J Korean Med Sci.
2024 Aug;39(30):e218. 10.3346/jkms.2024.39.e218.
Estimation of Attributable Risk and Direct Medical and Non-Medical Costs of Major Mental Disorders Associated With Air Pollution Exposures Among Children and Adolescents in the Republic of Korea, 2011–2019
- Affiliations
-
- 1Department of Public Health, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Healthcare Management, Graduate School of Public Health, Yonsei University, Seoul, Korea
- 3Department of Precision Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 4Department of Preventive Medicine and Institute of Medical Sciences, College of Medicine, Gyeongsang National University, Jinju, Korea
- 5Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- 6Institute for Environmental Research, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2558518
- DOI: http://doi.org/10.3346/jkms.2024.39.e218
Abstract
- Background
Recent studies have reported the burden of attention deficit hyperactivity disorder [ADHD], autism spectrum disorder [ASD], and depressive disorder. Also, there is mounting evidence on the effects of environmental factors, such as ambient air pollution, on these disorders among children and adolescents. However, few studies have evaluated the burden of mental disorders attributable to air pollution exposure in children and adolescents.
Methods
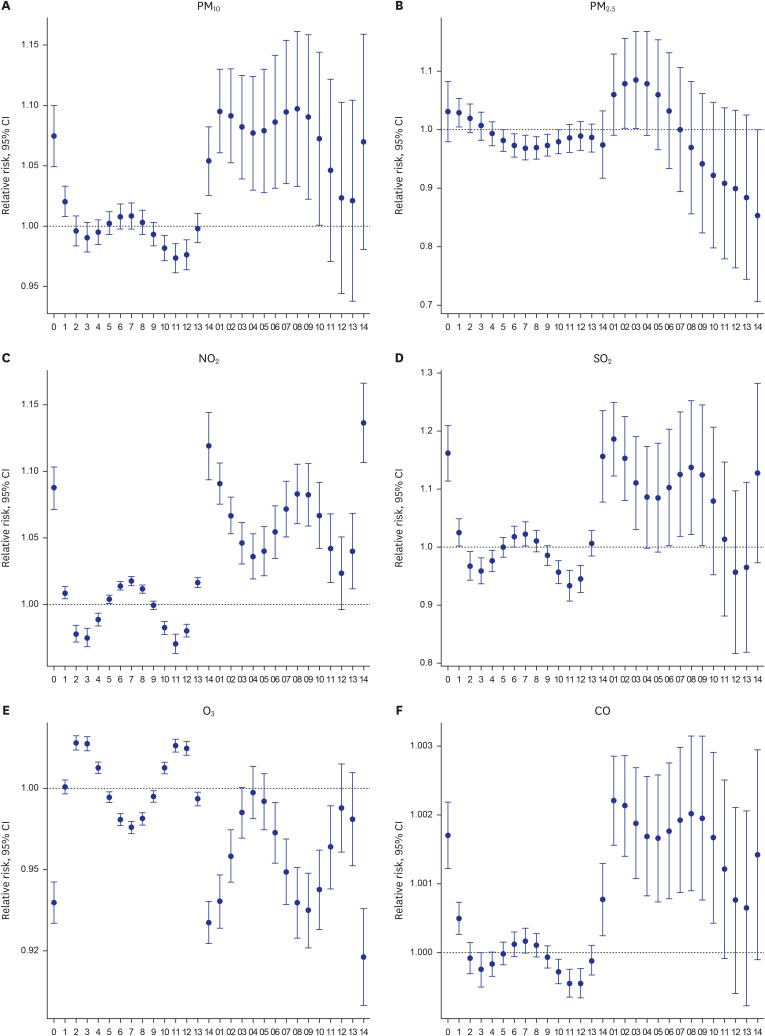
We estimated the risk ratios of major mental disorders (ADHD, ASD, and depressive disorder) associated with air pollutants among children and adolescents using time-series data (2011–2019) obtained from a nationwide air pollution monitoring network and healthcare utilization claims data in the Republic of Korea. Based on the estimated risk ratios, we determined the population attributable fraction (PAF) and calculated the medical costs of major mental disorders attributable to air pollution.
