Brain Tumor Res Treat.
2024 Jul;12(3):200-203. 10.14791/btrt.2024.0025.
A Rare Case of Intracranial Growing Teratoma Syndrome in a Young Adult
- Affiliations
-
- 1Department of Neurosurgery, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Neurosurgery, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Rehabilitation Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Medical Oncology, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Hospital Pathology, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2558439
- DOI: http://doi.org/10.14791/btrt.2024.0025
Abstract
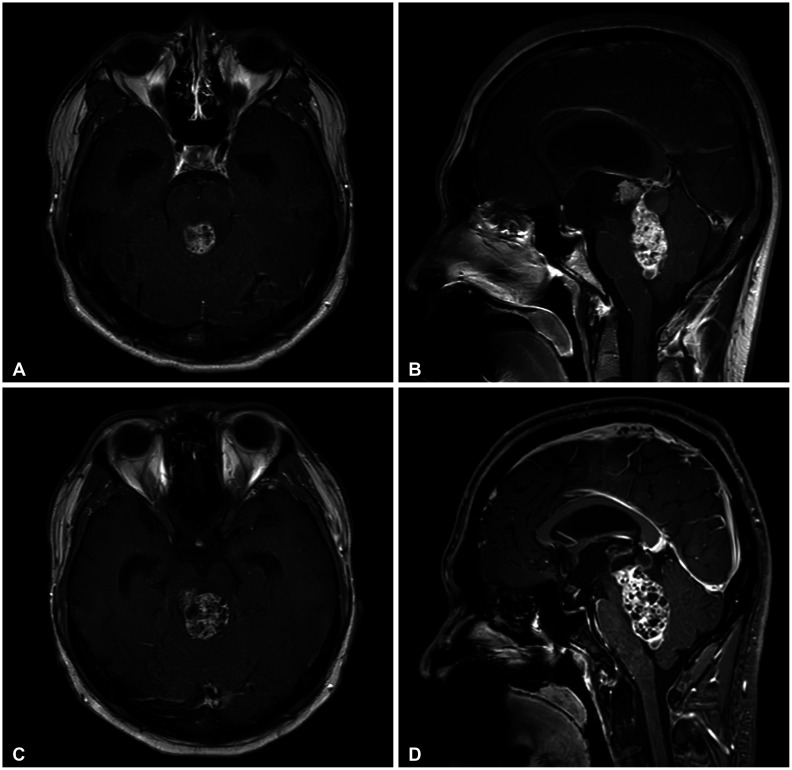
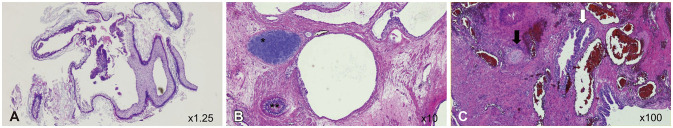
- Intracranial growing teratoma syndrome (iGTS) is a rare phenomenon in patients with non-germinomatous germ cell tumor (NGGCT) after chemotherapy or radiotherapy. It manifests as paradoxical growth of teratomatous components, with multiple cystic lesions on cranial imaging despite normalized tumor markers. This paper presents a 22-year-old male with iGTS, diagnosed one month after chemotherapy against NGGCT. Initially diagnosed with presumptive pineal NGGCT causing obstructive hydrocephalus, the patient underwent endoscopic third ventriculostomy and extraventricular drainage with tumor biopsy followed by two chemotherapy cycles. Despite normalization of tumor markers, follow-up MRI showed increased tumor size with honeycomb-like cystic patterns. The patient underwent suboccipital craniotomy for tumor removal via combined telovelar and infratentorial supracerebellar approaches. The final pathology confirmed mature teratoma. However, postoperative bleeding and left thalamic infarction occurred, resulting in severe neurological deficits. Despite challenges, the patient eventually regained the ability to follow simple commands. To understand iGTS pathophysiology, several hypotheses, including the differentiation of immature components and the uninhibited growth of mature components induced by chemotherapy or radiotherapy, were explored. Surgical intervention remains as an ideal treatment, while clinical trials investigate chemotherapy options. Frequent imaging followups are crucial for early detection in iGTS for NGGCT patients.
