Korean Circ J.
2024 Aug;54(8):454-465. 10.4070/kcj.2024.0006.
Clinical Outcomes After Drug-Coated Balloon Treatment in Popliteal Artery Disease: K-POP Registry 12-Month Results
- Affiliations
-
- 1Division of Cardiology, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu, Korea
- 2Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Cardiology, Korea University Guro Hospital, Seoul, Korea
- 4Division of Cardiology, Korea University Anam Hospital, Seoul, Korea
- 5Division of Cardiology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 6Division of Cardiology, Soonchunhyang University Cheonan Hospital, Cheonan, Korea
- 7Division of Cardiology, Chungnam National University Sejong Hospital, Sejong, Korea
- 8Division of Cardiology, Busan Veterans Hospital, Busan, Korea
- KMID: 2558536
- DOI: http://doi.org/10.4070/kcj.2024.0006
Abstract
- Background and Objectives
The popliteal artery is generally regarded as a “no-stent zone.” Limited data are available on the outcomes of drug-coated balloons (DCBs) for popliteal artery disease. This study aimed to evaluate the 12-month clinical outcomes among patients who received DCB treatment for atherosclerotic popliteal artery disease.
Methods
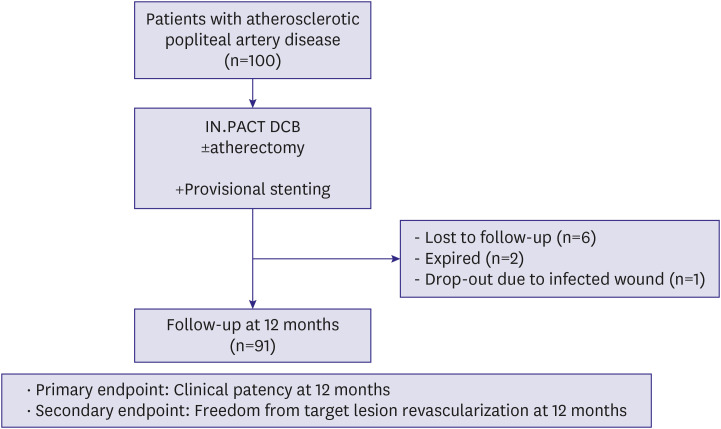
This prospective, multicenter registry study enrolled 100 patients from 7 Korean endovascular centers who underwent endovascular therapy using IN.PACT DCB (Medtronic) for symptomatic atherosclerotic popliteal artery disease. The primary endpoint was 12-month clinical primary patency and the secondary endpoint was clinically driven target lesion revascularization (TLR)–free rate.
Results
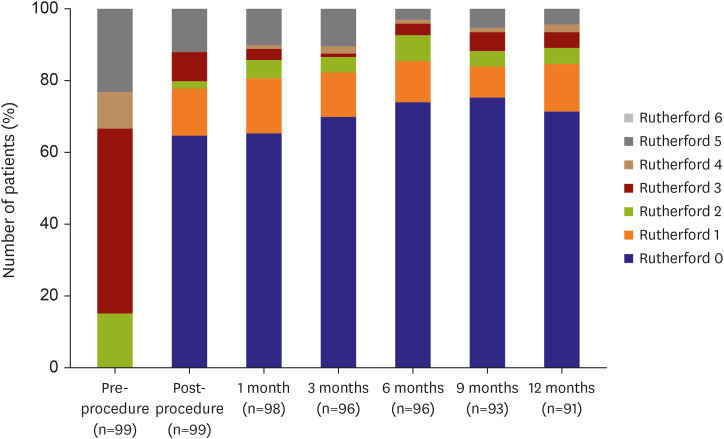
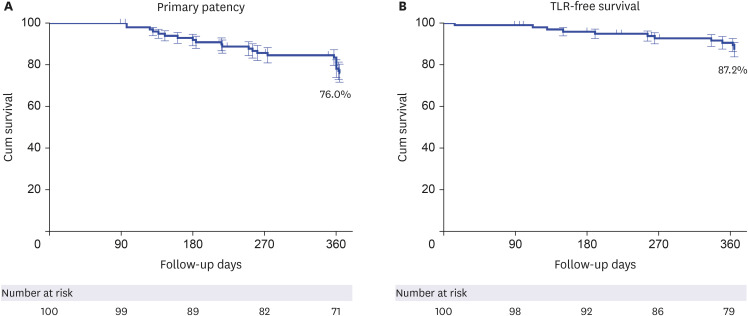
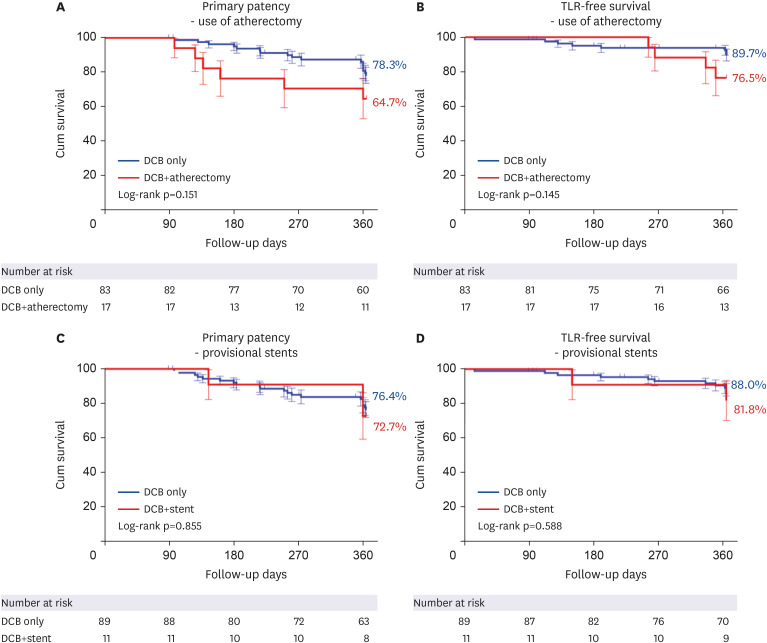
The mean age of the study cohort was 65.7±10.8 years, and 77% of enrolled patients were men. The mean lesion length was 93.7±53.7 mm, and total occlusions were present in 45% of patients. Technical success was achieved in all patients. Combined atherectomy was performed in 17% and provisional stenting was required in 11%. Out of the enrolled patients, 91 patients completed the 12-month follow-up. Clinical primary patency and TLR-free survival rates at 12 months were 76.0% and 87.2%, respectively. A multivariate Cox regression analysis identified female and longer lesion length as the significant independent predictors of loss of patency.
Conclusions
DCB treatment yielded favorable 12-month clinical primary patency and TLRfree survival outcomes in patients with popliteal artery disease.
Keyword
Figure
Reference
-