Results
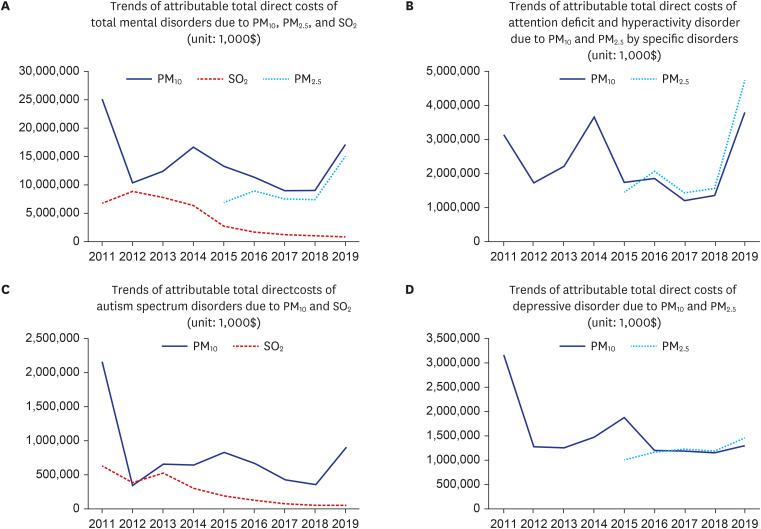
A total of 33,598 patients were diagnosed with major mental disorders during 9 years. The PAFs for all the major mental disorders were estimated at 6.9% (particulate matter < 10 μm [PM10 ]), 3.7% (PM2.5 ), and 2.2% (sulfur dioxide [SO2 ]). The PAF of PM10 was highest for depressive disorder (9.2%), followed by ASD (8.4%) and ADHD (5.2%). The direct medical costs of all major mental disorders attributable to PM10 and SO2 decreased during the study period.
Conclusion
This study assessed the burden of major mental disorders attributable to air pollution exposure in children and adolescents. We found that PM10, PM2.5 , and SO2 attributed 7%, 4%, and 2% respectively, to the risk of major mental disorders among children and adolescents.
Keyword
Figure
Reference
-
1. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022; 9(2):137–150. PMID: 35026139.2. Bitsko RH, Claussen AH, Lichstein J, Black LI, Jones SE, Danielson ML, et al. Mental health surveillance among children - United States, 2013-2019. MMWR Suppl. 2022; 71(2):1–42.3. Park JH, Yoon SJ, Lee HY, Cho HS, Lee JY, Eun SJ, et al. Estimating the burden of psychiatric disorder in Korea. J Prev Med Public Health. 2006; 39(1):39–45. PMID: 16613070.4. Li Z, Yang L, Chen H, Fang Y, Zhang T, Yin X, et al. Global, regional and national burden of autism spectrum disorder from 1990 to 2019: results from the Global Burden of Disease Study 2019. Epidemiol Psychiatr Sci. 2022; 31:e33. PMID: 35535764.5. Hong M, Lee SM, Park S, Yoon SJ, Kim YE, Oh IH. Prevalence and economic burden of autism spectrum disorder in South Korea using National Health Insurance data from 2008 to 2015. J Autism Dev Disord. 2020; 50(1):333–339. PMID: 31630294.6. Kim GE, Jo MW, Shin YW. Increased prevalence of depression in South Korea from 2002 to 2013. Sci Rep. 2020; 10(1):16979. PMID: 33046758.7. Tkacz J, Brady BL. Increasing rate of diagnosed childhood mental illness in the United States: incidence, prevalence and costs. Public Health Pract (Oxf). 2021; 2:100204. PMID: 36101631.8. Thygesen M, Holst GJ, Hansen B, Geels C, Kalkbrenner A, Schendel D, et al. Exposure to air pollution in early childhood and the association with attention-deficit hyperactivity disorder. Environ Res. 2020; 183:108930. PMID: 31810593.9. Jung CR, Lin YT, Hwang BF. Air pollution and newly diagnostic autism spectrum disorders: a population-based cohort study in Taiwan. PLoS One. 2013; 8(9):e75510. PMID: 24086549.10. Park J, Sohn JH, Cho SJ, Seo HY, Hwang IU, Hong YC, et al. Association between short-term air pollution exposure and attention-deficit/hyperactivity disorder-related hospital admissions among adolescents: a nationwide time-series study. Environ Pollut. 2020; 266(Pt 1):115369. PMID: 32810816.11. Kim KN, Sohn JH, Cho SJ, Seo HY, Kim S, Hong YC. Effects of short-term exposure to air pollution on hospital admissions for autism spectrum disorder in Korean school-aged children: a nationwide time-series study. BMJ Open. 2022; 12(9):e058286.12. Wu Z, Chen X, Li G, Tian L, Wang Z, Xiong X, et al. Attributable risk and economic cost of hospital admissions for mental disorders due to PM2.5 in Beijing. Sci Total Environ. 2020; 718:137274. PMID: 32109812.13. Qiu H, Wang L, Luo L, Shen M. Gaseous air pollutants and hospitalizations for mental disorders in 17 Chinese cities: association, morbidity burden and economic costs. Environ Res. 2022; 204(Pt A):111928. PMID: 34437848.14. Gao X, Jiang W, Liao J, Li J, Yang L. Attributable risk and economic cost of hospital admissions for depression due to short-exposure to ambient air pollution: a multi-city time-stratified case-crossover study. J Affect Disord. 