Brain Tumor Res Treat.
2024 Jul;12(3):172-180. 10.14791/btrt.2024.0026.
Supraorbital Approaches for Anterior Skull Base and Parasellar Lesions: Insights From a Single-Center Experience
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- KMID: 2558435
- DOI: http://doi.org/10.14791/btrt.2024.0026
Abstract
- Background
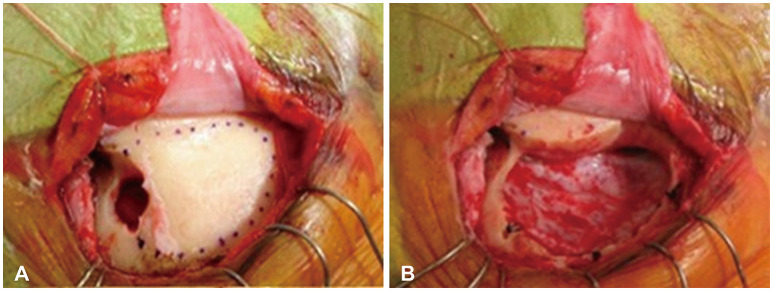
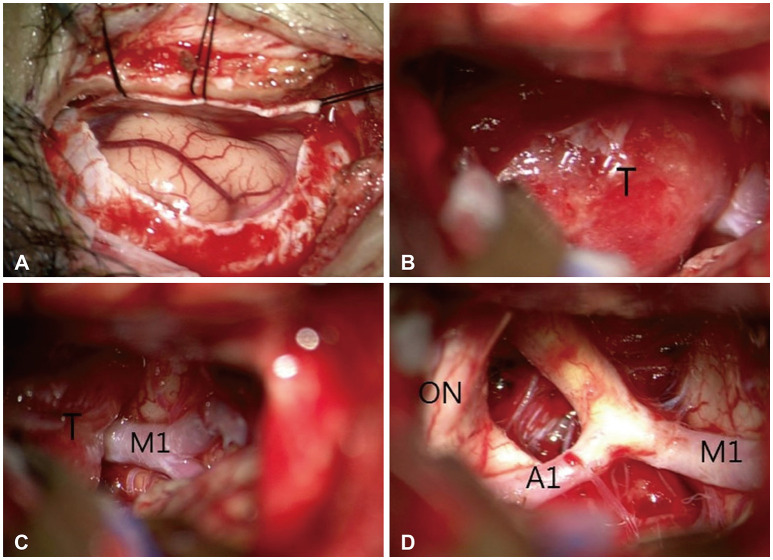
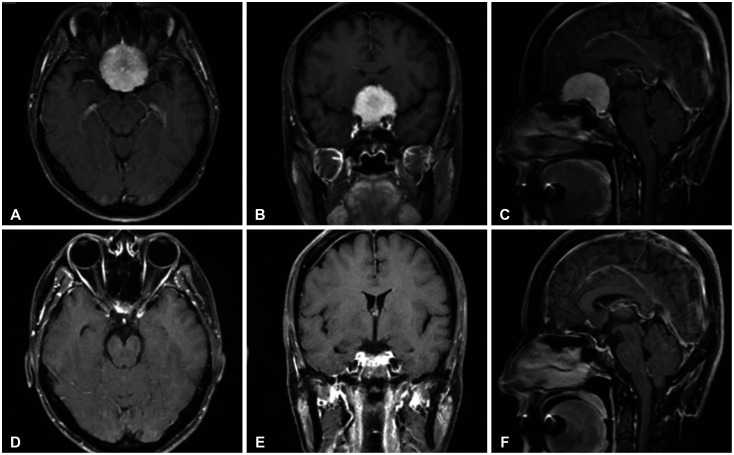
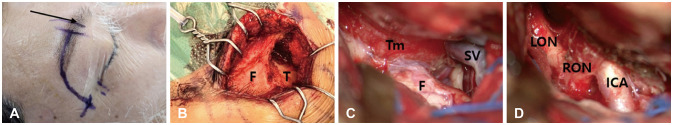
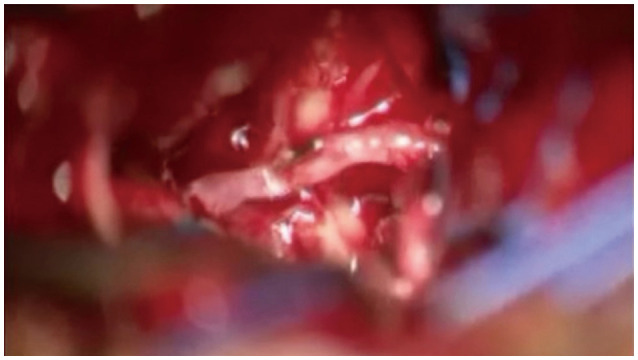
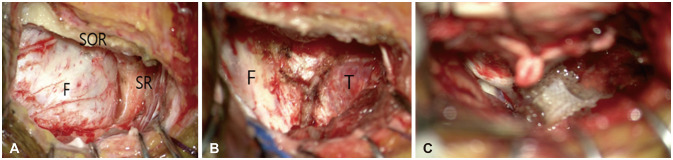
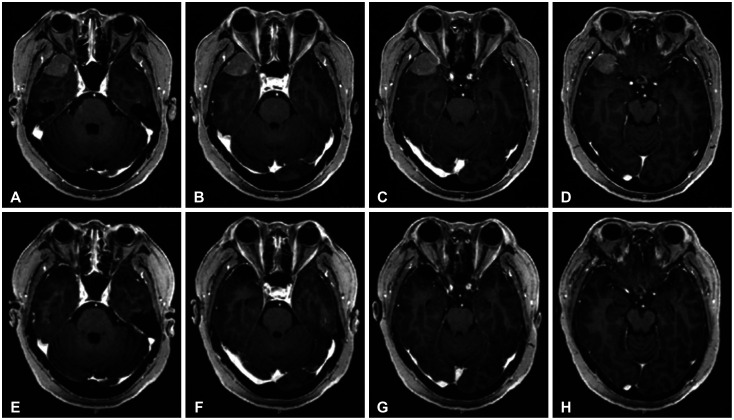
Modern neurosurgery has undergone significant evolution to include minimally inva-sive procedures, with the supraorbital approach (SOA) being a prime example. In this study, we aim to explore the surgical techniques and outcomes of this approach in the surgical treatment of frontal lobe, anterior skull base, and parasellar lesions.
