J Rhinol.
2024 Jul;31(2):93-100. 10.18787/jr.2024.00017.
Comparative Analysis of the Clinical Manifestations of Sinonasal Natural Killer T-Cell Lymphoma and Diffuse Large B-Cell Lymphoma
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- KMID: 2558235
- DOI: http://doi.org/10.18787/jr.2024.00017
Abstract
- Background and Objectives
Natural killer T-cell lymphoma (NKTCL) and diffuse large B-cell lymphoma (DLBCL) are the two most prevalent subtypes of lymphoma in the sinonasal region. Accurately differentiating between sinonasal DLBCL and NKTCL is crucial for determining the appropriate treatment and prognosis. The present study compared the clinical characteristics of these two conditions.
Methods
We conducted a retrospective review of 173 patients diagnosed with sinonasal lymphoma at a single institute between 2004 and 2017. This review included only patients with DLBCL and NKTCL who had more than 6 months of follow-up records. We analyzed patient data encompassing clinical characteristics, pathologic findings, radiologic findings, treatment modalities, recurrence, and survival.
Results
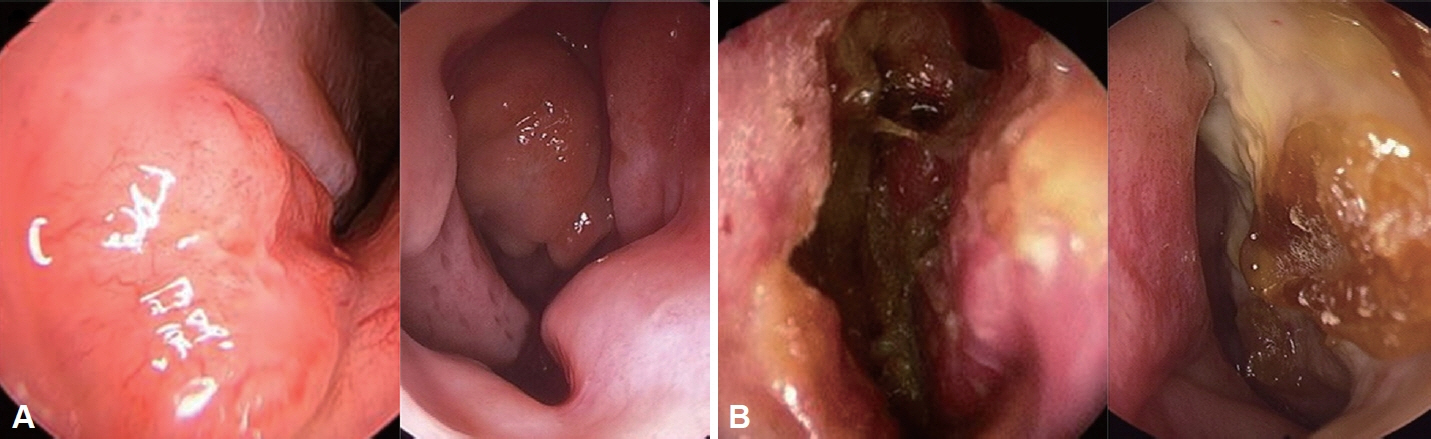
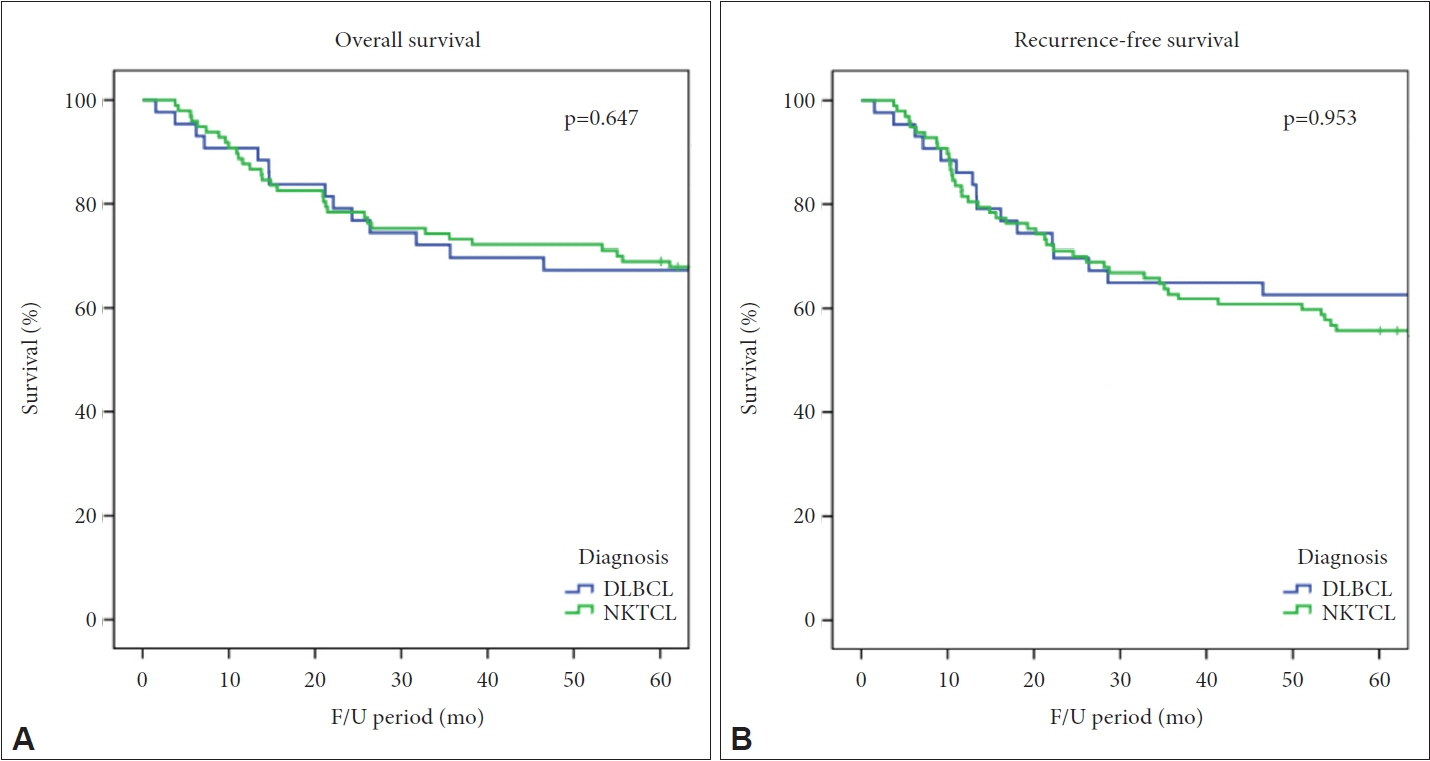
Among the patients analyzed, 117 patients were diagnosed with NKTCL and 45 with DLBCL. Endoscopic evaluation revealed a significantly higher incidence of crusting (p<0.001) and necrotic lesions (p=0.001) in patients with NKTCL, whereas polypoid masses were more commonly observed in patients with DLBCL (p<0.001). Computed tomography (CT) scans indicated no significant differences in bilaterality or bone destruction between the two groups. The DLBCL group exhibited a higher rate of concurrent lymph node or organ involvement than the NKTCL group (p<0.001). The 5-year overall survival rate was 67.4% for DLBCL and 69.1% for NKTCL, with no significant difference between the two.
