J Korean Med Sci.
2024 Aug;39(32):e232. 10.3346/jkms.2024.39.e232.
Associations Between COVID-19, Delirium, and 1-Year Mortality: Exploring Influences on Delirium Incidence in COVID-19 Patients
- Affiliations
-
- 1Department of Neuropsychiatry, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Psychiatry, Seoul National University College of Medicine, Seoul, Korea
- 3Big Data Center, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2558531
- DOI: http://doi.org/10.3346/jkms.2024.39.e232
Abstract
- Background
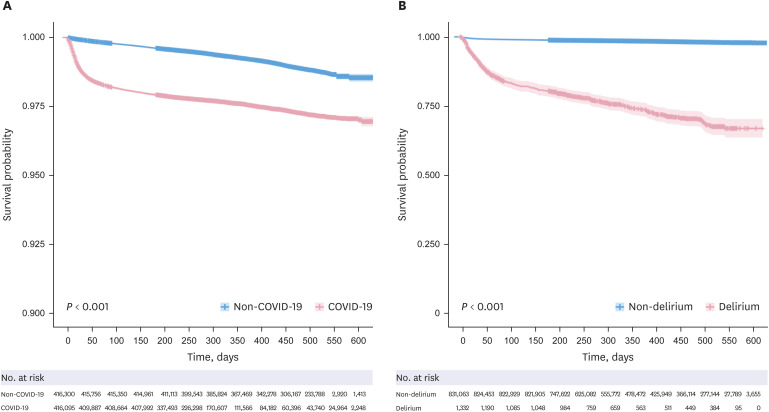
This study investigated the relationship between coronavirus disease 2019 (COVID-19), delirium, and 1-year mortality. Factors associated with delirium in COVID-19 patients were identified, along with the influence of psychotropic medications on delirium.
Methods
The study used the South Korean National Health Insurance Service database. Adult COVID-19 patients diagnosed between October 2020 and December 2021 were included, with a propensity score-matched control group. Time-dependent Cox regression assessed associations among COVID-19, delirium, and mortality. Logistic regression analyzed the impact of psychotropic medications on delirium incidence.
Results
The study included 832,602 individuals, with 416,301 COVID-19 patients. COVID-19 (hazard ratio [HR], 3.03; 95% confidence interval [CI], 2.92–3.13) and delirium (HR, 2.33; 95% CI, 2.06–2.63) were independent risk factors for 1-year mortality. Comorbidities, insurance type, and residence were also related to mortality. Among COVID-19 patients, antipsychotic use was associated with lower delirium incidence (odds ratio [OR], 0.38; 95% CI, 0.30–0.47), while mood stabilizers (OR, 1.77; 95% CI, 1.40–2.21) and benzodiazepines (OR, 8.62; 95% CI, 7.46–9.97) were linked to higher delirium incidence.
Conclusion
COVID-19 and delirium are risk factors for 1-year mortality. Some factors associated with delirium in COVID-19 patients are modifiable and can be targeted in preventive and therapeutic interventions.
Keyword
Figure
Reference
-
1. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998; 13(4):234–242. PMID: 9565386.2. Pranata R, Huang I, Lim MA, Yonas E, Vania R, Kuswardhani RA. Delirium and mortality in coronavirus disease 2019 (COVID-19)–a systematic review and meta-analysis. Arch Gerontol Geriatr. 2021; 95:104388. PMID: 33713880.3. Baller EB, Hogan CS, Fusunyan MA, Ivkovic A, Luccarelli JW, Madva E, et al. Neurocovid: pharmacological recommendations for delirium associated with COVID-19. Psychosomatics. 2020; 61(6):585–596. PMID: 32828569.4. White L, Jackson T. Delirium and COVID-19: a narrative review of emerging evidence. Anaesthesia. 2022; 77(S1):Suppl 1. 49–58. PMID: 35001383.5. Hosp JA, Dressing A, Blazhenets G, Bormann T, Rau A, Schwabenland M, et al. Cognitive impairment and altered cerebral glucose metabolism in the subacute stage of COVID-19. Brain. 2021; 144(4):1263–1276. PMID: 33822001.6. Hariyanto TI, Putri C, Hananto JE, Arisa J, Fransisca V Situmeang R, Kurniawan A. Delirium is a good predictor for poor outcomes from coronavirus disease 2019 (COVID-19) pneumonia: A systematic review, meta-analysis, and meta-regression. J Psychiatr Res. 2021; 142:361–368. PMID: 34425488.7. Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, MacLullich AM, et al. Delirium. Nat Rev Dis Primers. 2020; 6(1):90. PMID: 33184265.8. Pun BT, Badenes R, Heras La Calle G, Orun OM, Chen W, Raman R, et al. COVID-19 Intensive Care International Study Group. