Intest Res.
2024 Jul;22(3):286-296. 10.5217/ir.2023.00199.
Diagnostic strategy of irritable bowel syndrome: a low- and middle-income country perspective
- Affiliations
-
- 1Department of Internal Medicine, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
- 2Department of Physiology and Biochemistry, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
- 3Helicobacter pylori and Microbiota Study Group, Institute Tropical Disease, Universitas Airlangga, Surabaya, Indonesia
- 4Division of Gastroentero-Hepatology, Department of Internal Medicine, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
- 5Department of Gastroenterology, Dhaka Medical College and Hospital, Dhaka, Bangladesh
- 6Department of Internal Medicine, Universitas Muhammadiyah Surabaya, Surabaya, Indonesia
- 7Center of Excellence in Digestive Diseases and Gastroenterology Unit, Department of Medicine, Thammasat University, Pathumthani, Thailand
- KMID: 2558189
- DOI: http://doi.org/10.5217/ir.2023.00199
Abstract
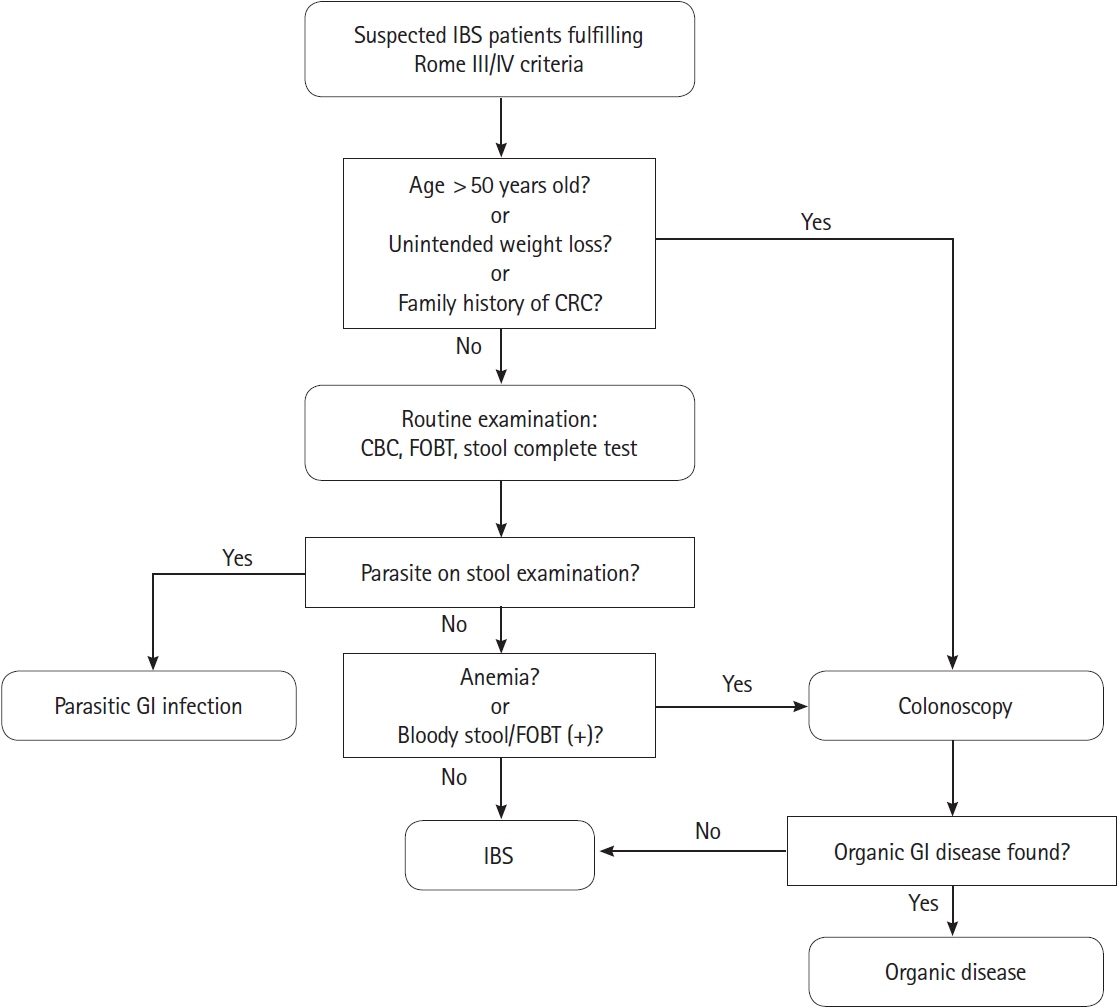
- Irritable bowel syndrome (IBS) is a highly prevalent gastrointestinal disorder associated with substantial impairment which considerably burdens healthcare systems worldwide. Research on IBS has largely been conducted in high-income countries posing barriers to the application of diagnostic strategies in low- and middle-income countries (LMICs) due to differences in disease characteristics, healthcare resources, and socioeconomic factors. This review discusses the diagnostic issues associated with LMICs. We present a concise overview of the relevant approaches and propose a diagnostic strategy based on the latest evidence. A positive diagnostic strategy that relies on appropriate symptom-based criteria is crucial within the diagnostic framework. A combination of complete blood count, fecal occult blood test, and complete stool test may reliably identify individuals with suspected IBS who are more likely to have organic diseases, thus justifying the necessity for a colonoscopy. Eventually, we developed a diagnostic algorithm based on a limited setting perspective that summarizes the available evidence and may be applied in LMICs.
