Ewha Med J.
2024 Jul;47(3):e38. 10.12771/emj.2024.e38.
Air pollution, including PM10 , as a potential risk factor for the development of appendicitis in Korea: a case-crossover study
- Affiliations
-
- 1Advanced Biomedical Research Institute, Ewha Womans University Seoul Hospital, Seoul, Korea
- 2Department of Surgery, Ewha Womans University College of Medicine, Seoul, Korea
- 3Department of Environmental Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 4Institute of Ewha-SCL for Environmental Health, Ewha Womans University College of Medicine, Seoul, Korea
- 5Department of Human Systems Medicine, Seoul National University College of Medicine, Seoul, Korea
- 6Graduate Program in System Health Science and Engineering, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2558575
- DOI: http://doi.org/10.12771/emj.2024.e38
Abstract
Objectives
Interest in the association between particulate air pollution and appendicitis risk has been increasing in recent years, and previous studies have suggested a link between particulate matter ≤ 10 μm in diameter (PM10 ) and appendicitis. However, robust evidence is currently lacking. This study explored the association between short-term PM10 exposure and appendicitis using data from Ewha Womans University Mokdong Hospital, Seoul, Korea, between January 1, 2001 and December 31, 2018.
Methods
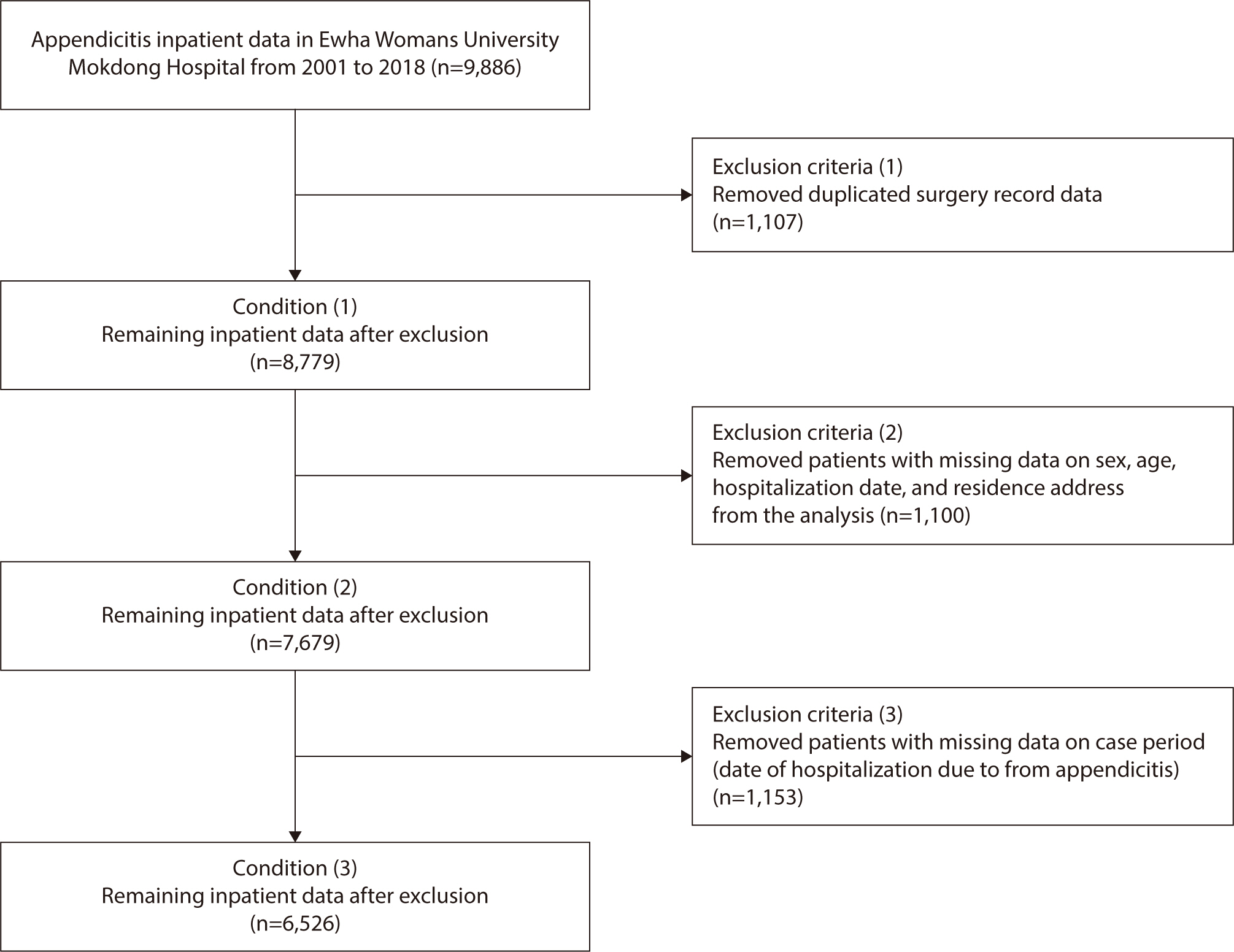
We employed a time-stratified case-crossover design using data from 6,526 appendicitis patients taken from the hospital’s electronic medical records system. We analyzed the data using a conditional logistic regression model adjusted for daily mean temperature and relative humidity. The effect size of PM10 was estimated in terms of each 10 μm/m3 increase in PM10 concentration. Sex, season, and age group were analyzed as subgroups.