1. Kröger K, Santosa F, Goyen M. Biomechanical incompatibility of popliteal stent placement. J Endovasc Ther. 2004; 11:686–694. PMID: 15615559.2. Hoffmann U, Vetter J, Rainoni L, Leu AJ, Bollinger A. Popliteal artery compression and force of active plantar flexion in young healthy volunteers. J Vasc Surg. 1997; 26:281–287. PMID: 9279316.3. Tamashiro GA, Tamashiro A, Villegas MO, et al. Flexions of the popliteal artery: technical considerations of femoropopliteal stenting. J Invasive Cardiol. 2011; 23:431–433. PMID: 21972163.4. Poulson W, Kamenskiy A, Seas A, Deegan P, Lomneth C, MacTaggart J. Limb flexion-induced axial compression and bending in human femoropopliteal artery segments. J Vasc Surg. 2018; 67:607–613. PMID: 28526560.5. Gökgöl C, Diehm N, Kara L, Büchler P. Quantification of popliteal artery deformation during leg flexion in subjects with peripheral artery disease: a pilot study. J Endovasc Ther. 2013; 20:828–835. PMID: 24325701.6. Tosaka A, Soga Y, Iida O, et al. Classification and clinical impact of restenosis after femoropopliteal stenting. J Am Coll Cardiol. 2012; 59:16–23. PMID: 22192663.7. Tepe G, Laird J, Schneider P, et al. Drug-coated balloon versus standard percutaneous transluminal angioplasty for the treatment of superficial femoral and popliteal peripheral artery disease: 12-month results from the IN.PACT SFA randomized trial. Circulation. 2015; 131:495–502. PMID: 25472980.8. Giacoppo D, Cassese S, Harada Y, et al. Drug-coated balloon versus plain balloon angioplasty for the treatment of femoropopliteal artery disease: an updated systematic review and meta-analysis of randomized clinical trials. JACC Cardiovasc Interv. 2016; 9:1731–1742. PMID: 27539695.9. Caradu C, Lakhlifi E, Colacchio EC, et al. Systematic review and updated meta-analysis of the use of drug-coated balloon angioplasty versus plain old balloon angioplasty for femoropopliteal arterial disease. J Vasc Surg. 2019; 70:981–995.e10. PMID: 31126769.10. Cha JJ, Lee JH, Ko YG, et al. Clinical outcomes of atherectomy plus drug-coated balloon versus drug-coated balloon alone in the treatment of femoropopliteal artery disease. Korean Circ J. 2022; 52:123–133. PMID: 34877824.11. Cummings P, Rivara FP, Koepsell TD. Writing informative abstracts for journal articles. Arch Pediatr Adolesc Med. 2004; 158:1086–1088. PMID: 15520348.12. Rastan A, Krankenberg H, Baumgartner I, et al. Stent placement versus balloon angioplasty for the treatment of obstructive lesions of the popliteal artery: a prospective, multicenter, randomized trial. Circulation. 2013; 127:2535–2541. PMID: 23694965.13. San Norberto EM, Flota CM, Fidalgo-Domingos L, Taylor JH, Vaquero C. Real-world results of Supera stent implantation for popliteal artery atherosclerotic lesions: 3-year outcome. Ann Vasc Surg. 2020; 62:397–405. PMID: 31449958.14. Scheinert D, Werner M, Scheinert S, et al. Treatment of complex atherosclerotic popliteal artery disease with a new self-expanding interwoven nitinol stent: 12-month results of the Leipzig SUPERA popliteal artery stent registry. JACC Cardiovasc Interv. 