Figure
Reference
-
1. Oka P, Parr H, Barberio B, Black CJ, Savarino EV, Ford AC. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020; 5:908–917.
Article2. Sperber AD, Dumitrascu D, Fukudo S, et al. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a Rome Foundation working team literature review. Gut. 2017; 66:1075–1082.
Article3. Ladep NG, Okeke EN, Samaila AA, et al. Irritable bowel syndrome among patients attending General Outpatients’ clinics in Jos, Nigeria. Eur J Gastroenterol Hepatol. 2007; 19:795–799.
Article4. Schmulson M, Ortíz O, Santiago-Lomeli M, et al. Frequency of functional bowel disorders among healthy volunteers in Mexico City. Dig Dis. 2006; 24:342–347.
Article5. Gwee KA. Irritable bowel syndrome in developing countries: a disorder of civilization or colonization? Neurogastroenterol Motil. 2005; 17:317–324.
Article6. Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019; 156:254–272.
Article7. Canavan C, West J, Card T. Review article: the economic impact of the irritable bowel syndrome. Aliment Pharmacol Ther. 2014; 40:1023–1034.8. Ladabaum U, Boyd E, Zhao WK, et al. Diagnosis, comorbidities, and management of irritable bowel syndrome in patients in a large health maintenance organization. Clin Gastroenterol Hepatol. 2012; 10:37–45.
Article9. Lacy BE, Patel H, Guérin A, et al. Variation in care for patients with irritable bowel syndrome in the United States. PLoS One. 2016; 11:e0154258.
Article10. Roshandel D, Rezailashkajani M, Shafaee S, Zali MR. A cost analysis of functional bowel disorders in Iran. Int J Colorectal Dis. 2007; 22:791–799.
Article11. Dean BB, Aguilar D, Barghout V, et al. Impairment in work productivity and health-related quality of life in patients with IBS. Am J Manag Care. 2005; 11(1 Suppl):S17–S26.12. Kanazawa M, Endo Y, Whitehead WE, Kano M, Hongo M, Fukudo S. Patients and nonconsulters with irritable bowel syndrome reporting a parental history of bowel problems have more impaired psychological distress. Dig Dis Sci. 2004; 49:1046–1053.
Article13. Kanazawa M, Drossman DA, Shinozaki M, et al. Translation and validation of a Japanese version of the irritable bowel syndrome-quality of life measure (IBS-QOL-J). Biopsychosoc Med. 2007; 1:6.
Article14. Drossman DA, Chang L, Schneck S, Blackman C, Norton WF, Norton NJ. A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. Dig Dis Sci. 2009; 54:1532–1541.15. Drossman DA, Morris CB, Schneck S, et al. International survey of patients with IBS: symptom features and their severity, health status, treatments, and risk taking to achieve clinical benefit. J Clin Gastroenterol. 2009; 43:541–550.16. Lacy BE, Everhart KK, Weiser KT, et al. IBS patients’ willingness to take risks with medications. Am J Gastroenterol. 2012; 107:804–809.
Article17. Frändemark Å, Törnblom H, Jakobsson S, Simrén M. Work productivity and activity impairment in irritable bowel syndrome (IBS): a multifaceted problem. Am J Gastroenterol. 2018; 113:1540–1549.
Article18. Leong SA, Barghout V, Birnbaum HG, et al. The economic consequences of irritable bowel syndrome: a US employer perspective. Arch Intern Med. 2003; 163:929–935.
