J Korean Med Sci.
2024 Jul;39(29):e214. 10.3346/jkms.2024.39.e214.
Healthcare Costs due to Dizziness/ Vertigo in Korea: Analyses Using the Public Data of Health Insurance Review & Assessment Service
- Affiliations
-
- 1Biomedical Research Institute, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Health Policy and Management, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Family Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 4Department of Family Medicine, College of Medicine, Seoul National University, Seoul, Korea
- 5Department of Neurology, College of Medicine, Seoul National University, Seoul, Korea
- 6Department of Neurology, Dizziness Center, Clinical Neuroscience Center, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2558249
- DOI: http://doi.org/10.3346/jkms.2024.39.e214
Abstract
- Background
Dizziness/vertigo is one of the most common symptoms for which people seek healthcare. However, the healthcare expenditure attributable to dizziness/vertigo in South Korea remains poorly understood. We investigated the healthcare costs due to six major disorders causing dizziness/vertigo using claims data.
Methods
The healthcare costs were evaluated using all the claims data submitted to the Health Insurance Review and Assessment Service from January 1 to December 31, 2022. The six major vestibular disorders included for analysis were benign paroxysmal positional vertigo (BPPV), psychogenic/persistent postural perceptual dizziness (PPPD), vascular vertigo/dizziness (VVD), vestibular migraine (VM), Meniere’s disease (MD), and vestibular neuritis (VN).
