J Rhinol.
2024 Jul;31(2):67-77. 10.18787/jr.2024.00022.
Epithelial-Mesenchymal Transition in Chronic Rhinosinusitis
- Affiliations
-
- 1Department of Medicine, Dankook University College of Medicine, Cheonan, Republic of Korea
- 2Department of Otorhinolaryngology, Dankook University College of Medicine, Cheonan, Republic of Korea
- 3Dankook Institute of Medicine & Optics, Dankook University, Cheonan, Republic of Korea
- KMID: 2558232
- DOI: http://doi.org/10.18787/jr.2024.00022
Abstract
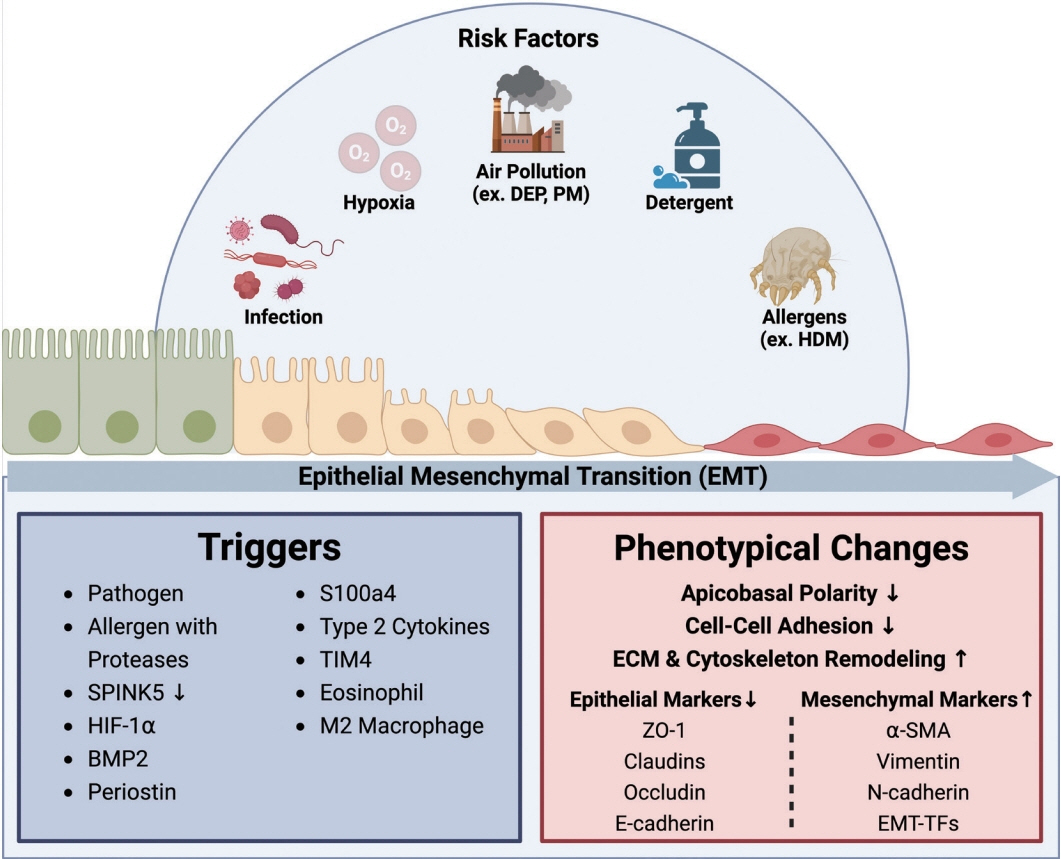
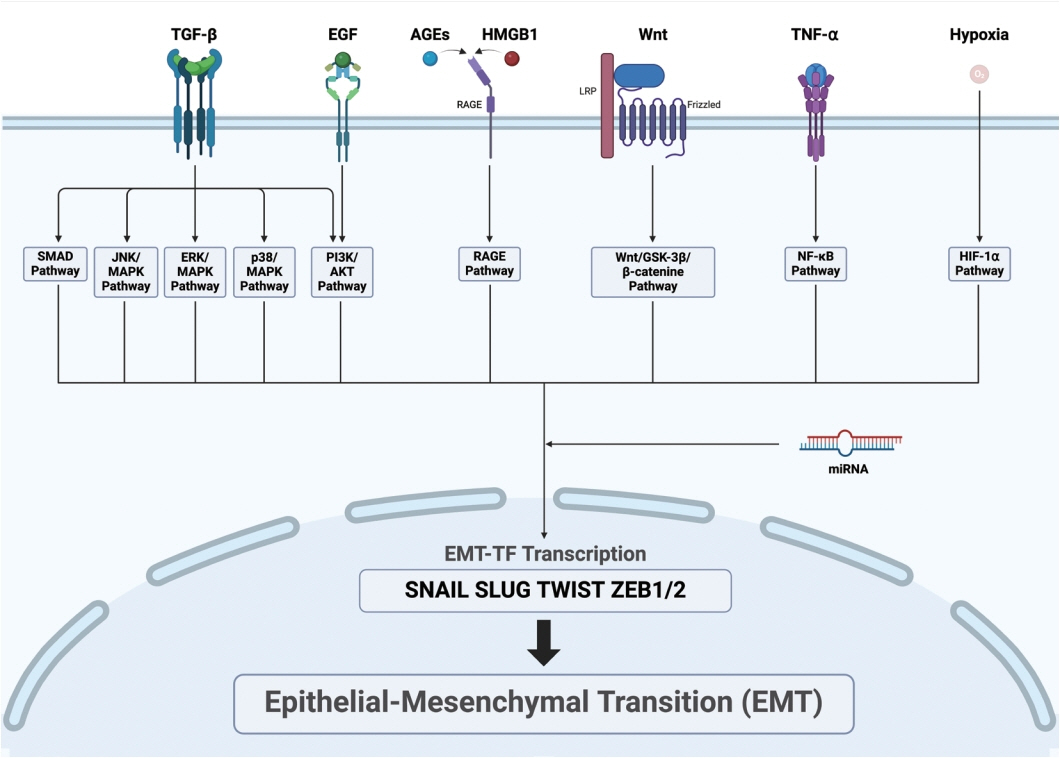
- Chronic rhinosinusitis (CRS) is characterized by prolonged inflammation of the nasal and paranasal sinus mucosa lasting over 12 weeks. CRS is divided into two main types based on the presence of nasal polyps: CRS without nasal polyps and CRS with nasal polyps. The condition is further classified into endotypes based on type 1, type 2, and type 3 inflammatory signatures, with differences in terms of disease severity, prognosis, and treatment response. Recent studies have emphasized the importance of the epithelial-mesenchymal transition (EMT) in CRS progression. In CRS, the EMT can be triggered by infections, allergens, hypoxia, and environmental pollutants. Specifically, EMT induction proceeds through the following mechanisms: viral and bacterial infections disrupt the epithelial barrier, house dust mites and other allergens activate the TGF-β and EGFR signaling pathways, hypoxia increases HIF-1α and other mesenchymal markers, and diesel exhaust particles and particulate matter cause oxidative stress. Maintaining the integrity of the epithelial barrier is essential for nasal mucosa homeostasis. In CRS, barrier damage activates repair processes that trigger the EMT, resulting in barrier dysfunction and tissue remodeling. Epithelial barrier dysfunction allows antigens and pathogens to penetrate, perpetuating inflammation and promoting the EMT. This disruption is a hallmark of CRS, emphasizing the importance of barrier integrity in the development of the disease. Key signaling pathways regulating the EMT in CRS include TGF-β, Wnt, HMGB1, AGE/ERK, TNF-α, and various miRNAs. These signaling pathways connect to various downstream pathways, such as the Smad2/3, GSK-3β/β-catenin, RAGE, and NF-κB pathways. This review focuses on the complex mechanisms of the EMT in CRS, emphasizing the role of epithelial barrier dysfunction and subsequent EMT processes in driving the disease’s development and progression. A deeper understanding of these EMT-driven mechanisms will help identify the potential therapeutic targets aimed at restoring epithelial integrity and reversing the EMT.
