J Yeungnam Med Sci.
2024 Jul;41(3):166-178. 10.12701/jyms.2024.00339.
Failed back surgery syndrome—terminology, etiology, prevention, evaluation, and management: a narrative review
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, Kyungpook National University, Kyungpook National University Chilgok Hospital, Daegu, Korea
- KMID: 2558141
- DOI: http://doi.org/10.12701/jyms.2024.00339
Abstract
- Amid the worldwide increase in spinal surgery rates, a significant proportion of patients continue to experience refractory chronic pain, resulting in reduced quality of life and escalated healthcare demands. Failed back surgery syndrome (FBSS) is a clinical condition characterized by persistent or recurrent pain after one or more spinal surgeries. The diverse characteristics and stigmatizing descriptions of FBSS necessitate a reevaluation of its nomenclature to reflect its complexity more accurately. Accurate identification of the cause of FBSS is hampered by the complex nature of the syndrome and limitations of current diagnostic labels. Management requires a multidisciplinary approach that may include pharmacological treatment, physical therapy, psychological support, and interventional procedures, emphasizing realistic goal-setting and patient education. Further research is needed to increase our understanding, improve diagnostic accuracy, and develop more effective management strategies.
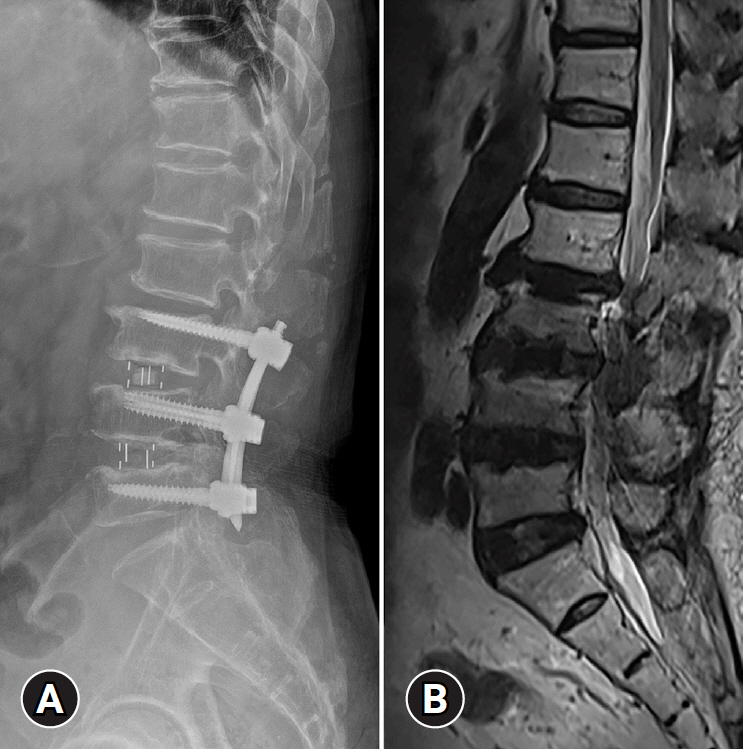
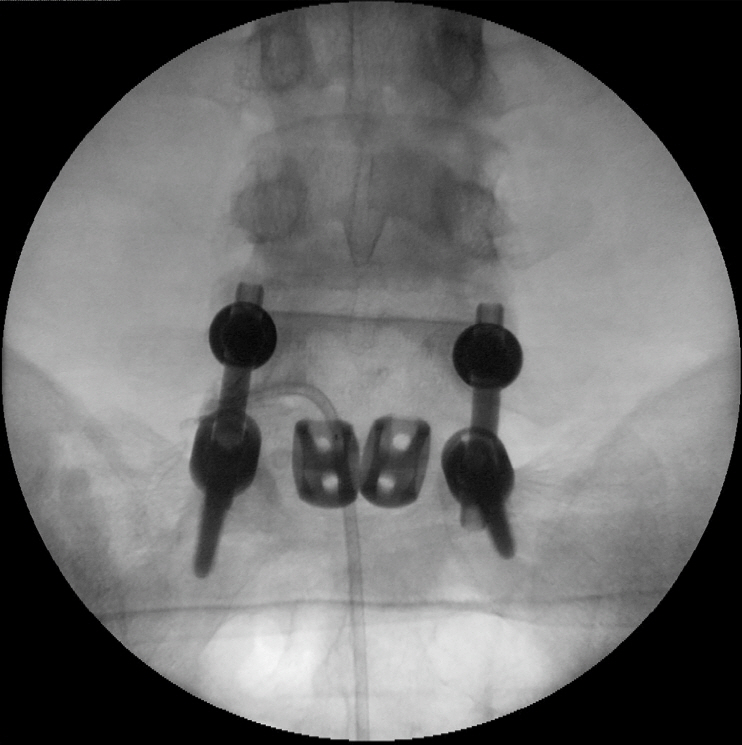
Figure
Reference
-
References
1. GBD 2021 Low Back Pain Collaborators. Global, regional, and national burden of low back pain, 1990-2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023; 5:e316–29.2. Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 2012; 37:67–76.3. National Health Insurance Service (NHIS). Annual report of major surgery statistics [Internet]. Wonju, Korea: NHIS;2021. [cited 2024 Mar 22]. https://www.nhis.or.kr/nhis/together/wbhaec06800m01.do?mode=view&articleNo=10813594.4. Kobayashi K, Sato K, Kato F, Kanemura T, Yoshihara H, Sakai Y, et al. Trends in the numbers of spine surgeries and spine surgeons over the past 15 years. Nagoya J Med Sci. 2022; 84:155–62.5. Grotle M, Småstuen MC, Fjeld O, Grøvle L, Helgeland J, Storheim K, et al. Lumbar spine surgery across 15 years: trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open. 2019; 9:e028743.6. Alshammari HS, Alshammari AS, Alshammari SA, Ahamed SS. Prevalence of chronic pain after spinal surgery: a systematic review and meta-analysis. Cureus. 2023; 15:e41841.7. Manca A, Eldabe S, Buchser E, Kumar K, Taylor RS. Relationship between health-related quality of life, pain, and functional disability in neuropathic pain patients with failed back surgery syndrome. Value Health. 2010; 13:95–102.8. Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res. 2016; 9:979–87.9. Waguespack A, Schofferman J, Slosar P, Reynolds J. Etiology of long-term failures of lumbar spine surgery. Pain Med. 2002; 3:18–22.10. Al Kaisy A, Pang D, Desai MJ, Pries P, North R, Taylor RS, et al. Failed back surgery syndrome: who has failed? Neurochirurgie. 2015; 61(Suppl 1):S6–14.11. Schug SA, Lavand’homme P, Barke A, Korwisi B, Rief W, Treede RD, et al. The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. Pain. 2019; 160:45–52.12. Christelis N, Simpson B, Russo M, Stanton-Hicks M, Barolat G, Thomson S, et al. Persistent spinal pain syndrome: a proposal for failed back surgery syndrome and ICD-11. Pain Med. 2021; 22:807–18.13. Carragee EJ, Alamin TF, Miller JL, Carragee JM. Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J. 2005; 5:24–35.14. Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J. 2006; 15(Suppl 1)(Suppl 1):S93–108.15. Young AK, Young BK, Riley LH 3rd, Skolasky RL. Assessment of presurgical psychological screening in patients undergoing spine surgery: use and clinical impact. J Spinal Disord Tech. 2014; 27:76–9.16. Nguyen TH, Randolph DC, Talmage J, Succop P, Travis R. Long-term outcomes of lumbar fusion among workers’ compensation subjects: a historical cohort study. Spine (Phila Pa 1976). 2011; 36:320–31.17. Pearce JM. Aspects of the failed back syndrome: role of litigation. Spinal Cord. 2000; 38:63–70.18. Siccoli A, Staartjes VE, Klukowska AM, Muizelaar JP, Schröder ML. Overweight and smoking promote recurrent lumbar disk herniation after discectomy. Eur Spine J. 2022; 31:604–13.19. Sandén B, Försth P, Michaëlsson K. Smokers show less improvement than nonsmokers two years after surgery for lumbar spinal stenosis: a study of 4555 patients from the Swedish spine register. Spine (Phila Pa 1976). 2011; 36:1059–64.20. Nakajima K, Miyahara J, Ohtomo N, Nagata K, Kato S, Doi T, et al. Impact of body mass index on outcomes after lumbar spine surgery. Sci Rep. 2023; 13:7862.21. Bokov A, Isrelov A, Skorodumov A, Aleynik A, Simonov A, Mlyavykh S. An analysis of reasons for failed back surgery syndrome and partial results after different types of surgical lumbar nerve root decompression. Pain Physician. 2011; 14:545–57.22. Chan CW, Peng P. Failed back surgery syndrome. Pain Med. 2011; 12:577–606.23. Leven D, Passias PG, Errico TJ, Lafage V, Bianco K, Lee A, et al. Risk factors for reoperation in patients treated surgically for intervertebral disc herniation: a subanalysis of eight-year SPORT data. J Bone Joint Surg Am. 2015; 97:1316–25.24. Javalkar V, Cardenas R, Tawfik TA, Khan IR, Bollam P, Banerjee AD, et al. Reoperations after surgery for lumbar spinal stenosis. World Neurosurg. 2011; 75:737–42.25. Arts MP, Kols NI, Onderwater SM, Peul WC. Clinical outcome of instrumented fusion for the treatment of failed back surgery syndrome: a case series of 100 patients. Acta Neurochir (Wien). 2012; 154:1213–7.26. Rubio-Haro R, DE Andrés-Serrano C, Noriega González DC, Bordes-García C, DE Andrés J. Adjacent segment syndrome after failed back surgery: biomechanics, diagnosis, and treatment. Minerva Anestesiol. 2022; 88:282–92.27. Rigoard P, Blond S, David R, Mertens P. Pathophysiological characterization of back pain generators in failed back surgery syndrome (part B). Neurochirurgie. 2015; 61(Suppl 1):S35–44.28. Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine (Phila Pa 1976). 1999; 24:1023–8.29. Bosscher HA, Heavner JE. Incidence and severity of epidural fibrosis after back surgery: an endoscopic study. Pain Pract. 2010; 10:18–24.30. Pereira P, Avelino A, Monteiro P, Vaz R, Castro-Lopes JM. New insights from immunohistochemistry for the characterization of epidural scar tissue. Pain Physician. 2014; 17:465–74.31. Clark R, Weber RP, Kahwati L. Surgical management of lumbar radiculopathy: a systematic review. J Gen Intern Med. 2020; 35:855–64.32. Xu W, Ran B, Luo W, Li Z, Gu R. Is lumbar fusion necessary for chronic low back pain associated with degenerative disk disease?: a meta-analysis. World Neurosurg. 