Article19. Spiegel BM. Do physicians follow evidence-based guidelines in the diagnostic work-up of IBS? Nat Clin Pract Gastroenterol Hepatol. 2007; 4:296–297.
Article20. Spiegel BM, Farid M, Esrailian E, Talley J, Chang L. Is irritable bowel syndrome a diagnosis of exclusion? A survey of primary care providers, gastroenterologists, and IBS experts. Am J Gastroenterol. 2010; 105:848–858.
Article21. Corsetti M, Tack J, Attara G, Sewell M. IBS Global Impact Report 2018: uncovering the true burden of irritable bowel syndrome (IBS) on people’s lives. Vancouver: Gastrointestinal Society;2018.22. Lacy BE, Pimentel M, Brenner DM, et al. ACG Clinical Guideline: management of irritable bowel syndrome. Am J Gastroenterol. 2021; 116:17–44.
Article23. Begtrup LM, Engsbro AL, Kjeldsen J, et al. A positive diagnostic strategy is noninferior to a strategy of exclusion for patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2013; 11:956–962.
Article24. Flik CE, Laan W, Smout AJ, Weusten BL, de Wit NJ. Comparison of medical costs generated by IBS patients in primary and secondary care in the Netherlands. BMC Gastroenterol. 2015; 15:168.
Article25. Wilson GT, Walsh BT. Eating disorders in the DSM-IV. J Abnorm Psychol. 1991; 100:362–365.
Article26. Lamprecht F, Sack M. Posttraumatic stress disorder revisited. Psychosom Med. 2002; 64:222–237.
Article27. Manning AP, Thompson WG, Heaton KW, Morris AF. Towards positive diagnosis of the irritable bowel. Br Med J. 1978; 2:653–654.28. Mearin F, Lacy BE, Chang L, et al. Bowel disorders. Gastroenterology. 2016; 150:1393–1407.
Article29. Shivaji UN, Ford AC. Beliefs about management of irritable bowel syndrome in primary care: cross-sectional survey in one locality. Prim Health Care Res Dev. 2015; 16:263–269.
Article30. Sood R, Gracie DJ, Law GR, Ford AC. Systematic review with meta-analysis: the accuracy of diagnosing irritable bowel syndrome with symptoms, biomarkers and/or psychological markers. Aliment Pharmacol Ther. 2015; 42:491–503.
Article31. Ford AC, Chey WD, Talley NJ, Malhotra A, Spiegel BM, Moayyedi P. Yield of diagnostic tests for celiac disease in individuals with symptoms suggestive of irritable bowel syndrome: systematic review and meta-analysis. Arch Intern Med. 2009; 169:651–658.
Article32. Halpin SJ, Ford AC. Prevalence of symptoms meeting criteria for irritable bowel syndrome in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2012; 107:1474–1482.
Article33. Fairbrass KM, Costantino SJ, Gracie DJ, Ford AC. Prevalence of irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease in remission: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020; 5:1053–1062.
Article34. Irvine AJ, Chey WD, Ford AC. Screening for celiac disease in irritable bowel syndrome: an updated systematic review and meta-analysis. Am J Gastroenterol. 2017; 112:65–76.
Article35. Patel P, Bercik P, Morgan DG, et al. Prevalence of organic disease at colonoscopy in patients with symptoms compatible with irritable bowel syndrome: cross-sectional survey. Scand J Gastroenterol. 2015; 50:816–823.
Article36. Ishihara S, Yashima K, Kushiyama Y, et al. Prevalence of organic colonic lesions in patients meeting Rome III criteria for diagnosis of IBS: a prospective multi-center study utilizing colonoscopy. J Gastroenterol. 2012; 47:1084–1090.
Article37. Poon D, Law GR, Major G, Andreyev HJ. A systematic review and meta-analysis on the prevalence of non-malignant, organic gastrointestinal disorders misdiagnosed as irritable bowel syndrome. Sci Rep. 2022; 12:1949.
Article38. Hellström PM, Benno P. The Rome IV: irritable bowel syndrome: a functional disorder. Best Pract Res Clin Gastroenterol. 2019; 40-41:101634.39. Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006; 130:1480–1491.
Article40. Gwee KA, Bak YT, Ghoshal UC, et al. Asian consensus on irritable bowel syndrome. J Gastroenterol Hepatol. 2010; 25:1189–1205.
Article41. Whitehead WE, Palsson OS, Simrén M. Irritable bowel syndrome: what do the new Rome IV diagnostic guidelines mean for patient management? Expert Rev Gastroenterol Hepatol. 2017; 11:281–283.