Conclusion
Clinical differences exist between sinonasal DLBCL and NKTCL in terms of endoscopic and CT findings. These distinct characteristics can aid in distinguishing between the two types of sinonasal lymphoma during clinical diagnosis.
Figure
Reference
-
References
1. Hermans R, Horvath M, De Schrijver T, Lemahieu SF, Baert AL. Extranodal non-Hodgkin lymphoma of the head and neck. J Belge Radiol. 1994; 77(2):72–7.2. Kanumuri VV, Khan MN, Vazquez A, Govindaraj S, Baredes S, Eloy JA. Diffuse large B-cell lymphoma of the sinonasal tract: analysis of survival in 852 cases. Am J Otolaryngol. 2014; 35(2):154–8.
Article3. Vazquez A, Khan MN, Blake DM, Sanghvi S, Baredes S, Eloy JA. Extranodal natural killer/T-cell lymphoma: a population-based comparison of sinonasal and extranasal disease. Laryngoscope. 2014; 124(4):888–95.4. Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006; 107(1):265–76.
Article5. Smith A, Howell D, Patmore R, Jack A, Roman E. Incidence of haematological malignancy by sub-type: a report from the haematological malignancy research network. Br J Cancer. 2011; 105(11):1684–92.
Article6. Coha B, Vucinic I, Mahovne I, Vukovic-Arar Z. Extranodal lymphomas of head and neck with emphasis on NK/T-cell lymphoma, nasal type. J Craniomaxillofac Surg. 2014; 42(2):149–52.
Article7. Magrath I. The lymphoid neoplasms. 3rd ed. London: Hodder Arnold;2010.8. van Doesum JA, Niezink AGH, Huls GA, Beijert M, Diepstra A, van Meerten T. Extranodal natural killer/T-cell lymphoma, nasal type: diagnosis and treatment. Hemasphere. 2021; 5(2):e523.9. Chaganti S, Illidge T, Barrington S, Mckay P, Linton K, Cwynarski K, et al. Guidelines for the management of diffuse large B-cell lymphoma. Br J Haematol. 2016; 174(1):43–56.