2021; 146:298–306.33. Achttien RJ, Powell A, Zoulas K, Staal JB, Rushton A. Prognostic factors for outcome following lumbar spine fusion surgery: a systematic review and narrative synthesis. Eur Spine J. 2022; 31:623–68.34. Wang H, Sun W, Fu D, Shen Y, Chen YY, Wang LL. Update on biomaterials for prevention of epidural adhesion after lumbar laminectomy. J Orthop Translat. 2018; 13:41–9.35. Hosseini S, Niakan A, Dehghankhalili M, Dehdab R, Shahjouei S, Rekabdar Y, et al. Effects of adhesion barrier gel on functional outcomes of patients with lumbar disc herniation surgery; a systematic review and meta-analysis of clinical trials. Heliyon. 2021; 7:e07286.36. Jackson KL, Rumley J, Griffith M, Agochukwu U, DeVine J. Correlating psychological comorbidities and outcomes after spine surgery. Global Spine J. 2020; 10:929–39.37. Vlaeyen JW, Maher CG, Wiech K, Van Zundert J, Meloto CB, Diatchenko L, et al. Low back pain. Nat Rev Dis Primers. 2018; 4:52.38. Hazard RG. Failed back surgery syndrome: surgical and nonsurgical approaches. Clin Orthop Relat Res. 2006; 443:228–32.39. Bennett MI, Attal N, Backonja MM, Baron R, Bouhassira D, Freynhagen R, et al. Using screening tools to identify neuropathic pain. Pain. 2007; 127:199–203.40. Cohen SP, Hurley RW, Christo PJ, Winkley J, Mohiuddin MM, Stojanovic MP. Clinical predictors of success and failure for lumbar facet radiofrequency denervation. Clin J Pain. 2007; 23:45–52.41. Matsumoto J, Isu T, Kim K, Iwamoto N, Yamazaki K, Morimoto D, et al. Impact of additional treatment of paralumbar spine and peripheral nerve diseases after lumbar spine surgery. World Neurosurg. 2018; 112:e778–82.42. Young S, Aprill C, Laslett M. Correlation of clinical examination characteristics with three sources of chronic low back pain. Spine J. 2003; 3:460–5.43. Carleton RN, Kachur SS, Abrams MP, Asmundson GJ. Waddell’s symptoms as indicators of psychological distress, perceived disability, and treatment outcome. J Occup Rehabil. 2009; 19:41–8.44. Cohen SP, Doshi TL, Kurihara C, Dolomisiewicz E, Liu RC, Dawson TC, et al. Waddell (nonorganic) signs and their association with interventional treatment outcomes for low back pain. Anesth Analg. 2021; 132:639–51.45. Witkam RL, Buckens CF, van Goethem JW, Vissers KC, Henssen DJ. The current role and future directions of imaging in failed back surgery syndrome patients: an educational review. Insights Imaging. 2022; 13:117.46. Kizilkilic O, Yalcin O, Sen O, Aydin MV, Yildirim T, Hurcan C. The role of standing flexion-extension radiographs for spondylolisthesis following single level disk surgery. Neurol Res. 2007; 29:540–3.47. Dhagat PK, Jain M, Singh SN, Arora S, Leelakanth K. Failed back surgery syndrome: evaluation with magnetic resonance imaging. J Clin Diagn Res. 2017; 11:TC06–9.48. Lehr AM, Duits AA, Reijnders MR, Nutzinger D, Castelein RM, Oner FC, et al. Assessment of posterolateral lumbar fusion: a systematic review of imaging-based fusion criteria. JBJS Rev. 2022; 10:e22.00129.49. Cartolari R. Functional evaluation of the operated lumbar spine with axial loaded computed tomography (AL-CT). Riv Neuroradiol. 2002; 15:393–9.50. Kotsenas AL, Michalak GJ, DeLone DR, Diehn FE, Grant K, Halaweish AF, et al. CT metal artifact reduction in the spine: can an iterative reconstruction technique improve visualization? AJNR Am J Neuroradiol. 2015; 36:2184–90.51. Ryan PJ, Evans PA, Gibson T, Fogelman I. Chronic low back pain: comparison of bone SPECT with radiography and CT. Radiology. 