Intest Res.
2024 Jul;22(3):310-318. 10.5217/ir.2023.00174.
Adequacy of sigmoidoscopy as compared to colonoscopy for assessment of disease activity in patients of ulcerative colitis: a prospective study
- Affiliations
-
- 1Department of Gastroenterology, Topiwala National Medical College and BYL Nair Charitable Hospital, Mumbai, India
- 2Department of Pathology, Topiwala National Medical College and BYL Nair Charitable Hospital, Mumbai, India
- KMID: 2558191
- DOI: http://doi.org/10.5217/ir.2023.00174
Abstract
- Background/Aims
Patients of ulcerative colitis (UC) on follow-up are routinely evaluated by sigmoidoscopy. There is no prospective literature to support this practice. We assessed agreement between sigmoidoscopy and colonoscopy prospectively in patients with disease extent beyond the sigmoid colon.
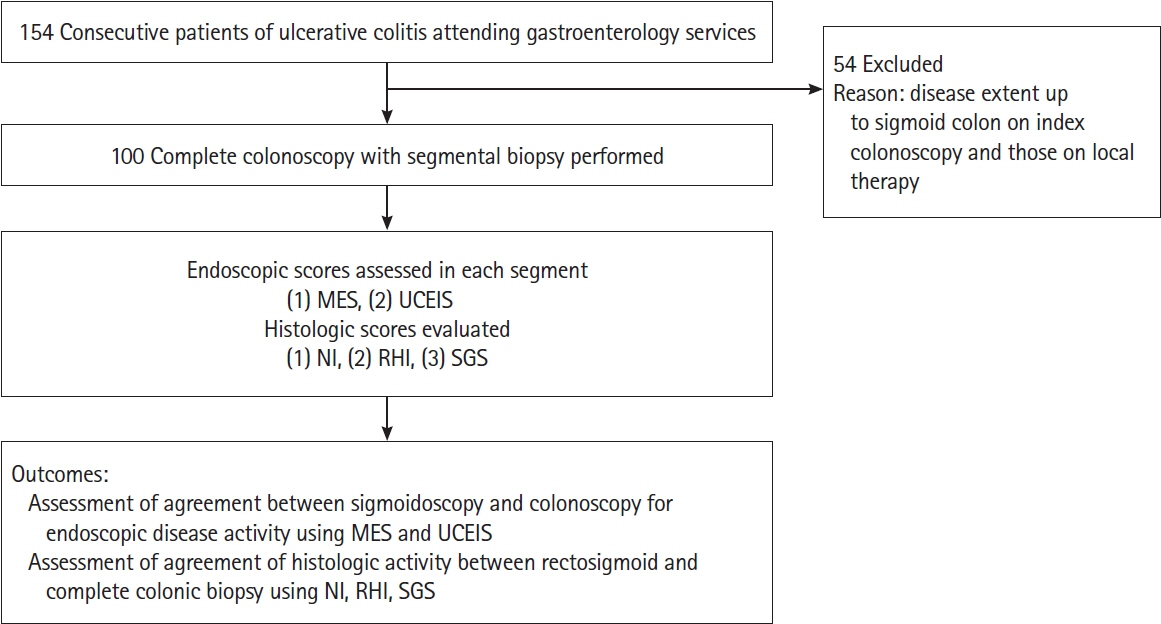
Methods
We conducted a prospective observational study at a tertiary care institute for agreement between sigmoidoscopy and colonoscopy. We assessed endoscopic activity using the Mayo Endoscopic Score (MES) and Ulcerative Colitis Endoscopic Index of Severity (UCEIS) and histological activity using the Nancy Index (NI), Robarts Histopathology Index (RHI), and Simplified Geboes Score (SGS).