Figure
Reference
-
References
1. Bachert C, Marple B, Schlosser RJ, Hopkins C, Schleimer RP, Lambrecht BN, et al. Adult chronic rhinosinusitis. Nat Rev Dis Primers. 2020; 6(1):86.
Article2. Sedaghat AR, Kuan EC, Scadding GK. Epidemiology of chronic rhinosinusitis: prevalence and risk factors. J Allergy Clin Immunol Pract. 2022; 10(6):1395–403.
Article3. Yan B, Lan F, Li J, Wang C, Zhang L. The mucosal concept in chronic rhinosinusitis: focus on the epithelial barrier. J Allergy Clin Immunol. 2024; 153(5):1206–14.4. Schleimer RP. Immunopathogenesis of chronic rhinosinusitis and nasal polyposis. Annu Rev Pathol. 2017; 12:331–57.5. Yang J, Antin P, Berx G, Blanpain C, Brabletz T, Bronner M, et al. Guidelines and definitions for research on epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2020; 21(6):341–52.
Article6. Youssef KK, Nieto MA. Epithelial–mesenchymal transition in tissue repair and degeneration. Nat Rev Mol Cell Biol. 2024; Apr. 29. [Epub]. Available from: https://doi.org/10.1038/s41580-024-00733-z.7. Xia Y, Wang H, Yin J. The role of epithelial-mesenchymal transition in chronic rhinosinusitis. Int Arch Allergy Immunol. 2022; 183(10):1029–39.8. Hupin C, Gohy S, Bouzin C, Lecocq M, Polette M, Pilette C. Features of mesenchymal transition in the airway epithelium from chronic rhinosinusitis. Allergy. 2014; 69(11):1540–9.
Article9. Kim JY, Lim S, Lim HS, Kim YS, Eun KM, Khalmuratova R, et al. Bone morphogenetic protein-2 as a novel biomarker for refractory chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol. 2021; 148(2):461–72.e13.10. Gong N, Shi L, Bing X, Li H, Hu H, Zhang P, et al. S100A4/TCF complex transcription regulation drives epithelial-mesenchymal transition in chronic sinusitis through Wnt/GSK-3β/β-catenin signaling. Front Immunol. 2022; 13:835888.11. Hwang JH, Ryu JS, Yu JO, Choo YK, Kang J, Kim JY. Ganglioside GD3 regulates inflammation and epithelial-to-mesenchymal transition in human nasal epithelial cells. Int J Mol Sci. 2024; 25(7):4054.
Article12. Könnecke M, Burmeister M, Pries R, Böscke R, Bruchhage KL, Ungefroren H, et al. Epithelial–mesenchymal transition in chronic rhinosinusitis: differences revealed between epithelial cells from nasal polyps and inferior turbinates. Arch Immunol Ther Exp (Warsz). 2017; 65(2):157–73.
Article13. Wu Y, Sun K, Tu Y, Li P, Hao D, Yu P, et al. MiR-200a-3p regulates epithelial-mesenchymal transition and inflammation in chronic rhinosinusitis with nasal polyps by targeting ZEB1 via ERK/p38 pathway. Int Forum Allergy Rhinol. 2024; 14(1):41–56.
Article14. Lee M, Lim S, Kim YS, Khalmuratova R, Shin SH, Kim I, et al. DEPinduced ZEB2 promotes nasal polyp formation via epithelial-to-mesenchymal transition. J Allergy Clin Immunol. 2022; 149(1):340–57.15. Rowan NR, Lee S, Sahu N, Kanaan A, Cox S, Phillips CD, et al. The role of viruses in the clinical presentation of chronic rhinosinusitis. Am J Rhinol Allergy. 2015; 29(6):e197–200.
