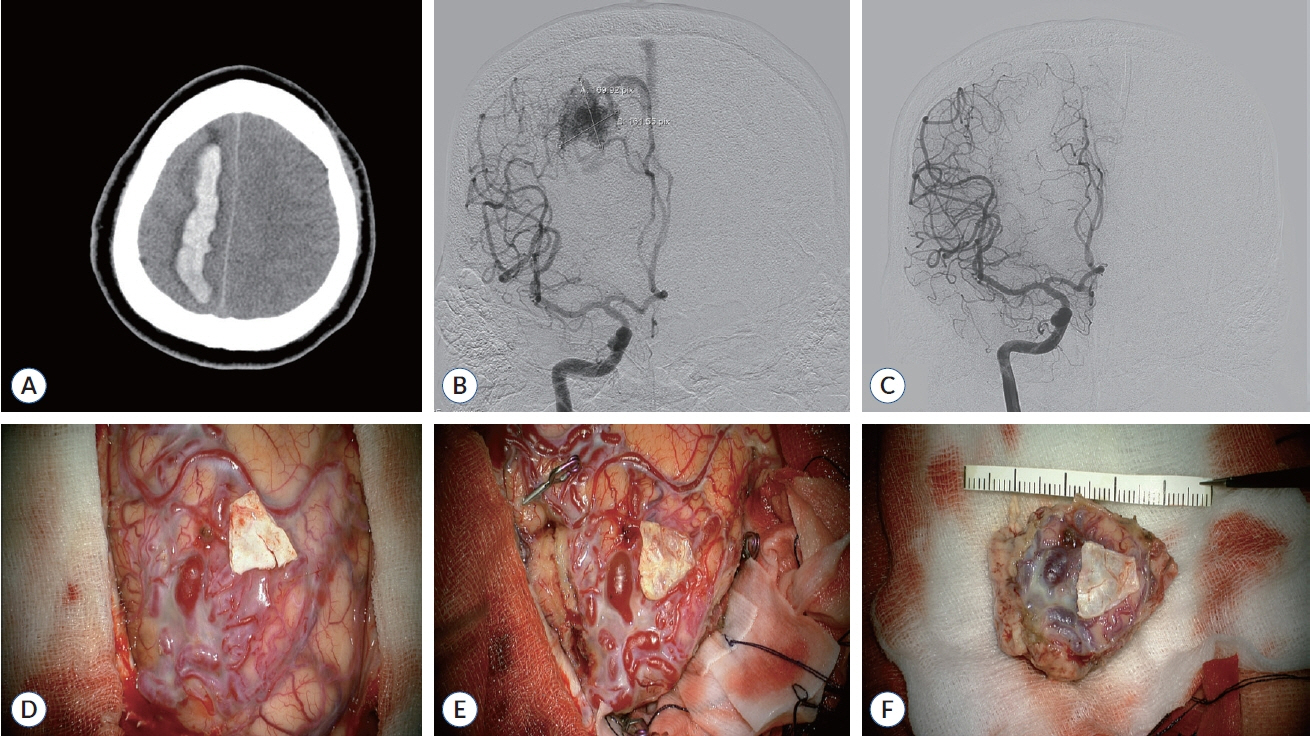
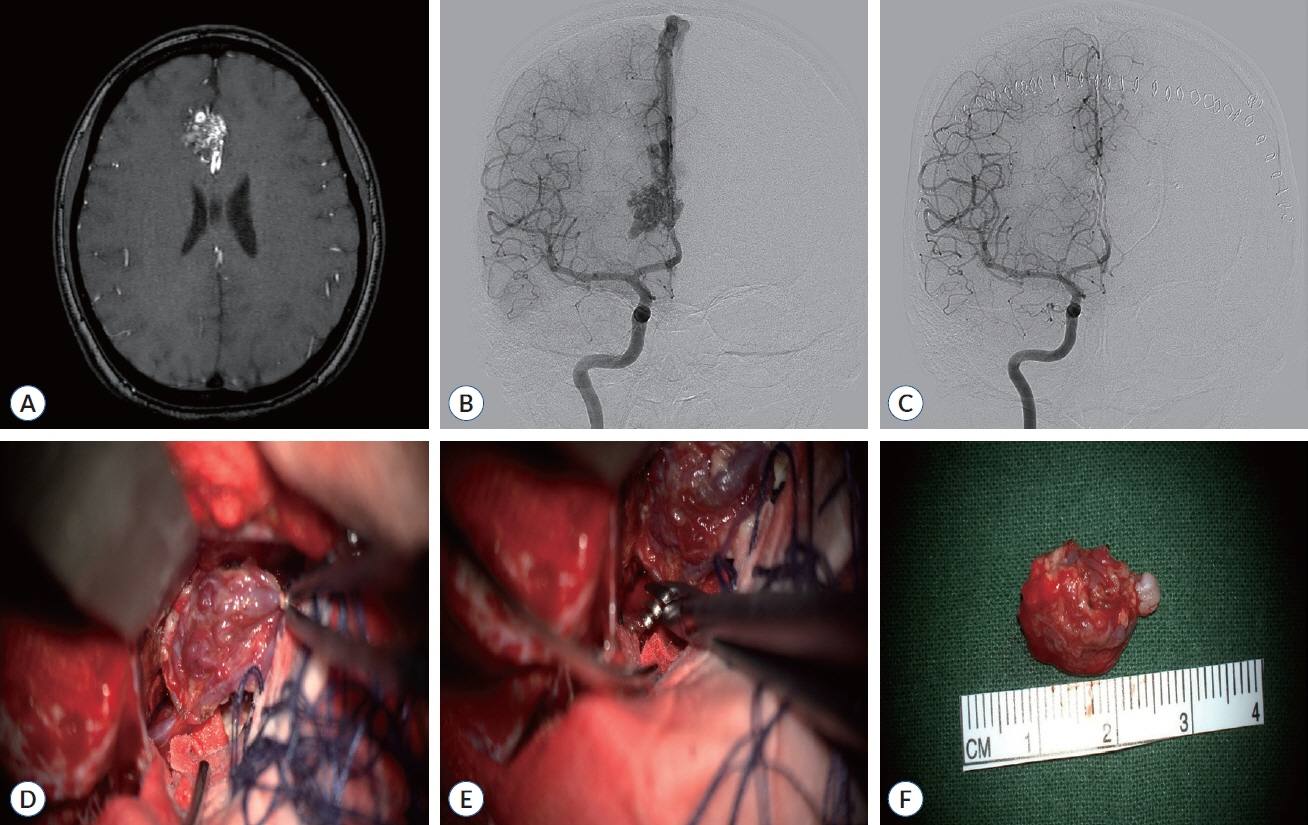
Figure
Reference
-
References
1. Baharvahdat H, Blanc R, Fahed R, Smajda S, Ciccio G, Desilles JP, et al. Endovascular treatment for low-grade (Spetzler-Martin I-II) brain arteriovenous malformations. AJNR Am J Neuroradiol. 40:668–672. 2019.2. Davies JM, Kim H, Young WL, Lawton MT. Classification schemes for arteriovenous malformations. Neurosurg Clin N Am. 23:43–53. 2012.