Results
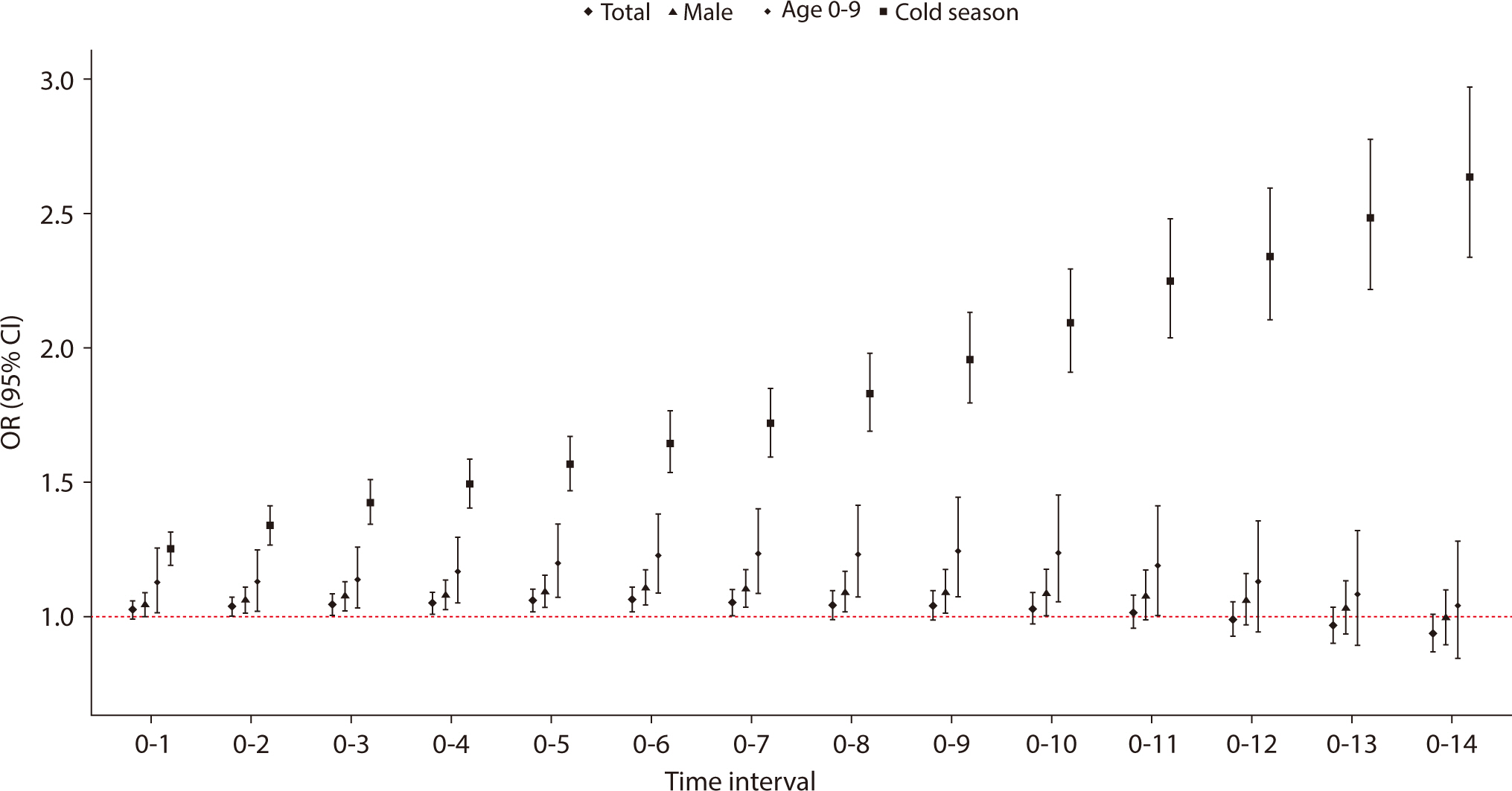
Appendicitis patients had been exposed to higher levels of PM10 concentrations 3 days (OR 1.045, 95% CI : 1.007–1.084) and 7 days (OR, 1.053; 95% CI, 1.005–1.103) before hospital admission. The case-crossover analysis stratified by sex, age, and season showed that the male sex, being aged under 10, and the cold season were associated with a significantly stronger association between appendicitis and PM10 concentrations.
Conclusion
Our study found that PM10 concentrations were associated with appendicitis in boys aged under 10. The cold season was also a risk factor. Further research with a larger sample size and with other pollutants is required to clarify the association between PM10 and appendicitis.