Article42. Black CJ, Craig O, Gracie DJ, Ford AC. Comparison of the Rome IV criteria with the Rome III criteria for the diagnosis of irritable bowel syndrome in secondary care. Gut. 2021; 70:1110–1116.
Article43. Yadav YS, Eslick GD, Talley NJ. Review article: irritable bowel syndrome: natural history, bowel habit stability and overlap with other gastrointestinal disorders. Aliment Pharmacol Ther. 2021; 54 Suppl 1:S24–S32.
Article44. Barberio B, Houghton LA, Yiannakou Y, Savarino EV, Black CJ, Ford AC. Symptom stability in Rome IV vs Rome III irritable bowel syndrome. Am J Gastroenterol. 2021; 116:362–371.
Article45. Ghoshal UC, Abraham P, Bhatt C, et al. Epidemiological and clinical profile of irritable bowel syndrome in India: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2008; 27:22–28.46. Ghoshal UC, Abraham P, Bhatia SJ, et al. Comparison of Manning, Rome I, II, and III, and Asian diagnostic criteria: report of the multicentric Indian irritable bowel syndrome (MIIBS) study. Indian J Gastroenterol. 2013; 32:369–375.
Article47. Pop LL, Mureşan IA, Dumitraşcu DL. How much bloating in the irritable bowel syndrome? Rom J Intern Med. 2018; 56:221–226.
Article48. Rahman MM, Mahadeva S, Ghoshal UC. Epidemiological and clinical perspectives on irritable bowel syndrome in India, Bangladesh and Malaysia: a review. World J Gastroenterol. 2017; 23:6788–6801.
Article49. Gwee KA, Gonlachanvit S, Ghoshal UC, et al. Second Asian Consensus on irritable bowel syndrome. J Neurogastroenterol Motil. 2019; 25:343–362.
Article50. Quigley EM. Impact of bloating and distention in irritable bowel syndrome: have we wandered too far from the Manning creed? Clin Gastroenterol Hepatol. 2009; 7:7–8.
Article51. Sperber AD, Gwee KA, Hungin AP, et al. Conducting multinational, cross-cultural research in the functional gastrointestinal disorders: issues and recommendations: a Rome Foundation working team report. Aliment Pharmacol Ther. 2014; 40:1094–1102.
Article52. Aziz I, Törnblom H, Palsson OS, Whitehead WE, Simrén M. How the change in IBS criteria from Rome III to Rome IV impacts on clinical characteristics and key pathophysiological factors. Am J Gastroenterol. 2018; 113:1017–1025.
Article53. Palsson OS, Whitehead WE, van Tilburg MA, et al. Rome IV diagnostic questionnaires and tables for investigators and clinicians. Gastroenterology. 2016; 150:1481–1491.54. Ghoshal UC, Rahman MM, Pratap N, et al. Comparisons of the Rome III and Rome IV criteria for diagnosis of irritable bowel syndrome in Indian and Bangladeshi communities and internal shifts in the diagnostic categories of bowel disorders of gut-brain interactions. Neurogastroenterol Motil. 2023; 35:e14579.
Article55. Fukudo S, Okumura T, Inamori M, et al. Evidence-based clinical practice guidelines for irritable bowel syndrome 2020. J Gastroenterol. 2021; 56:193–217.
Article56. Quigley EM, Fried M, Gwee KA, et al. World Gastroenterology Organisation Global Guidelines irritable bowel syndrome: a global perspective update September 2015. J Clin Gastroenterol. 2016; 50:704–713.
Article57. Black TP, Manolakis CS, Di Palma JA. “Red flag” evaluation yield in irritable bowel syndrome. J Gastrointestin Liver Dis. 2012; 21:153–156.
Article58. Jellema P, van der Windt DA, Schellevis FG, van der Horst HE. Systematic review: accuracy of symptom-based criteria for diagnosis of irritable bowel syndrome in primary care. Aliment Pharmacol Ther. 2009; 30:695–706.
Article59. Asghar Z, Thoufeeq M, Kurien M, et al. Diagnostic yield of colonoscopy in patients with symptoms compatible with Rome IV functional bowel disorders. Clin Gastroenterol Hepatol. 2022; 20:334–341.
Article60. Whitehead WE, Palsson OS, Feld AD, et al. Utility of red flag symptom exclusions in the diagnosis of irritable bowel syndrome. Aliment Pharmacol Ther. 2006; 24:137–146.