2022; 304:150–158. PMID: 35219742.15. Zhang P, Zhou X. Health and economic impacts of particulate matter pollution on hospital admissions for mental disorders in Chengdu, Southwestern China. Sci Total Environ. 2020; 733:139114. PMID: 32447079.16. Kim CB, Ock M, Jung YS, Kim KB, Kim YE, Kim KA, et al. Estimation of years lived with disability using a prevalence-based approach: application to major psychiatric disease in Korea. Int J Environ Res Public Health. 2021; 18(17):9056. PMID: 34501645.17. Korean Statistical Information Service (KOSIS). Population of the Middle of the Year. Daejeon, Korea: KOSIS;2022.18. Dominici F, McDermott A, Zeger SL, Samet JM. On the use of generalized additive models in time-series studies of air pollution and health. Am J Epidemiol. 2002; 156(3):193–203. PMID: 12142253.19. Qiu H, Zhu X, Wang L, Pan J, Pu X, Zeng X, et al. Attributable risk of hospital admissions for overall and specific mental disorders due to particulate matter pollution: a time-series study in Chengdu, China. Environ Res. 2019; 170:230–237. PMID: 30594694.20. Gao Q, Xu Q, Guo X, Fan H, Zhu H. Particulate matter air pollution associated with hospital admissions for mental disorders: a time-series study in Beijing, China. Eur Psychiatry. 2017; 44:68–75. PMID: 28545011.21. Zhao Y, Wang S, Lang L, Huang C, Ma W, Lin H. Ambient fine and coarse particulate matter pollution and respiratory morbidity in Dongguan, China. Environ Pollut. 2017; 222:126–131. PMID: 28041838.22. Li Z, Liu M, Wu Z, Liu Y, Li W, Liu M, et al. Association between ambient air pollution and hospital admissions, length of hospital stay and hospital cost for patients with cardiovascular diseases and comorbid diabetes mellitus: base on 1,969,755 cases in Beijing, China, 2014-2019. Environ Int. 2022; 165:107301. PMID: 35598418.23. World Health Organization Regional Office for Europe. Air Quality Guidelines: Global Update 2005: Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide. Copenhagen, Denmark: World Health Organization Regional Office for Europe;2006.24. World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. Geneva, Switzerland: World Health Organization;2021.25. National Health Insurance Service (KO). Medical Aid Statistics. Wonju, Korea: National Health Insurance Service;2020.26. Braithwaite I, Zhang S, Kirkbride JB, Osborn DP, Hayes JF. Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta-analysis. Environ Health Perspect. 2019; 127(12):126002. PMID: 31850801.27. Dutheil F, Comptour A, Morlon R, Mermillod M, Pereira B, Baker JS, et al. Autism spectrum disorder and air pollution: a systematic review and meta-analysis. Environ Pollut. 2021; 278:116856. PMID: 33714060.28. Liu Q, Wang W, Gu X, Deng F, Wang X, Lin H, et al. Association between particulate matter air pollution and risk of depression and suicide: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2021; 28(8):9029–9049. PMID: 33481201.29. Lee S, Lee W, Kim D, Kim E, Myung W, Kim SY, et al. Short-term PM2.5 exposure and emergency hospital admissions for mental disease. Environ Res. 2019; 171:313–320. PMID: 30711732.30. Kim C, Jung SH, Kang DR, Kim HC, Moon KT, Hur NW, et al. Ambient particulate matter as a risk factor for suicide. Am J Psychiatry. 