Article16. Minor DM, Proud D. Role of human rhinovirus in triggering human airway epithelial-mesenchymal transition. Respir Res. 2017; 18(1):110.
Article17. Sajjan U, Wang Q, Zhao Y, Gruenert DC, Hershenson MB. Rhinovirus disrupts the barrier function of polarized airway epithelial cells. Am J Respir Crit Care Med. 2008; 178(12):1271–81.
Article18. Xiang Z, Liang Z, Yanfeng H, Leitao K. Persistence of RSV promotes proliferation and epithelial-mesenchymal transition of bronchial epithelial cells through Nodal signaling. J Med Microbiol. 2017; 66(10):1499–505.
Article19. Borthwick LA, Sunny SS, Oliphant V, Perry J, Brodlie M, Johnson GE, et al. Pseudomonas aeruginosa accentuates epithelial-to-mesenchymal transition in the airway. Eur Respir J. 2011; 37(5):1237–47.20. Gupta I, Pedersen S, Vranic S, Al Moustafa AE. Implications of gut microbiota in epithelial-mesenchymal transition and cancer progression: a concise review. Cancers (Basel). 2022; 14(12):2964.
Article21. Ziesemer S, Eiffler I, Schönberg A, Müller C, Hochgräfe F, Beule AG, et al. Staphylococcus aureus α-toxin induces actin filament remodeling in human airway epithelial model cells. Am J Respir Cell Mol Biol. 2018; 58(4):482–91.
Article22. Meng J, Zhou P, Liu Y, Liu F, Yi X, Liu S, et al. The development of nasal polyp disease involves early nasal mucosal inflammation and remodelling. PLoS One. 2013; 8(12):e82373.
Article23. Patou J, Gevaert P, Van Zele T, Holtappels G, van Cauwenberge P, Bachert C. Staphylococcus aureus enterotoxin B, protein A, and lipoteichoic acid stimulations in nasal polyps. J Allergy Clin Immunol. 2008; 121(1):110–5.
Article24. Johnson JR, Roos A, Berg T, Nord M, Fuxe J. Chronic respiratory aero allergen exposure in mice induces epithelial-mesenchymal transition in the large airways. PLoS One. 2011; 6(1):e16175.25. Heijink IH, Postma DS, Noordhoek JA, Broekema M, Kapus A. House dust mite-promoted epithelial-to-mesenchymal transition in human bronchial epithelium. Am J Respir Cell Mol Biol. 2010; 42(1):69–79.
Article26. Sun Z, Ji N, Ma Q, Zhu R, Chen Z, Wang Z, et al. Epithelial-mesenchymal transition in asthma airway remodeling is regulated by the IL-33/CD146 axis. Front Immunol. 2020; 11:1598.
Article27. Zou Y, Song W, Zhou L, Mao Y, Hong W. House dust mite induces Sonic hedgehog signaling that mediates epithelial‑mesenchymal transition in human bronchial epithelial cells. Mol Med Rep. 2019; 20(5):4674–82.
Article28. Wan H, Winton HL, Soeller C, Tovey ER, Gruenert DC, Thompson PJ, et al. Der p 1 facilitates transepithelial allergen delivery by disruption of tight junctions. J Clin Invest. 1999; 104(1):123–33.
Article29. Richer SL, Truong-Tran AQ, Conley DB, Carter R, Vermylen D, Grammer LC, et al. Epithelial genes in chronic rhinosinusitis with and without nasal polyps. Am J Rhinol. 2008; 22(3):228–34.30. Tieu DD, Kern RC, Schleimer RP. Alterations in epithelial barrier function and host defense responses in chronic rhinosinusitis. J Allergy Clin Immunol. 2009; 124(1):37–42.