Results
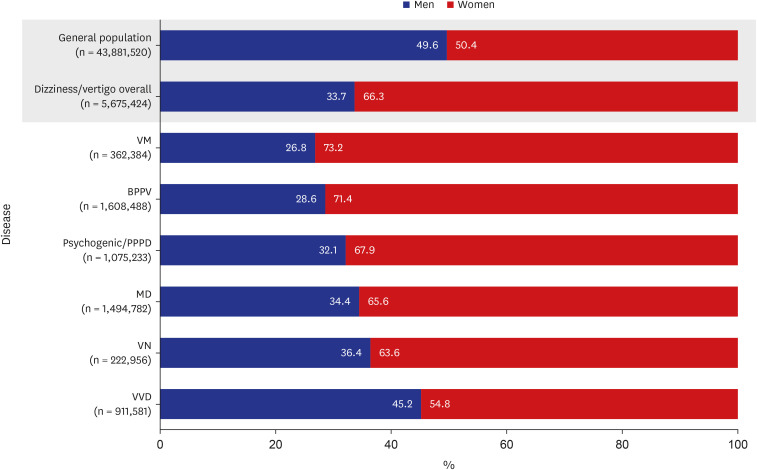
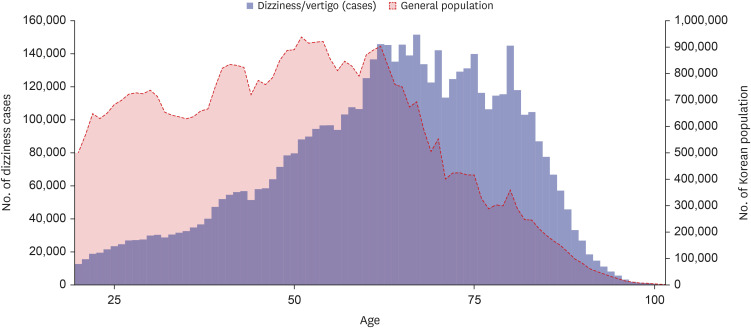
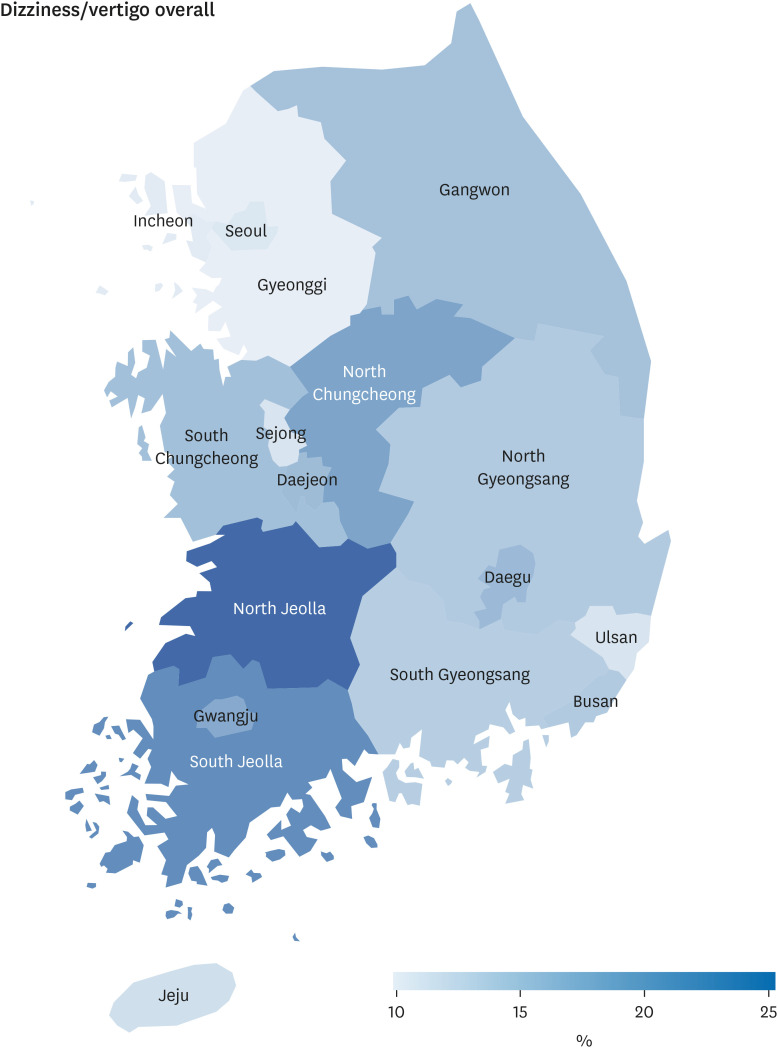
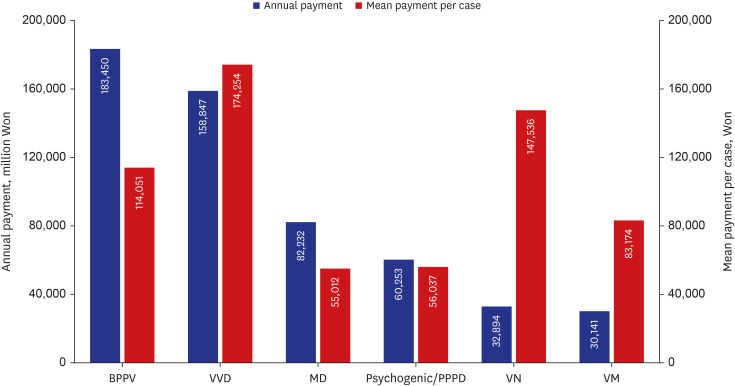
During the 1-year study period, 4.1% of adults aged 20 or older visited hospitals due to dizziness/vertigo in South Korea. Compared to the general population, the patients with dizziness/vertigo were more often elderly, female, and residents of small towns. The total healthcare cost for the six major vestibular disorders was ₩547.8 billion (approximately $406.5 million). BPPV incurred the highest annual healthcare cost (₩183.5 billion, 33.5%), followed by VVD (₩158.8 billion, 29.0%), MD (₩82.2 billion, 15.0%), psychogenic/PPPD (₩60.3 billion, 11.0%), VN (₩32.9 billion, 6.0%), and VM (₩30.1 billion, 5.5%). The mean healthcare cost per hospital visit due to dizziness/vertigo was ₩96,524 (95% confidence interval, ₩96,194–₩96,855), 30% higher than the average (₩73,948) of the overall healthcare cost per hospital visit over the same period.
Conclusion
Owing to higher healthcare costs for dizziness/vertigo and increased prevalence of dizziness/vertigo in the aged population, healthcare costs due to dizziness/vertigo will increase rapidly in South Korea. Thus, a guideline for cost-effective management of dizziness/ vertigo should be established to reduce the healthcare costs due to these common symptoms.