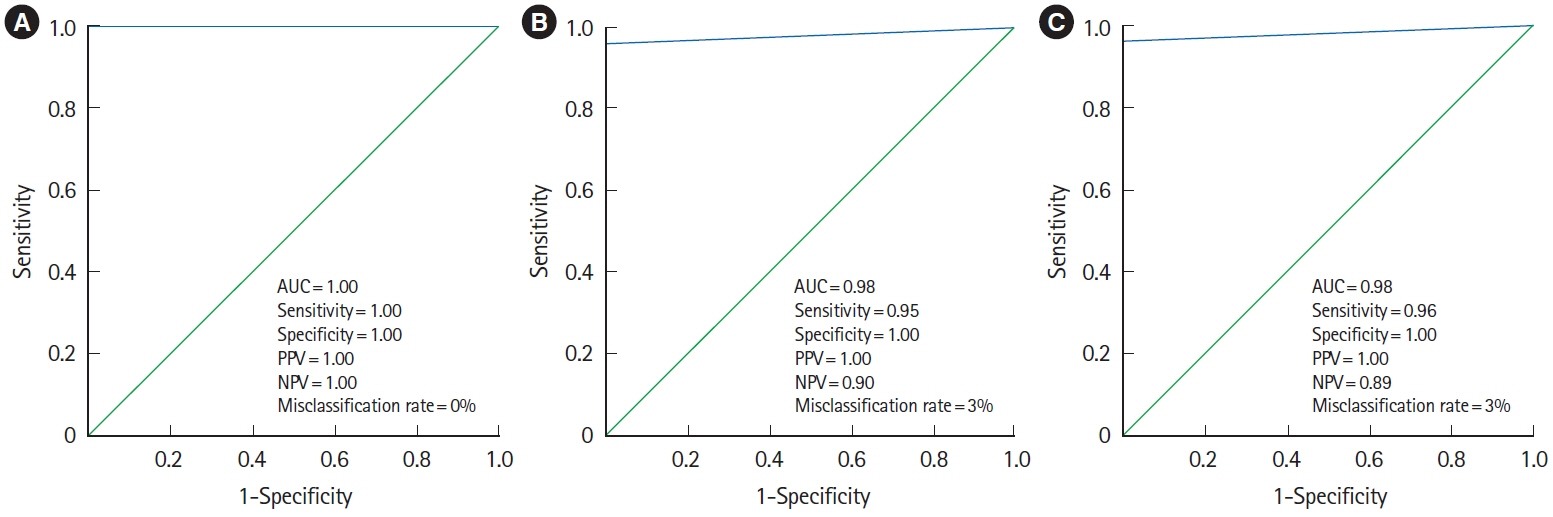
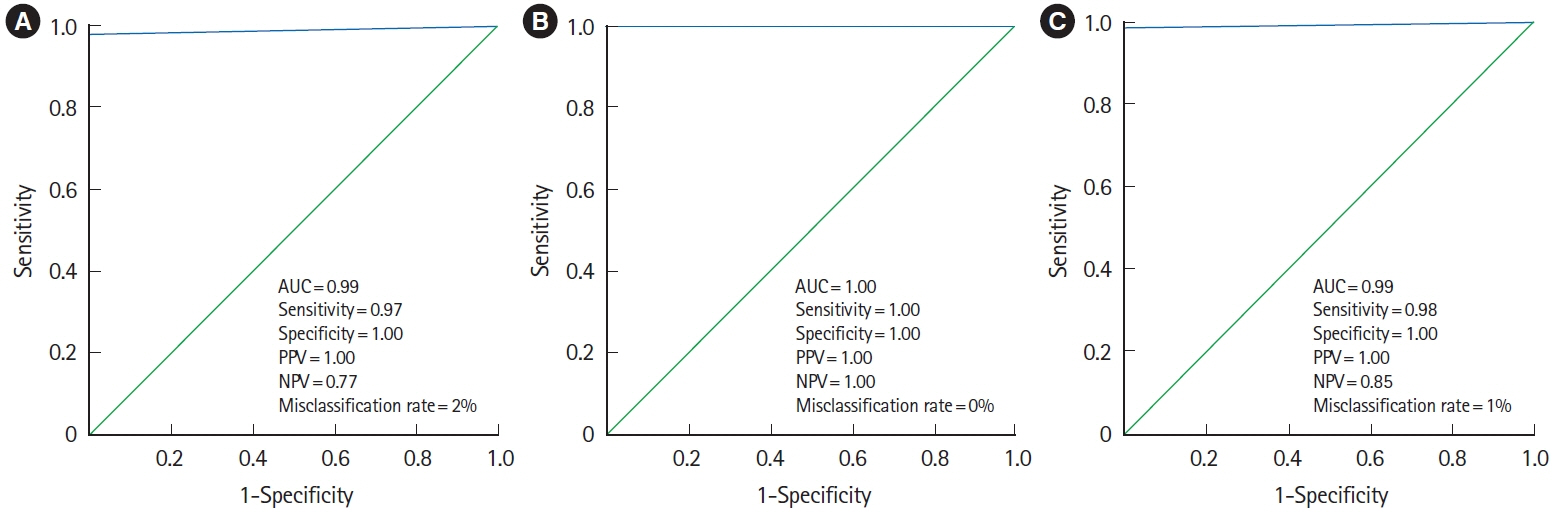
Results
Sigmoidoscopy showed a strong agreement with colonoscopy for MES and UCEIS with a kappa (κ) of 0.96 and 0.94 respectively. The misclassification rate for MES and UCEIS was 3% and 5% respectively. Sigmoidoscopy showed perfect agreement (κ = 1.00) with colonoscopy for assessment of the presence of endoscopic activity in the colon using MES ≥ 1 as activity criteria and strong agreement (κ = 0.93) using MES > 1 as activity criteria. Sigmoidoscopy showed strong agreement with colonoscopy for assessment of the presence of endoscopic activity using UCEIS (κ = 0.92). Strong agreement was observed between sigmoidoscopy and colonoscopy using NI (κ = 0.86), RHI (κ = 1.00), and SGS (κ = 0.92) for the detection of histological activity. The misclassification rate for the detection of histological activity was 2%, 0%, and 1% for NI, RHI, and SGS respectively.