Article31. Shin HW, Cho K, Kim DW, Han DH, Khalmuratova R, Kim SW, et al. Hypoxia-inducible factor 1 mediates nasal polypogenesis by inducing epithelial-to-mesenchymal transition. Am J Respir Crit Care Med. 2012; 185(9):944–54.
Article32. Kao SH, Wu KJ, Lee WH. Hypoxia, epithelial-mesenchymal transition, and TET-mediated epigenetic changes. J Clin Med. 2016; 5(2):24.
Article33. Lim JH, Lee YM, Chun YS, Chen J, Kim JE, Park JW. Sirtuin 1 modulates cellular responses to hypoxia by deacetylating hypoxia-inducible factor 1α. Mol Cell. 2010; 38(6):864–78.
Article34. Lee M, Kim DW, Yoon H, So D, Khalmuratova R, Rhee CS, et al. Sirtuin 1 attenuates nasal polypogenesis by suppressing epithelial-tomesenchymal transition. J Allergy Clin Immunol. 2016; 137(1):87–98.E7.35. Yang N, Cheng H, Mo Q, Zhou X, Xie M. MiR‑155‑5p downregulation inhibits epithelial‑to‑mesenchymal transition by targeting SIRT1 in human nasal epithelial cells. Mol Med Rep. 2020; 22(5):3695–704.
Article36. Chen SY, Liu PQ, Qin DX, Lv H, Zhou HQ, Xu Y. E3 ubiquitin ligase NEDD4L inhibits epithelial-mesenchymal transition by suppressing the β-catenin/HIF-1α positive feedback loop in chronic rhinosinusitis with nasal polyps. Acta Pharmacol Sin. 2024; 45(4):831–43.
Article37. Zhao R, Guo Z, Zhang R, Deng C, Xu J, Dong W, et al. Nasal epithelial barrier disruption by particulate matter ≤2.5 μm via tight junction protein degradation. J Appl Toxicol. 2018; 38(5):678–87.
Article38. Xian M, Ma S, Wang K, Lou H, Wang Y, Zhang L, et al. Particulate matter 2.5 causes deficiency in barrier integrity in human nasal epithelial cells. Allergy Asthma Immunol Res. 2020; 12(1):56–71.
Article39. Lee KI, Han Y, Ryu JS, In SM, Kim JY, Park JS, et al. Tobacco smoking could accentuate epithelial-mesenchymal transition and Th2-type response in patients with chronic rhinosinusitis with nasal polyps. Immune Netw. 2022; 22(4):e35.
Article40. Zuo H, Trombetta-Lima M, Heijink IH, van der Veen CHTJ, Hesse L, Faber KN, et al. A-kinase anchoring proteins diminish TGF-β1/cigarette smoke-induced epithelial-to-mesenchymal transition. Cells. 2020; 9(2):356.
Article41. Celebi Sözener Z, Cevhertas L, Nadeau K, Akdis M, Akdis CA. Environmental factors in epithelial barrier dysfunction. J Allergy Clin Immunol. 2020; 145(6):1517–28.
Article42. Wang M, Tan G, Eljaszewicz A, Meng Y, Wawrzyniak P, Acharya S, et al. Laundry detergents and detergent residue after rinsing directly disrupt tight junction barrier integrity in human bronchial epithelial cells. J Allergy Clin Immunol. 2019; 143(5):1892–903.
Article43. Vaezi GH, Aliabadi F, Shiravi AB, Pourkazem M, Toosi F. Histopathology of inhalation of industrial bleach and detergent mixture on epithelial layer of trachea in mice. J Chem Health Risks. 2011; 1(1):29–33.44. Wang W, Xu Y, Wang L, Zhu Z, Aodeng S, Chen H, et al. Single-cell profiling identifies mechanisms of inflammatory heterogeneity in chronic rhinosinusitis. Nat Immunol. 2022; 23(10):1484–94.45. Hewitt RJ, Lloyd CM. Regulation of immune responses by the airway epithelial cell landscape. Nat Rev Immunol. 2021; 21(6):347–62.