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study. Lancet Respir Med. 2021; 9(3):239–250. PMID: 33428871.9. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009; 5(4):210–220. PMID: 19347026.10. Saxena S, Lawley D. Delirium in the elderly: a clinical review. Postgrad Med J. 2009; 85(1006):405–413. PMID: 19633006.11. Burry L, Hutton B, Williamson DR, Mehta S, Adhikari NK, Cheng W, et al. Pharmacological interventions for the treatment of delirium in critically ill adults. Cochrane Database Syst Rev. 2019; 9(9):CD011749. PMID: 31479532.12. Maust DT, Blow FC, Wiechers IR, Kales HC, Marcus SC. National trends in antidepressant, benzodiazepine, and other sedative-hypnotic treatment of older adults in psychiatric and primary care. J Clin Psychiatry. 2017; 78(4):e363–e371. PMID: 28448697.13. Cho H, Choi J, Kim YS, Son SJ, Lee KS, Hwang HJ, et al. Prevalence and predictors of potentially inappropriate prescribing of central nervous system and psychotropic drugs among elderly patients: A national population study in Korea. Arch Gerontol Geriatr. 2018; 74:1–8. PMID: 28917110.14. Larsen CS. Assessing the proportion of the Danish population at risk of clinically significant drug-drug interactions with new oral antivirals for early treatment of COVID-19. Int J Infect Dis. 2022; 122:599–601. PMID: 35803465.15. Kok L, Slooter AJ, Hillegers MH, van Dijk D, Veldhuijzen DS. Benzodiazepine use and neuropsychiatric outcomes in the ICU: a systematic review. Crit Care Med. 2018; 46(10):1673–1680. PMID: 29985215.16. Reisinger M, Reininghaus EZ, Biasi J, Fellendorf FT, Schoberer D. Delirium-associated medication in people at risk: A systematic update review, meta-analyses, and GRADE-profiles. Acta Psychiatr Scand. 2023; 147(1):16–42. PMID: 36168988.17. Youn YC, Shin HW, Choi BS, Kim S, Lee JY, Ha YC. Rivastigmine patch reduces the incidence of postoperative delirium in older patients with cognitive impairment. Int J Geriatr Psychiatry. 2017; 32(10):1079–1084. PMID: 27561376.18. Tampi RR, Tampi DJ, Ghori AK. Acetylcholinesterase inhibitors for delirium in older adults. Am J Alzheimers Dis Other Demen. 2016; 31(4):305–310. PMID: 26646113.19. Massoudi N, Mohit B, Fathi M, Nooraei N, Hannani KK, ArianNik M. The impact of rivastigmine on post-surgical delirium and cognitive impairment; a randomized clinical trial. Int J Geriatr Psychiatry. 2023; 38(7):e5970. PMID: 37485727.20. Serafim RB, Soares M, Bozza FA, Lapa E Silva JR, Dal-Pizzol F, Paulino MC, et al. Outcomes of subsyndromal delirium in ICU: a systematic review and meta-analysis. Crit Care. 2017; 21(1):179. PMID: 28697802.21. Sanchez-Ramirez DC, Normand K, Zhaoyun Y, Torres-Castro R. Long-term impact of COVID-19: a systematic review of the literature and meta-analysis. Biomedicines. 2021; 9(8):900. PMID: 34440104.22. Ma Y, Deng J, Liu Q, Du M, Liu M, Liu J. Long-term consequences of COVID-19 at 6 months and above: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022; 19(11):6865. PMID: 35682448.23. Banerjee A, Pasea L, Harris S, Gonzalez-Izquierdo A, Torralbo A, Shallcross L, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020; 395(10238):1715–1725. PMID: 32405103.24. Garg M, Maralakunte M, Garg S, Dhooria S, Sehgal I, Bhalla AS, et al. The conundrum of ‘long-COVID-19: a narrative review. Int J Gen Med. 2021; 14:2491–2506. PMID: 34163217.25. Park EA, Kim MY. Postoperative delirium is associated with negative outcomes and long-term mortality in elderly Koreans: a retrospective observational study. Medicina (Kaunas). 