Conclusions
Sigmoidoscopy showed strong agreement with colonoscopy for endoscopic and histologic disease activity. Sigmoidoscopy is adequate for assessment of disease activity in patients with UC during follow-up evaluation.
Figure
Reference
-
1. Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017; 389:1756–1770.
Article2. Peyrin-Biroulet L, Sandborn W, Sands BE, et al. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015; 110:1324–1338.3. Narang V, Kaur R, Garg B, et al. Association of endoscopic and histological remission with clinical course in patients of ulcerative colitis. Intest Res. 2018; 16:55–61.
Article4. Ozaki R, Kobayashi T, Okabayashi S, et al. Histological risk factors to predict clinical relapse in ulcerative colitis with endoscopically normal mucosa. J Crohns Colitis. 2018; 12:1288–1294.
Article5. Kornbluth A, Sachar DB; Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010; 105:501–523.6. Dignass A, Eliakim R, Magro F, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012; 6:965–990.
Article7. Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013; 7:982–1018.
Article8. Colombel JF, Ordás I, Ullman T, et al. Agreement between rectosigmoidoscopy and colonoscopy analyses of disease activity and healing in patients with ulcerative colitis. Gastroenterology. 2016; 150:389–395.
Article9. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987; 317:1625–1629.
Article10. Travis SP, Schnell D, Krzeski P, et al. Reliability and initial validation of the ulcerative colitis endoscopic index of severity. Gastroenterology. 2013; 145:987–995.
Article11. Turner D, Ricciuto A, Lewis A, et al. STRIDE-II: an update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology. 2021; 160:1570–1583.
Article12. Vuitton L, Peyrin-Biroulet L, Colombel JF, et al. Defining endoscopic response and remission in ulcerative colitis clinical trials: an international consensus. Aliment Pharmacol Ther. 2017; 45:801–813.
Article13. Magro F, Doherty G, Peyrin-Biroulet L, et al. ECCO Position Paper: harmonization of the approach to ulcerative colitis histopathology. J Crohns Colitis. 2020; 14:1503–1511.
Article14. Marchal-Bressenot A, Salleron J, Boulagnon-Rombi C, et al. Development and validation of the Nancy histological index for UC. Gut. 2017; 66:43–49.
Article15. Mosli MH, Feagan BG, Zou G, et al. Development and validation of a histological index for UC. Gut. 2017; 66:50–58.
Article16. Jauregui-Amezaga A, Geerits A, Das Y, et al. A simplified Geboes Score for ulcerative colitis. J Crohns Colitis. 2017; 11:305–313.
Article17. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012; 22:276–282.
Article18. Kato J, Kuriyama M, Hiraoka S, Yamamoto K. Is sigmoidoscopy sufficient for evaluating inflammatory status of ulcerative colitis patients? J Gastroenterol Hepatol. 2011; 26:683–687.
Article19. Jangi S, Holmer AK, Dulai PS, et al. Spatial evolution of histologic and endoscopic healing in the left and right colon in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2022; 20:e750–e760.
Article20. Lin WC, Chang CW, Chen MJ, Hsu TC, Wang HY. Effectiveness of sigmoidoscopy for assessing ulcerative colitis disease activity and therapeutic response. Medicine (Baltimore). 2019; 98:e15748.
Article21. Park SB, Kim SJ, Lee J, et al. Efficacy of sigmoidoscopy for evaluating disease activity in patients with ulcerative colitis. BMC Gastroenterol. 2022; 22:83.
Article22. Magro F, Lopes J, Borralho P, et al. Comparison of the Nancy index with continuous Geboes score: histological remission and response in ulcerative colitis. J Crohns Colitis. 2020; 14:1021–1025.
Article23. Peyrin-Biroulet L, Arenson E, Rubin DT, et al. A comparative evaluation of the measurement properties of three histological indices of mucosal healing in ulcerative colitis: Geboes score, Robarts histopathology index and Nancy index. J Crohns Colitis. 2023; 17:1733–1743.
Article24. Navaneethan U, Parasa S, Venkatesh PG, Trikudanathan G, Shen B. Prevalence and risk factors for colonic perforation during colonoscopy in hospitalized inflammatory bowel disease patients. J Crohns Colitis. 2011; 5:189–195.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comments on “Adequacy of sigmoidoscopy as compared to colonoscopy for assessment of disease activity in patients of ulcerative colitis: a prospective study”
- Response: Comments on “Adequacy of sigmoidoscopy as compared to colonoscopy for assessment of disease activity in patients of ulcerative colitis: a prospective study”
- Endoscopy for assessment of mucosal healing in ulcerative colitis: time bound or response guided?
- Usefulness of Magnifying Chromoscopy in Ulcerative Colitis
- A Case of Non-Hodgkin's Lymphoma in Ulcerative Colitis