Figure
Reference
-
1. Yanagisawa S, Okamoto K, Yamaguchi S, Tamai Y, Fujitani M, Inoue M, et al. Intracranial growing teratoma syndrome observed at 44 months after initial treatment; a case presentation and literature review. Childs Nerv Syst. 2020; 36:865–868. PMID: 31853895.2. Khoo B, Ramakonar HH, Robbins P, Honeybul S. Intracranial monodermal teratoma presenting with growing teratoma syndrome. J Surg Case Rep. 2017; 2017:rjx038. PMID: 28560020.3. Kim CY, Choi JW, Lee JY, Kim SK, Wang KC, Park SH, et al. Intracranial growing teratoma syndrome: clinical characteristics and treatment strategy. J Neurooncol. 2011; 101:109–115. PMID: 20532955.4. Frappaz D, Dhall G, Murray MJ, Goldman S, Faure Conter C, Allen J, et al. EANO, SNO and Euracan consensus review on the current management and future development of intracranial germ cell tumors in adolescents and young adults. Neuro Oncol. 2022; 24:516–527. PMID: 34724065.5. Logothetis CJ, Samuels ML, Trindade A, Johnson DE. The growing teratoma syndrome. Cancer. 1982; 50:1629–1635. PMID: 6288220.6. Michaiel G, Strother D, Gottardo N, Bartels U, Coltin H, Hukin J, et al. Intracranial growing teratoma syndrome (iGTS): an international case series and review of the literature. J Neurooncol. 2020; 147:721–730. PMID: 32297094.7. Moiyadi A, Jalali R, Kane SV. Intracranial growing teratoma syndrome following radiotherapy--an unusually fulminant course. Acta Neurochir (Wien). 2010; 152:137–142. PMID: 19404574.8. Iwata H, Mori Y, Takagi H, Shirahashi K, Shinoda J, Shimokawa K, et al. Mediastinal growing teratoma syndrome after cisplatin-based chemotherapy and radiotherapy for intracranial germinoma. J Thorac Cardiovasc Surg. 2004; 127:291–293. PMID: 14752454.9. Tasaka K, Umeda K, Kamitori T, Ogata H, Mikami T, Saida S, et al. Intracranial growing teratoma syndrome with intraventricular lipid accumulation. J Pediatr Hematol Oncol. 2021; 43:e505–e507. PMID: 32769571.10. Oya S, Saito A, Okano A, Arai E, Yanai K, Matsui T. The pathogenesis of intracranial growing teratoma syndrome: proliferation of tumor cells or formation of multiple expanding cysts? Two case reports and review of the literature. Childs Nerv Syst. 2014; 30:1455–1461. PMID: 24633581.11. Kong DS, Nam DH, Lee JI, Park K, Kim JH, Shin HJ. Intracranial growing teratoma syndrome mimicking tumor relapse: a diagnostic dilemma. J Neurosurg Pediatr. 2009; 3:392–396. PMID: 19409018.12. Satake D, Natsumeda M, Satomi K, Tada M, Sato T, Okubo N, et al. Successful multimodal treatment of intracranial growing teratoma syndrome with malignant features. Curr Oncol. 2024; 31:1831–1838. PMID: 38668041.13. Han NY, Sung DJ, Park BJ, Kim MJ, Cho SB, Kim KA, et al. Imaging features of growing teratoma syndrome following a malignant ovarian germ cell tumor. J Comput Assist Tomogr. 2014; 38:551–557. PMID: 24681864.14. Kajiwara S, Nakamura H, Sakata K, Komaki S, Negoto T, Morioka M. Endoscopic aqueductal membrane fenestration was effective for intractable hydrocephalus after removal of a nongerminomatous germ cell tumor exhibiting growing teratoma syndrome: a case report. BMC Pediatr. 2022; 22:683. PMID: 36443673.15. Kanamori M, Kumabe T, Watanabe M, Chonan M, Saito R, Yamashita Y, et al. Indications for salvage surgery during treatment for intracranial germ cell tumors. J Neurooncol. 2018; 138:601–607. PMID: 29582270.16. Yagi K, Kageji T, Nagahiro S, Horiguchi H. Growing teratoma syndrome in a patient with a non-germinomatous germ cell tumor in the neurohypophysis--case report. Neurol Med Chir (Tokyo). 2004; 44:33–37. PMID: 14959935.17. Schultz KA, Petronio J, Bendel A, Patterson R, Vaughn DJ. PD0332991 (palbociclib) for treatment of pediatric intracranial growing teratoma syndrome. Pediatr Blood Cancer. 2015; 62:1072–1074. PMID: 25417786.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Recurrent Growing Teratoma Syndrome during Chemotherapy for Immature Teratoma of the Ovary
- Growing Teratoma Syndrome of the Pineal Gland Recognized Very Early during Chemotherapy in a Child with a Non-Germinomatous Germ-Cell Tumor
- A Case of Retroperitoneal Teratoma in an Adult
- Primary Intracranial Teratoma
- A Case of Testicular Teratoma