2019; 55(10):618. PMID: 31547219.26. Sepandi M, Taghdir M, Alimohamadi Y, Afrashteh S, Hosamirudsari H. Factors associated with mortality in COVID-19 patients: a systematic review and meta-analysis. Iran J Public Health. 2020; 49(7):1211–1221. PMID: 33083287.27. Shao SC, Lai CC, Chen YH, Chen YC, Hung MJ, Liao SC. Prevalence, incidence and mortality of delirium in patients with COVID-19: a systematic review and meta-analysis. Age Ageing. 2021; 50(5):1445–1453. PMID: 33984129.28. Hoertel N, Sánchez-Rico M, Vernet R, Beeker N, Jannot AS, Neuraz A, et al. AP-HP / Universities / INSERM COVID-19 Research Collaboration and AP-HP COVID CDR Initiative. Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study. Mol Psychiatry. 2021; 26(9):5199–5212. PMID: 33536545.29. Nikooie R, Neufeld KJ, Oh ES, Wilson LM, Zhang A, Robinson KA, et al. Antipsychotics for treating delirium in hospitalized adults: a systematic review. Ann Intern Med. 2019; 171(7):485–495. PMID: 31476770.30. Sadlonova M, Duque L, Smith D, Madva EN, Amonoo HL, Vogelsang J, et al. Pharmacologic treatment of delirium symptoms: A systematic review. Gen Hosp Psychiatry. 2022; 79:60–75. PMID: 36375344.31. Aguilar-Navarro SG, Duarte-Flores JO, Granados-Valdéz MC, Suing-Ortega MJ, Mimenza-Alvarado AJ. Prevention, diagnosis, and treatment of delirium in older adults with COVID-19. Literature review. Salud Ment. 2021; 43(6):319–327.32. Ostuzzi G, Gastaldon C, Papola D, Fagiolini A, Dursun S, Taylor D, et al. Pharmacological treatment of hyperactive delirium in people with COVID-19: rethinking conventional approaches. Ther Adv Psychopharmacol. 2020; 10:2045125320942703. PMID: 32733668.33. Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing. 2011; 40(1):23–29. PMID: 21068014.34. Pandharipande P, Cotton BA, Shintani A, Thompson J, Pun BT, Morris JA Jr, et al. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. 2008; 65(1):34–41. PMID: 18580517.35. Park CM, Inouye SK, Marcantonio ER, Metzger E, Bateman BT, Lie JJ, et al. Perioperative gabapentin use and in-hospital adverse clinical events among older adults after major surgery. JAMA Intern Med. 2022; 182(11):1117–1127. PMID: 36121671.36. Sher Y, Miller Cramer AC, Ament A, Lolak S, Maldonado JR. Valproic acid for treatment of hyperactive or mixed delirium: rationale and literature review. Psychosomatics. 2015; 56(6):615–625. PMID: 26674479.37. Wang Y, Shen X. Postoperative delirium in the elderly: the potential neuropathogenesis. Aging Clin Exp Res. 2018; 30(11):1287–1295. PMID: 30051417.38. Grinchii D, Dremencov E. Mechanism of action of atypical antipsychotic drugs in mood disorders. Int J Mol Sci. 2020; 21(24):9532. PMID: 33333774.39. Teslyar P, Stock VM, Wilk CM, Camsari U, Ehrenreich MJ, Himelhoch S. Prophylaxis with antipsychotic medication reduces the risk of post-operative delirium in elderly patients: a meta-analysis. Psychosomatics. 2013; 54(2):124–131. PMID: 23380670.40. Chuen VL, Chan AC, Ma J, Alibhai SM, Chau V. Assessing the accuracy of International Classification of Diseases (ICD) coding for delirium. J Appl Gerontol. 2022; 41(5):1485–1490. PMID: 35176883.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Short Review of Delirium in Patients With COVID-19
- Osteonecrosis following Steroid Therapy in COVID-19 Patients: An Outlook on the Emerging Problem
- Acute Confusion as an Initial Presentation of SARS-CoV-2 Infection
- Cardiovascular Manifestations of COVID-19
- The Role of COVID-19 Vaccination for Patients With Atherosclerotic Cardiovascular Disease in the Upcoming Endemic Era