Article46. Grainge CL, Davies DE. Epithelial injury and repair in airways diseases. Chest. 2013; 144(6):1906–12.
Article47. Gohy S, Hupin C, Ladjemi MZ, Hox V, Pilette C. Key role of the epithelium in chronic upper airways diseases. Clin Exp Allergy. 2020; 50(2):135–46.
Article48. Wang M, Sun Y, Li C, Qu J, Zhou B. Eosinophils correlate with epithelial-mesenchymal transition in chronic rhinosinusitis with nasal polyps. ORL J Otorhinolaryngol Relat Spec. 2022; 84(1):70–80.
Article49. Bachert C, Han JK, Desrosiers M, Hellings PW, Amin N, Lee SE, et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet. 2019; 394(10209):1638–50.50. Kato A. Immunopathology of chronic rhinosinusitis. Allergol Int. 2015; 64(2):121–30.51. Chen J, Chen S, Gong G, Yang F, Chen J, Wang Y. Inhibition of IL-4/STAT6/IRF4 signaling reduces the epithelial-mesenchymal transition in eosinophilic chronic rhinosinusitis with nasal polyps. Int Immunopharmacol. 2023; 121:110554.
Article52. Qin D, Liu P, Zhou H, Jin J, Gong W, Liu K, et al. TIM-4 in macrophages contributes to nasal polyp formation through the TGF-β1-mediated epithelial to mesenchymal transition in nasal epithelial cells. Front Immunol. 2022; 13:941608.53. Flood-Page P, Menzies-Gow A, Phipps S, Ying S, Wangoo A, Ludwig MS, et al. Anti-IL-5 treatment reduces deposition of ECM proteins in the bronchial subepithelial basement membrane of mild atopic asthmatics. J Clin Invest. 2003; 112(7):1029–36.54. Chiarella E, Lombardo N, Lobello N, Aloisio A, Aragona T, Pelaia C, et al. Nasal polyposis: insights in epithelial-mesenchymal transition and differentiation of polyp mesenchymal stem cells. Int J Mol Sci. 2020; 21(18):6878.55. Lee K, Tai J, Lee SH, Kim TH. Advances in the knowledge of the underlying airway remodeling mechanisms in chronic rhinosinusitis based on the endotypes: a review. Int J Mol Sci. 2021; 22(2):910.56. Van Bruaene N, Derycke L, Perez-Novo CA, Gevaert P, Holtappels G, De Ruyck N, et al. TGF-β signaling and collagen deposition in chronic rhinosinusitis. J Allergy Clin Immunol. 2009; 124(2):253–9.E2.
Article57. Dobzanski A, Khalil SM, Lane AP. Nasal polyp fibroblasts modulate epithelial characteristics via Wnt signaling. Int Forum Allergy Rhinol. 2018; 8(12):1412–20.58. Wang Y, Li Z, Lu J. Single-cell RNA sequencing reveals the epithelial cell, fibroblast, and key gene alterations in chronic rhinosinusitis with nasal polyps. Sci Rep. 2024; 14(1):2270.59. Li YC, An YS, Wang T, Zang HR. Analysis of transforming growth factor β signaling in chronic rhinosinusitis. Chin Med J (Engl). 2013; 126(17):3340–3.
Article60. Wang T, Zang HR, Li YC. [The role of Smad signaling pathway in the repair of mucosal epithelium in chronic sinusitis with nasal polyps and without nasal polyps]. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2019; 33(1):9–13. Chinese.61. Gao R, Chen Y, Liu H, Ye M, Chu L, Wang T. CD109 identified in circulating proteomics mitigates postoperative recurrence in chronic rhinosinusitis with nasal polyps by suppressing TGF-β1-induced epithelial-mesenchymal transition. Int Immunopharmacol. 2024; 130:111793.