Figure
Reference
-
References
1. Sammalkorpi HE, Mentula P, Leppäniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis: a prospective study. BMC Gastroenterol. 2014; 14:114. DOI: 10.1186/1471-230X-14-114. PMID: 24970111. PMCID: PMC4087125.2. Lee JH, Park YS, Choi JS. The epidemiology of appendicitis and appendectomy in South Korea: national registry data. J Epidemiol. 2010; 20(2):97–105. DOI: 10.2188/jea.JE20090011. PMID: 20023368. PMCID: PMC3900807.3. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015; 386(10000):1278–1287. DOI: 10.1016/S0140-6736(15)00275-5. PMID: 26460662.4. Guo MY, Antonsen AN, Wiseman SM. The pathogenesis of appendicitis in 2022: more than just a fecalith. Am J Surg. 2023; 225(3):597–598. DOI: 10.1016/j.amjsurg.2022.10.021. PMID: 36307337.5. Williams GR. Presidential address: a history of appendicitis. With anecdotes illustrating its importance. Ann Surg. 1983; 197(5):495–506. DOI: 10.1097/00000658-198305000-00001. PMID: 6342553. PMCID: PMC1353017.6. Kaplan GG, Dixon E, Panaccione R, Fong A, Chen L, Szyszkowicz M, et al. Effect of ambient air pollution on the incidence of appendicitis. Can Med Assoc J. 2009; 181(9):591–597. DOI: 10.1503/cmaj.082068. PMID: 19805497. PMCID: PMC2764754.7. Chen CC, Yang CY. Effects of ambient air pollution exposure on frequency of hospital admissions for appendicitis in Taipei, Taiwan. J Toxicol Environ Health A. 2018; 81(17):854–860. DOI: 10.1080/15287394.2018.1498276. PMID: 30047832.8. Kim K, Kwak IY, Min H. Particulate matter 10 (PM10) is associated with epistaxis in children and adults. Int J Environ Res Public Health. 2021; 18(9):4809. DOI: 10.3390/ijerph18094809. PMID: 33946392. PMCID: PMC8124263.9. Kwak K, Kim JH. The association between air pollution and appendicitis: a systematic review and meta-analysis. J Epidemiol Community Health. 2017; 71(12):1263–1270.10. Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991; 133(2):144–153. DOI: 10.1093/oxfordjournals.aje.a115853. PMID: 1985444.11. Seo S, Kim J, Lee H, Jeong U, Kim W, Holben BN, et al. Estimation of PM10 concentrations over Seoul using multiple empirical models with AERONET and MODIS data collected during the DRAGON-Asia campaign. Atmos Chem Phys. 2015; 15(1):319–334. DOI: 10.5194/acp-15-319-2015.12. Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016; 16(10):626–638. DOI: 10.1038/nri.2016.90. PMID: 27546235.13. Zheng P, Zhang B, Zhang K, Lv X, Wang Q, Bai X. The impact of air pollution on intestinal microbiome of asthmatic children: a panel study. Biomed Res Int. 2020; 2020:5753427. DOI: 10.1155/2020/5753427. PMID: 33204702. PMCID: PMC7661118.14. Donaldson GC, Seemungal TA, Patel IS, Lloyd-Owen SJ, Wedzicha JA. Air pollution and other seasonal triggers of acute chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med. 2002; 166(8):1118–1123. DOI: 10.1164/rccm.2105081.15. Golz RA, Flum DR, Sanchez SE, Liu XH, Donovan C, Drake FT. Geographic association between incidence of acute appendicitis and socioeconomic status. JAMA Surg. 2020; 155(4):330–338. DOI: 10.1001/jamasurg.2019.6030. PMID: 32129808. PMCID: PMC7057178.16. Ji Y, Su X, Zhang F, Huang Z, Zhang X, Chen Y, et al. Impacts of short-term air pollution exposure on appendicitis admissions: evidence from one of the most polluted cities in mainland China. Front Public Health. 2023; 11:1144310. DOI: 10.3389/fpubh.2023.1144310. PMID: 37006531. PMCID: PMC10061118.17. Aroui H, Kalboussi H, El Ghali A, Kacem I, Maoua M, Maatoug J, et al. The effect of environmental factors on the incidence of perforated appendicitis. Ann Ital Chir. 2018; 89(5):431–437.18. McGowan JA, Hider PN, Chacko E, Town GI. Particulate air pollution and hospital admissions in Christchurch, New Zealand. Aust N Z J Public Health. 2002; 26(1):23–29. DOI: 10.1111/j.1467-842X.2002.tb00266.x. PMID: 11895020.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Update in Association between Lung Cancer and Air Pollution
- Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea
- Adverse Effects of Air Pollution on Pulmonary Diseases
- Estimation of Attributable Risk and Direct Medical and Non-Medical Costs of Major Mental Disorders Associated With Air Pollution Exposures Among Children and Adolescents in the Republic of Korea, 2011–2019
- Public-health impact of outdoor air pollution for 2nd air pollution management policy in Seoul metropolitan area, Korea