Figure
Reference
-
1. Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989; 86(3):262–266. PMID: 2919607.2. Mendel B, Bergenius J, Langius-Eklöf A. Dizziness: a common, troublesome symptom but often treatable. J Vestib Res. 2010; 20(5):391–398. PMID: 20826938.3. Bisdorff A, Bosser G, Gueguen R, Perrin P. The epidemiology of vertigo, dizziness, and unsteadiness and its links to co-morbidities. Front Neurol. 2013; 4:29. PMID: 23526567.4. Kim HJ, Lee JO, Choi JY, Kim JS. Etiologic distribution of dizziness and vertigo in a referral-based dizziness clinic in South Korea. J Neurol. 2020; 267(8):2252–2259. PMID: 32300888.5. Ruthberg JS, Rasendran C, Kocharyan A, Mowry SE, Otteson TD. The economic burden of vertigo and dizziness in the United States. J Vestib Res. 2021; 31(2):81–90. PMID: 33285661.6. Jeong SS, Simpson KN, Johnson JM, Rizk HG. Assessment of the cost burden of episodic recurrent vestibular vertigo in the US. JAMA Otolaryngol Head Neck Surg. 2022; 148(12):1103–1110. PMID: 36227614.7. Le A, Lelli DA, Van Katwyk S, Hogan D, Thavorn K, Tse D. Dizziness at a Canadian tertiary care hospital: a cost-of-illness study. J Otolaryngol Head Neck Surg. 2019; 48(1):5. PMID: 30651134.8. Wang X, Strobl R, Holle R, Seidl H, Peters A, Grill E. Vertigo and dizziness cause considerable more health care resource use and costs: results from the KORA FF4 study. J Neurol. 2019; 266(9):2120–2128. PMID: 31119449.9. United Nations (UN). World Population Prospects 2022. New York, NY, USA: UN;2022.10. Kyoung DS, Kim HS. Understanding and utilizing claim data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) database for research. J Lipid Atheroscler. 2022; 11(2):103–110. PMID: 35656154.11. Park JS, Lee CH. Clinical study using healthcare claims database. J Rheum Dis. 2021; 28(3):119–125. PMID: 37475998.12. Lee H, Lee JR, Jung H, Lee JY. Power of universal health coverage in the era of COVID-19: a nationwide observational study. Lancet Reg Health West Pac. 2021; 7:100088. PMID: 33521744.13. Tuty Kuswardhani RA, Henrina J, Pranata R, Anthonius Lim M, Lawrensia S, Suastika K. Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: a systematic review and meta-analysis. Diabetes Metab Syndr. 2020; 14(6):2103–2109. PMID: 33161221.14. Kim KH. Comparative study on three algorithms of the ICD-10 Charlson comorbidity index with myocardial infarction patients. J Prev Med Public Health. 2010; 43(1):42–49. PMID: 20185982.15. Charlson M. Charlson comorbidity index (CCI). Accessed June 7, 2024. https://www.mdcalc.com/calc/3917/charlson-comorbidity-index-cci .16. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004; 57(12):1288–1294. PMID: 15617955.17. Health Insurance Review & Assessment Service (HIRA). 2022 National Health Insurance Statistical Yearbook. Wonju, Korea: HIRA;2023.18. Yardley L, Owen N, Nazareth I, Luxon L. Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Pract. 1998; 48(429):1131–1135. PMID: 9667086.19. Neuhauser HK, Radtke A, von Brevern M, Lezius F, Feldmann M, Lempert T. Burden of dizziness and vertigo in the community. Arch Intern Med. 2008; 168(19):2118–2124. PMID: 18955641.20. Organisation for Economic Co-operation and Development (OECD). OECD Health Statistics 2023. Paris, France: OECD;2023.21. Park EK, Cho JW, Choi HG. Prevalence and risk factors of subjective dizziness in Korean. Res Vestib Sci. 2015; 14(2):46–49.22. Kim HY, Choi YJ, Kim DH, Lim HK, Kim GH, Choi MK, et al. The association of socioeconomic status and subjective dizziness in elderly Koreans: a cross sectional study from the Korean National Health and Nutrition Examination Survey 2010-2012. Korean J Fam Pract. 2017; 7(4):465–469.23. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383. PMID: 3558716.24. Kim SH. Differential diagnosis of the acute vestibular syndrome. Res Vestib Sci. 2021; 20(1):7–16.