2010; 167(9):1100–1107. PMID: 20634364.31. Wang F, Liu H, Li H, Liu J, Guo X, Yuan J, et al. Ambient concentrations of particulate matter and hospitalization for depression in 26 Chinese cities: a case-crossover study. Environ Int. 2018; 114:115–122. PMID: 29500987.32. Cheng Y, Meng Y, Li X, Yin J. Effects of ambient air pollution on the hospitalization risk and economic burden of mental disorders in Qingdao, China. Int Arch Occup Environ Health. 2024; 97(2):109–120. PMID: 38062177.33. Ajmani GS, Suh HH, Wroblewski KE, Kern DW, Schumm LP, McClintock MK, et al. Fine particulate matter exposure and olfactory dysfunction among urban-dwelling older US adults. Environ Res. 2016; 151:797–803. PMID: 27692900.34. Block ML, Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009; 32(9):506–516. PMID: 19716187.35. Fan HC, Chen CM, Tsai JD, Chiang KL, Tsai SC, Huang CY, et al. Association between exposure to particulate matter air pollution during early childhood and risk of attention-deficit/hyperactivity disorder in Taiwan. Int J Environ Res Public Health. 2022; 19(23):16138. PMID: 36498210.36. Fuertes E, Standl M, Forns J, Berdel D, Garcia-Aymerich J, Markevych I, et al. Traffic-related air pollution and hyperactivity/inattention, dyslexia and dyscalculia in adolescents of the German GINIplus and LISAplus birth cohorts. Environ Int. 2016; 97:85–92. PMID: 27835751.37. Ceylan MF, Sener S, Bayraktar AC, Kavutcu M. Changes in oxidative stress and cellular immunity serum markers in attention-deficit/hyperactivity disorder. Psychiatry Clin Neurosci. 2012; 66(3):220–226. PMID: 22443244.38. Allen JL, Oberdorster G, Morris-Schaffer K, Wong C, Klocke C, Sobolewski M, et al. Developmental neurotoxicity of inhaled ambient ultrafine particle air pollution: parallels with neuropathological and behavioral features of autism and other neurodevelopmental disorders. Neurotoxicology. 2017; 59:140–154. PMID: 26721665.39. Ahadullah , Yau SY, Lu HX, Lee TM, Guo H, Chan CC. PM2.5 as a potential risk factor for autism spectrum disorder: its possible link to neuroinflammation, oxidative stress and changes in gene expression. Neurosci Biobehav Rev. 2021; 128:534–548. PMID: 34216652.40. Yang T, Wang J, Huang J, Kelly FJ, Li G. Long-term exposure to multiple ambient air pollutants and association with incident depression and anxiety. JAMA Psychiatry. 2023; 80(4):305–313. PMID: 36723924.41. Gao X, Jiang M, Huang N, Guo X, Huang T. Long-term air pollution, genetic susceptibility, and the risk of depression and anxiety: a prospective study in the UK Biobank cohort. Environ Health Perspect. 2023; 131(1):17002. PMID: 36598457.42. Lavelle TA, Weinstein MC, Newhouse JP, Munir K, Kuhlthau KA, Prosser LA. Economic burden of childhood autism spectrum disorders. Pediatrics. 2014; 133(3):e520–e529. PMID: 24515505.43. Hong M, Park B, Lee SM, Bahn GH, Kim MJ, Park S, et al. Economic burden and disability-adjusted life years (DALYs) of attention deficit/hyperactivity disorder. J Atten Disord. 2020; 24(6):823–829. PMID: 31364445.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adverse Effects of Air Pollution on Pulmonary Diseases
- Risk-Based Damage Cost Estimation on Mortality Due to Environmental Problems
- Mental Disorders in Adolescents
- Public-health impact of outdoor air pollution for 2nd air pollution management policy in Seoul metropolitan area, Korea
- Review of epidemiological studies on air pollution and health effects in children