Article10. Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC, et al. Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease: Cotswolds meeting. J Clin Oncol. 1989; 7(11):1630–6.
Article11. Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014; 32(27):3059–68.
Article12. Yamaguchi M, Suzuki R, Miyazaki K, Amaki J, Takizawa J, Sekiguchi N, et al. Improved prognosis of extranodal NK/T cell lymphoma, nasal type of nasal origin but not extranasal origin. Ann Hematol. 2019; 98(7):1647–55.
Article13. Chen Y, Wang X, Li L, Li W, Xian J. Differential diagnosis of sinonasal extranodal NK/T cell lymphoma and diffuse large B cell lymphoma on MRI. Neuroradiology. 2020; 62(9):1149–55.14. Swain SK, Acharya S. Extranodal non-Hodgkin’s lymphoma of the sinonasal tract: a review. BLDE Univ J Health Sci. 2021; 6(1):1–6.15. Ho FC, Srivastava G, Loke SL, Fu KH, Leung BP, Liang R, et al. Presence of Epstein-Barr virus DNA in nasal lymphomas of B and ‘T’ cell type. Hematol Oncol. 1990; 8(5):271–81.
Article16. Tao Q, Srivastava G, Loke SL, Liang RH, Liu YT, Ho FC. Epstein-Barr virus (EBV)-related lymphoproliferative disorder with subsequent EBV-negative T-cell lymphoma. Int J Cancer. 1994; 58(1):33–9.
Article17. Chim CS, Ma SY, Au WY, Choy C, Lie AK, Liang R, et al. Primary nasal natural killer cell lymphoma: long-term treatment outcome and relationship with the international prognostic index. Blood. 2004; 103(1):216–21.
Article18. Lee J, Suh C, Park YH, Ko YH, Bang SM, Lee JH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006; 24(4):612–8.19. Varelas AN, Eggerstedt M, Ganti A, Tajudeen BA. Epidemiologic, prognostic, and treatment factors in sinonasal diffuse large B -cell lymphoma. Laryngoscope. 2019; 129(6):1259–64.
Article20. Lombard M, Michel G, Rives P, Moreau A, Espitalier F, Malard O. Extranodal non-Hodgkin lymphoma of the sinonasal cavities: a 22-case report. Eur Ann Otorhinolaryngol Head Neck Dis. 2015; 132(5):271–4.
Article21. Cuadra-Garcia I, Proulx GM, Wu CL, Wang CC, Pilch BZ, Harris NL, et al. Sinonasal lymphoma: a clinicopathologic analysis of 58 cases from the Massachusetts General Hospital. Am J Surg Pathol. 1999; 23(11):1356–69.22. Schmitt C, Sako N, Bagot M, Huang Y, Gaulard P, Bensussan A. Extranodal NK/T-cell lymphoma: toward the identification of clinical molecular targets. J Biomed Biotechnol. 2011; 2011:790871.
Article23. Yan Z, Huang HQ, Wang XX, Gao Y, Zhang YJ, Bai B, et al. A TNM staging system for nasal NK/T-cell lymphoma. PLoS One. 2015; 10(6):e0130984.24. Dubal PM, Dutta R, Vazquez A, Patel TD, Baredes S, Eloy JA. A comparative population-based analysis of sinonasal diffuse large B-cell and extranodal NK/T-cell lymphomas. Laryngoscope. 2015; 125(5):1077–83.25. Kwong YL, Kim SJ, Tse E, Oh SY, Kwak JY, Eom HS, et al. Sequential chemotherapy/radiotherapy was comparable with concurrent chemoradiotherapy for stage I/II NK/T-cell lymphoma. Ann Oncol. 2018; 29(1):256–63.
Article26. Yamaguchi M, Kwong YL, Kim WS, Maeda Y, Hashimoto C, Suh C, et al. Phase II study of SMILE chemotherapy for newly diagnosed stage IV, relapsed, or refractory extranodal natural killer (NK)/T-cell lymphoma, nasal type: the NK-cell tumor study group study. J Clin Oncol. 2011; 29(33):4410–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Cutaneous T-cell/histiocyte-rich B-cell Lymphoma
- Metachronous extranodal natural killer/T-cell lymphoma of nasal type and primary testicular lymphoma
- Two Cases of Diffuse Large B-cell Lymphoma of Sinonasal Tract
- A Case of Natural Killer T-cell Lymphoma of the Tongue
- A Case of Diffuse Large B-Cell Lymphoma of Sinonasal Tract with Acute Visual Disturbance