Article61. Yang Q, Wei ZC, Liu N, et al. Predictive value of alarm symptoms in Rome IV irritable bowel syndrome: a multicenter cross-sectional study. World J Clin Cases. 2022; 10:563–575.
Article62. Tinmouth J, Lansdorp-Vogelaar I, Allison JE. Faecal immunochemical tests versus guaiac faecal occult blood tests: what clinicians and colorectal cancer screening programme organisers need to know. Gut. 2015; 64:1327–1337.63. Klem F, Wadhwa A, Prokop LJ, et al. Prevalence, risk factors, and outcomes of irritable bowel syndrome after infectious enteritis: a systematic review and meta-analysis. Gastroenterology. 2017; 152:1042–1054.
Article64. Hamm LR, Sorrells SC, Harding JP, et al. Additional investigations fail to alter the diagnosis of irritable bowel syndrome in subjects fulfilling the Rome criteria. Am J Gastroenterol. 1999; 94:1279–1282.
Article65. Ximénez C, Morán P, Rojas L, Valadez A, Gómez A. Reassessment of the epidemiology of amebiasis: state of the art. Infect Genet Evol. 2009; 9:1023–1032.
Article66. Patel P, Bercik P, Morgan DG, et al. Irritable bowel syndrome is significantly associated with somatisation in 840 patients, which may drive bloating. Aliment Pharmacol Ther. 2015; 41:449–458.
Article67. Shafiei Z, Esfandiari F, Sarkari B, Rezaei Z, Fatahi MR, Hosseini Asl SM. Parasitic infections in irritable bowel syndrome patients: evidence to propose a possible link, based on a casecontrol study in the south of Iran. BMC Res Notes. 2020; 13:264.
Article68. Burke KE, D’Amato M, Ng SC, Pardi DS, Ludvigsson JF, Khalili H. Microscopic colitis. Nat Rev Dis Primers. 2021; 7:39.
Article69. Phisalprapa P, Supakankunti S, Chaiyakunapruk N. Cost-effectiveness and budget impact analyses of colorectal cancer screenings in a low- and middle-income country: example from Thailand. J Med Econ. 2019; 22:1351–1361.
Article70. Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG Clinical Guidelines: colorectal cancer screening 2021. Am J Gastroenterol. 2021; 116:458–479.
Article71. Mujagic Z, Jonkers DM, Hungin AP, et al. Use of Rome criteria for the diagnosis of irritable bowel syndrome in primary care: a survey among European countries. Eur J Gastroenterol Hepatol. 2017; 29:651–656.
Article72. Remes Troche JM, Bernal Reyes R, Valladares Lepine MA, Alonso Lárraga O, Gómez Escudero O, Meléndez Mena D. Gastroenterology diagnosis and treatment guidelines of irritable bowel syndrome; clinical features and diagnostic criteria. Rev Gastroenterol Mex. 2009; 74:58–62.73. Ortiz-Garrido O, Schmulson MJ. Los medicos en latinoamerica reportan utilizar con mayor frecuencia los mas recientes criterios de Roma III para diagnosticar sindrome de intestino irritable en la clinica. Pero conocen realmente los criterios. Rev Gastroenterol Mex. 2012; 77(Suppl 3):95.74. Thompson WG, Drossman DA, Talley N. Rome III diagnostic questionnaire for the adult functional GI disorders (including alarm questions) and scoring algorithm. In: Drossman DA, Corazziari E, Delvaux M, et al. eds. Rome III: the functional gastrointestinal disorders. 3rd ed. McLean: Degnon Associates, 2006;917-951.75. Rajbhandari R, Blakemore S, Gupta N, et al. Crohn’s disease among the poorest billion: burden of Crohn’s disease in lowand lower-middle-income countries. Dig Dis Sci. 2023; 68:1226–1236.
Article76. Oxley H. Health policy. In: Organisation for Economic Co-operation and Development (OECD), ed. Getting it right: OECD Perspectives on Policy Challenges in Mexico. Paris: OECD, 2007:99-106.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Irritable bowel syndrome
- Irritable Bowel Syndrome: Is It Really a Functional Disorder? A New Perspective on Alteration of Enteric Nervous System
- Decreased Neuroplasticity May Play a Role in Irritable Bowel Syndrome: Implication From the Comorbidity of Depression and Irritable Bowel Syndrome
- What Is the Role of the Low FODMAP Diets in the Management of Irritable Bowel Syndrome?
- Pharmacological therapy for irritable bowel syndrome