Article62. Zhong Y, Li Y, Zhang H. Silencing TBX1 exerts suppressive effects on epithelial–mesenchymal transition and inflammation of chronic rhinosinusitis through inhibition of the TGFβ-Smad2/3 signaling pathway in mice. Am J Rhinol Allergy. 2020; 34(1):16–25.63. Fan Q, Jian Y. MiR-203a-3p regulates TGF-β1-induced epithelial-mesenchymal transition (EMT) in asthma by regulating Smad3 pathway through SIX1. Biosci Rep. 2020; 40(2):BSR20192645.64. Park JH, Shin JM, Yang HW, Park IH. DNMTs are involved in TGF-β1-induced epithelial-mesenchymal transitions in airway epithelial cells. Int J Mol Sci. 2022; 23(6):3003.65. Lamouille S, Derynck R. Cell size and invasion in TGF-beta-induced epithelial to mesenchymal transition is regulated by activation of the mTOR pathway. J Cell Biol. 2007; 178(3):437–51.66. Yang HW, Lee SA, Shin JM, Park IH, Lee HM. Glucocorticoids ameliorate TGF-β1-mediated epithelial-to-mesenchymal transition of airway epithelium through MAPK and Snail/Slug signaling pathways. Sci Rep. 2017; 7(1):3486.
Article67. Shin JM, Park JH, Yang HW, Moon JW, Lee HM, Park IH. MiR-29b regulates TGF-β1-induced epithelial-mesenchymal transition by inhibiting heat shock protein 47 expression in airway epithelial cells. Int J Mol Sci. 2021; 22(21):11535.68. Jiang W, Zhou C, Ma C, Cao Y, Hu G, Li H. TGF-β1 induces epithelial-to-mesenchymal transition in chronic rhinosinusitis with nasal polyps through microRNA-182. Asian Pac J Allergy Immunol. 2024; 42(1):61–73.69. Park IH, Kang JH, Shin JM, Lee HM. Trichostatin A inhibits epithelial mesenchymal transition induced by TGF-β1 in airway epithelium. PLoS One. 2016; 11(8):e0162058.70. Lee HM, Kang JH, Shin JM, Lee SA, Park IH. Chemical chaperone of endoplasmic reticulum stress inhibits epithelial-mesenchymal transition induced by TGF-β1 in airway epithelium via the c-Src pathway. Mediators Inflamm. 2017; 2017:8123281.71. Dzaman K, Szczepanski MJ, Molinska-Glura M, Krzeski A, Zagor M. Expression of the receptor for advanced glycation end products, a target for high mobility group box 1 protein, and its role in chronic recalcitrant rhinosinusitis with nasal polyps. Arch Immunol Ther Exp (Warsz). 2015; 63(3):223–30.
Article72. Min HJ, Choe JW, Kim KS, Yoon JH, Kim CH. High-mobility group box 1 protein induces epithelialmesenchymal transition in upper airway epithelial cells. Rhinology. 2020; 58(5):495–505.73. Liu P, Qin D, Deng Z, Tong X, Liu K, Fan W, et al. TET2 deficiency exacerbates nasal polypogenesis by inducing epithelial-to-mesenchymal transition. Allergy. 2022; 77(11):3452–5.74. Yang P, Chen S, Zhong G, Kong W, Wang Y. Agonist of PPAR-γ reduced epithelial-mesenchymal transition in eosinophilic chronic rhinosinusitis with nasal polyps via inhibition of high mobility group box1. Int J Med Sci. 2019; 16(12):1631–41.75. Hao W, Zhu Y, Guo Y, Wang H. MiR-1287-5p upregulation inhibits the EMT and pro-inflammatory cytokines in LPS-induced human nasal epithelial cells (HNECs). Transpl Immunol. 2021; 68:101429.76. Bae JS, Ryu G, Kim JH, Kim EH, Rhee YH, Chung YJ, et al. Effects of Wnt signaling on epithelial to mesenchymal transition in chronic rhinosinusitis with nasal polyp. Thorax. 2020; 75(11):982–93.