Methods
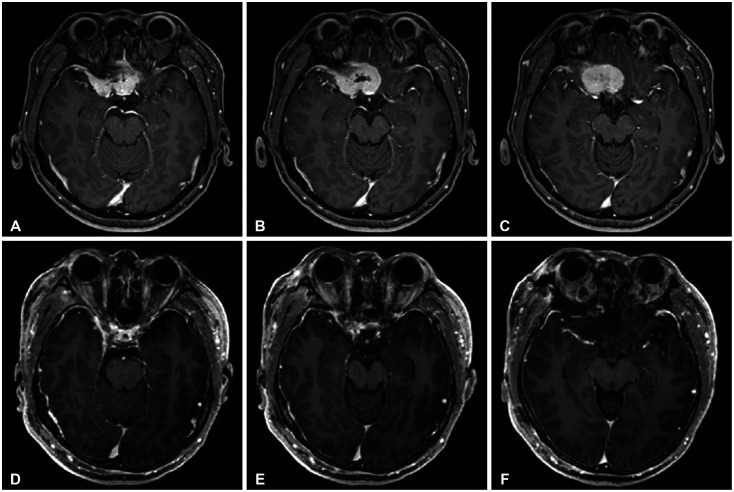
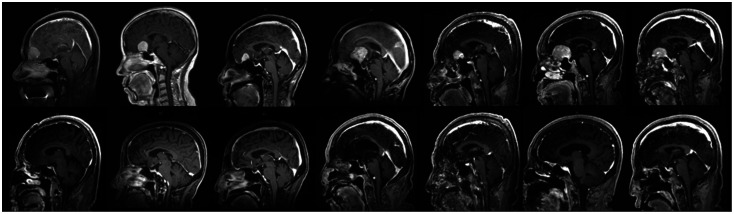
This study included 33 patients aged 36–83 years who underwent surgery using the SOA for lesions in the inferior frontal lobe, anterior skull base, and parasellar area between 2015 and 2024. There were 25 cases of meningioma, 2 cases of brain abscess, 2 cases of glioma, and one case each of craniopharyngioma, hemangioma, metastasis, and Rathke’s cleft cyst. The medical data and follow-up results were retrospectively analyzed.
Results
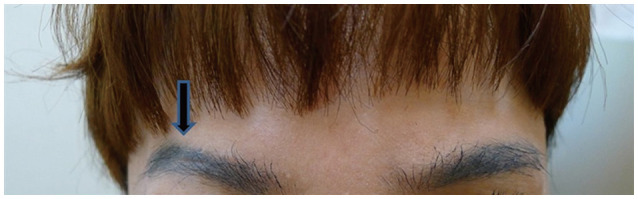
The mean size of lesion was 3.38±3.05 cm. The mean follow-up period was 48.8 months. Gross total resection was achieved in 25 patients (75.8%). There were no perioperative deaths, cases of cerebrospinal fluid rhinorrhea, or infections. Two cases of morbidity were reported as complications: one case of delayed intracerebral hemorrhage and one case of infarction due to vascular injury. All patients exhibited satisfactory cosmetic results.
Conclusion
In comparison to the conventional pterional approach, the SOA represents a safe and effective keyhole method for the removal of both extra-axial and intra-axial skull base tumors. This is particularly beneficial for lesions in the orbitofrontal region and parasellar area, as it allows for minimal disruption of normal brain parenchyma. Moreover, the SOA promotes a swift recovery and short hospital stay. Additionally, the SOA yields superior cosmetic results, including the prevention of temporalis muscle atrophy.