Article3. Englot DJ, Young WL, Han SJ, McCulloch CE, Chang EF, Lawton MT. Seizure predictors and control after microsurgical resection of supratentorial arteriovenous malformations in 440 patients. Neurosurgery. 71:572–580. discussion 580. 2012.4. Feghali J, Huang J. Updates in arteriovenous malformation management: the post-ARUBA era. Stroke Vasc Neurol. 5:34–39. 2019.5. Gami A, Feghali J, Rapaport S, Sattari SA, Yang W, Tamargo RJ, et al. Microsurgical resection versus stereotactic radiosurgery for low-grade intracranial arteriovenous malformations: a 27-year institutional experience. J Clin Neurosci. 94:209–215. 2021.
Article6. Gobin YP, Laurent A, Merienne L, Schlienger M, Aymard A, Houdart E, et al. Treatment of brain arteriovenous malformations by embolization and radiosurgery. J Neurosurg. 85:19–28. 1996.7. Guimaraes M, Wooster M. Onyx (ethylene-vinyl alcohol copolymer) in peripheral applications. Semin Intervent Radiol. 28:350–356. 2011.
Article8. Hamilton MG, Spetzler RF. The prospective application of a grading system for arteriovenous malformations. Neurosurgery. 34:2–6. discussion 6-7. 1994.
Article9. Josephson CB, Bhattacharya JJ, Counsell CE, Papanastassiou V, Ritchie V, Roberts R, et al. Seizure risk with AVM treatment or conservative management: prospective, population-based study. Neurology. 79:500–507. 2012.
Article10. Link TW, Winston G, Schwarz JT, Lin N, Patsalides A, Gobin P, et al. Treatment of unruptured brain arteriovenous malformations: a singlecenter experience of 86 patients and a critique of the a randomized trial of unruptured brain arteriovenous malformations (ARUBA) trial. World Neurosurg. 120:e1156–e1162. 2018.11. Mohr JP, Parides MK, Stapf C, Moquete E, Moy CS, Overbey JR, et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, nonblinded, randomised trial. Lancet. 383:614–621. 2014.12. Moon K, Levitt MR, Almefty RO, Nakaji P, Albuquerque FC, Zabramski JM, et al. Safety and efficacy of surgical resection of unruptured lowgrade arteriovenous malformations from the modern decade. Neurosurgery. 77:948–952. discussion 952-953. 2015.
Article13. Peschillo S, Caporlingua A, Colonnese C, Guidetti G. Brain AVMs: an endovascular, surgical, and radiosurgical update. ScientificWorldJournal. 2014:834931. 2014.
Article14. Potts MB, Lau D, Abla AA, Kim H, Young WL, Lawton MT, et al. Current surgical results with low-grade brain arteriovenous malformations. J Neurosurg. 122:912–920. 2015.
Article15. Razavi SAS, Mirbolouk MH, Gorji R, Ebrahimnia F, Sasannejad P, Zabihyan S, et al. Endovascular treatment as the first-line approach for cure of low-grade brain arteriovenous malformation. Neurosurg Focus. 53:E8. 2022.16. Rubin BA, Brunswick A, Riina H, Kondziolka D. Advances in radiosurgery for arteriovenous malformations of the brain. Neurosurgery 74 Suppl. 1:S50–S59. 2014.
Article17. Rutledge WC, Abla AA, Nelson J, Halbach VV, Kim H, Lawton MT. Treatment and outcomes of ARUBA-eligible patients with unruptured brain arteriovenous malformations at a single institution. Neurosurg Focus. 37:E8. 2014.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acquired Multiple Arteriovenous Malformations on the Scalp in the Patient of Liver Cirrhosis
- 3 Cases of Surgically Treated Arteriovenous Malformations of the Brain
- Staged Treatment of High Flow, Large Cerebral Arteriovenous Malformation with a Combination of Preoperative Embolization and Microsurgery
- Hemodynamics of Cerebral Arteriovenous Malformation
- Complications after Radiosurgery of the Cerebral Arteriovenous Malformation