Article77. Vetuschi A, Pompili S, Di Marco GP, Calvaruso F, Iacomino E, Angelosante L, et al. Can the AGE/RAGE/ERK signalling pathway and the epithelial-to-mesenchymal transition interact in the pathogenesis of chronic rhinosinusitis with nasal polyps? Eur J Histochem. 2020; 64(1):3079.78. Chen YS, Wang XJ, Feng W, Hua KQ. Advanced glycation end products decrease collagen I levels in fibroblasts from the vaginal wall of patients with POP via the RAGE, MAPK and NF-κB pathways. Int J Mol Med. 2017; 40(4):987–98.79. Lee M, Kim DW, Khalmuratova R, Shin SH, Kim YM, Han DH, et al. The IFN-γ-p38, ERK kinase axis exacerbates neutrophilic chronic rhinosinusitis by inducing the epithelial-to-mesenchymal transition. Mucosal Immunol. 2019; 12(3):601–11.80. Câmara J, Jarai G. Epithelial-mesenchymal transition in primary human bronchial epithelial cells is Smad-dependent and enhanced by fibronectin and TNF-α. Fibrogenesis Tissue Repair. 2010; 3(1):2.81. Li CW, Xia W, Huo L, Lim SO, Wu Y, Hsu JL, et al. Epithelial-mesenchymal transition induced by TNF-α requires NF-κB-mediated transcriptional upregulation of Twist1. Cancer Res. 2012; 72(5):1290–300.
Article82. Lee SN, Lee DH, Sohn MH, Yoon JH. Overexpressed proprotein convertase 1/3 induces an epithelial-mesenchymal transition in airway epithelium. Eur Respir J. 2013; 42(5):1379–90.83. Zhang T, Zhou Y, You B, You Y, Yan Y, Zhang J, et al. MiR-30a-5p inhibits epithelial-to-mesenchymal transition by targeting CDK6 in nasal polyps. Am J Rhinol Allergy. 2021; 35(2):152–63.84. Wang T, Zhou Q, Shang Y. MiRNA-451a inhibits airway remodeling by targeting Cadherin 11 in an allergic asthma model of neonatal mice. Int Immunopharmacol. 2020; 83:106440.
Article85. Gu X, Yao X, Liu D. Up-regulation of microRNA-335-5p reduces inflammation via negative regulation of the TPX2-mediated AKT/GSK3β signaling pathway in a chronic rhinosinusitis mouse model. Cell Signal. 2020; 70:109596.
Article86. Cheng J, Chen J, Zhao Y, Yang J, Xue K, Wang Z. MicroRNA-761 suppresses remodeling of nasal mucosa and epithelial-mesenchymal transition in mice with chronic rhinosinusitis through LCN2. Stem Cell Res Ther. 2020; 11(1):151.
Article87. Callejas-Díaz B, Fernandez G, Fuentes M, Martínez-Antón A, Alobid I, Roca-Ferrer J, et al. Integrated mRNA and microRNA transcriptome profiling during differentiation of human nasal polyp epithelium reveals an altered ciliogenesis. Allergy. 2020; 75(10):2548–61.88. Zhang XH, Zhang YN, Li HB, Hu CY, Wang N, Cao PP, et al. Overexpression of miR-125b, a novel regulator of innate immunity, in eosinophilic chronic rhinosinusitis with nasal polyps. Am J Respir Crit Care Med. 2012; 185(2):140–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Targeting epithelial-mesenchymal transition pathway in hepatocellular carcinoma
- Consideration of EphA2 in relation to epithelial-mesenchymal transition in uterine endometrial cancer
- Role of Gastric Stem Cells in Gastric Carcinogenesis by Chronic Helicobacter pylori Infection
- Aberrant Expression of Epithelial-Mesenchymal Transition Markers in Early Gastric Cancer: Clinical Application
- Cell Lineage, Self-Renewal, and Epithelial-to-Mesenchymal Transition during Secondary Neurulation