2013; 6:65–71. PMID: 23347863.15. Goltz JP, Ritter CO, Kellersmann R, Klein D, Hahn D, Kickuth R. Endovascular treatment of popliteal artery segments P1 and P2 in patients with critical limb ischemia: initial experience using a helical nitinol stent with increased radial force. J Endovasc Ther. 2012; 19:450–456. PMID: 22788900.16. Wu X, Peng Z, Qin J, Yang X, Lu X, Ye K. Outcomes of drug-coated balloon angioplasty for isolated chronic occlusion of the popliteal artery: a retrospective single-institution study. J Vasc Interv Radiol. 2021; 32:593–601. PMID: 33531180.17. Torsello G, Stavroulakis K, Brodmann M, et al. Three-year sustained clinical efficacy of drug-coated balloon angioplasty in a real-world femoropopliteal cohort. J Endovasc Ther. 2020; 27:693–705. PMID: 32583749.18. Stavroulakis K, Schwindt A, Torsello G, et al. Directional atherectomy with antirestenotic therapy vs drug-coated balloon angioplasty alone for isolated popliteal artery lesions. J Endovasc Ther. 2017; 24:181–188. PMID: 28008792.19. Rastan A, McKinsey JF, Garcia LA, et al. One-year outcomes following directional atherectomy of popliteal artery lesions: subgroup analysis of the prospective, multicenter DEFINITIVE LE trial. J Endovasc Ther. 2018; 25:100–108. PMID: 29117818.20. McKinsey JF, Zeller T, Rocha-Singh KJ, Jaff MR, Garcia LA. DEFINITIVE LE Investigators. Lower extremity revascularization using directional atherectomy: 12-month prospective results of the DEFINITIVE LE study. JACC Cardiovasc Interv. 2014; 7:923–933. PMID: 25147039.21. Spiliopoulos S, Kitrou P, Galanakis N, et al. Incidence and endovascular treatment of isolated atherosclerotic popliteal artery disease: outcomes from the IPAD multicenter study. Cardiovasc Intervent Radiol. 2018; 41:1481–1487. PMID: 29992345.22. Kohi MP, Brodmann M, Zeller T, et al. Sex-related differences in the long-term outcomes of patients with femoropopliteal arterial disease treated with the IN.PACT drug-coated balloon in the IN.PACT SFA randomized controlled trial: a post hoc analysis. J Vasc Interv Radiol. 2020; 31:1410–1418.e10. PMID: 32868016.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sex-Related Outcomes of Successful Drug-Coated Balloon Treatment in De Novo Coronary Artery Disease
- Endovascular Treatment of Arteriovenous Fistula with Pseudoaneurysm at Popliteal Fossa Using a PTFE Stent-graft: A Case Report
- Successful Interventional Treatment of a Huge Pseudoaneurysm of the Popliteal Artery Caused by a Percutaneous Balloon Angioplasty Complication: A Case Report
- Clinical Outcomes of Atherectomy Plus Drug-coated Balloon Versus Drugcoated Balloon Alone in the Treatment of Femoropopliteal Artery Disease
- Drug-Coated Balloon Treatment for De Novo Coronary Artery Disease