Figure
Reference
-
1. Adappa ND, Lee JY, Chiu AG, Palmer JN. Olfactory groove meningioma. Otolaryngol Clin North Am. 2011; 44:965–980. PMID: 21819883.2. Rychen J, Croci D, Roethlisberger M, Nossek E, Potts M, Radovanovic I, et al. Minimally invasive alternative approaches to pterional craniotomy: a systematic review of the literature. World Neurosurg. 2018; 113:163–179. PMID: 29452317.3. Gazzeri R, Nishiyama Y, Teo C. Endoscopic supraorbital eyebrow approach for the surgical treatment of extraaxialand intraaxial tumors. Neurosurg Focus. 2014; 37:E20.4. Robinow ZM, Peterson C, Waldau B, Shahlaie K. Supraorbital keyhole craniotomy via eyebrow incision: a systematic review and meta-analysis. World Neurosurg. 2022; 158:e509–e542. PMID: 34775096.5. Youngerman BE, Shtayer L, Gerges MM, Larsen AG, Tomasiewicz HC, Schwartz TH. Eyebrow supraorbital keyhole craniotomy for olfactory groove meningiomas with endoscope assistance: case series and systematic review of extent of resection, quantification of postoperative frontal lobe injury, anosmia, and recurrence. Acta Neurochir (Wien). 2021; 163:101–112. PMID: 32888076.6. Reisch R, Perneczky A, Filippi R. Surgical technique of the supraorbital key-hole craniotomy. Surg Neurol. 2003; 59:223–227. PMID: 12681560.7. Zumofen DW, Rychen J, Roethlisberger M, Taub E, Kalbermatten D, Nossek E, et al. A review of the literature on the transciliary supraorbital keyhole approach. World Neurosurg. 2017; 98:614–624. PMID: 27989977.8. Pepper JP, Hecht SL, Gebarski SS, Lin EM, Sullivan SE, Marentette LJ. Olfactory groove meningioma: discussion of clinical presentation and surgical outcomes following excision via the subcranial approach. Laryngoscope. 2011; 121:2282–2289. PMID: 21994142.9. Sade B, Lee JH. High incidence of optic canal involvement in tuberculum sellae meningiomas: rationale for aggressive skull base approach. Surg Neurol. 2009; 72:118–123. PMID: 19147207.10. Chen HC, Tzaan WC. Microsurgical supraorbital keyhole approach to the anterior cranial base. J Clin Neurosci. 2010; 17:1510–1514. PMID: 20817469.11. Tatarli N, Ceylan D, Şeker A, Solmaz B, Çavdar S, Kiliç T. The supraorbital keyhole approach. J Craniofac Surg. 2015; 26:1663–1667. PMID: 26114521.12. Eroglu U, Shah K, Bozkurt M, Kahilogullari G, Yakar F, Dogan İ, et al. Supraorbital keyhole approach: lessons learned from 106 operative cases. World Neurosurg. 2019; 124:e667–e674. PMID: 30659969.13. Iacoangeli M, Nocchi N, Nasi D, DI Rienzo A, Dobran M, Gladi M, et al. Minimally invasive supraorbital key-hole approach for the treatment of anterior cranial fossa meningiomas. Neurol Med Chir (Tokyo). 2016; 56:180–185. PMID: 26804334.14. Wiedemayer H, Sandalcioglu IE, Wiedemayer H, Stolke D. The supraorbital keyhole approach via an eyebrow incision for resection of tumors around the sella and the anterior skull base. Minim Invasive Neurosurg. 2004; 47:221–225. PMID: 15346318.15. Wilson DA, Duong H, Teo C, Kelly DF. The supraorbital endoscopic approach for tumors. World Neurosurg. 2014; 82:e243–e256. PMID: 23395805.16. Bander ED, Pandey A, Yan J, Giantini-Larsen AM, Schwartz A, Estin J, et al. Olfactory groove meningiomas: supraorbital keyhole versus orbitofrontal, frontotemporal, or bifrontal approaches. J Neurosurg. 2023; 140:1568–1575. PMID: 38064694.17. Cai M, Hou B, Luo L, Zhang B, Guo Y. Trans-eyebrow supraorbital keyhole approach to tuberculum sellae meningiomas: a series of 30 cases with long-term visual outcomes and recurrence rates. J Neurooncol. 2019; 142:545–555. PMID: 30796744.18. Singh H, Essayed WI, Jada A, Moussazadeh N, Dhandapani S, Rote S, et al. Contralateral supraorbital keyhole approach to medial optic nerve lesions: an anatomoclinical study. J Neurosurg. 2017; 126:940–944. PMID: 27257841.19. Troude L, Boucekine M, Baucher G, Farah K, Boissonneau S, Fuentes S, et al. Ipsilateral vs controlateral approach in tuberculum sellae meningiomas surgery: a retrospective comparative study. Neurosurg Rev. 2021; 44:3581–3591. PMID: 33890190.20. Beseoglu K, Lodes S, Stummer W, Steiger HJ, Hänggi D. The transorbital keyhole approach: early and long-term outcome analysis of approach-related morbidity and cosmetic results. J Neurosurg. 2011; 114:852–856. PMID: 21029037.