1992; 182:849–54.52. Dessouky R, Khaleel M, Khalifa DN, Tantawy HI, Chhabra A. Magnetic resonance neurography of the lumbosacral plexus in failed back surgery syndrome. Spine (Phila Pa 1976). 2018; 43:839–47.53. Cashin AG, Wand BM, O’Connell NE, Lee H, Rizzo RR, Bagg MK, et al. Pharmacological treatments for low back pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2023; 4:CD013815.54. Enthoven WT, Roelofs PD, Deyo RA, van Tulder MW, Koes BW. Non-steroidal anti-inflammatory drugs for chronic low back pain. Cochrane Database Syst Rev. 2016; 2:CD012087.55. Ferreira GE, McLachlan AJ, Lin CC, Zadro JR, Abdel-Shaheed C, O’Keeffe M, et al. Efficacy and safety of antidepressants for the treatment of back pain and osteoarthritis: systematic review and meta-analysis. BMJ. 2021; 372:m4825.56. Bejarano G, Vining R, Desai DP, Minchew J, Michael Guo H, Goertz C. Development of a low back pain care pathway in an academic hospital system: results of a consensus process. J Orthop Surg Res. 2024; 19:11.57. Al-Ameri LT, Shukri ME, Hameed EK, Marzook AA. Pregabalin versus gabapentin efficacy in the management of neuropathic pain associated with failed back surgery syndrome. J Korean Neurosurg Soc. 2024; 67:202–8.58. Giménez-Campos MS, Pimenta-Fermisson-Ramos P, Díaz-Cambronero JI, Carbonell-Sanchís R, López-Briz E, Ruíz-García V. A systematic review and meta-analysis of the effectiveness and adverse events of gabapentin and pregabalin for sciatica pain. Aten Primaria. 2022; 54:102144.59. Tatit RT, Poetscher AW, Oliveira CA. Pregabalin and gabapentin for chronic low back pain without radiculopathy: a systematic review. Arq Neuropsiquiatr. 2023; 81:564–76.60. Petzke F, Klose P, Welsch P, Sommer C, Häuser W. Opioids for chronic low back pain: an updated systematic review and meta-analysis of efficacy, tolerability and safety in randomized placebo-controlled studies of at least 4 weeks of double-blind duration. Eur J Pain. 2020; 24:497–517.61. Nury E, Schmucker C, Nagavci B, Motschall E, Nitschke K, Schulte E, et al. Efficacy and safety of strong opioids for chronic noncancer pain and chronic low back pain: a systematic review and meta-analyses. Pain. 2022; 163:610–36.62. Song IA, Choi HR, Oh TK. Long-term opioid use and mortality in patients with chronic non-cancer pain: ten-year follow-up study in South Korea from 2010 through 2019. EClinicalMedicine. 2022; 51:101558.63. Gomes T, Juurlink DN, Antoniou T, Mamdani MM, Paterson JM, van den Brink W. Gabapentin, opioids, and the risk of opioid-related death: a population-based nested case-control study. PLoS Med. 2017; 14:e1002396.64. Hayden JA, Ellis J, Ogilvie R, Malmivaara A, van Tulder MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. 2021; 9:CD009790.65. Hayden JA, Ellis J, Ogilvie R, Stewart SA, Bagg MK, Stanojevic S, et al. Some types of exercise are more effective than others in people with chronic low back pain: a network meta-analysis. J Physiother. 2021; 67:252–62.66. Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015; 350:h444.67. Yang J, Lo WL, Zheng F, Cheng X, Yu Q, Wang C. Evaluation of cognitive behavioral therapy on improving pain, fear avoidance, and self-efficacy in patients with chronic low back pain: a systematic review and meta-analysis. Pain Res Manag. 2022; 2022:4276175.68. Williams AC, Fisher E, Hearn L, Eccleston C. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2020; 8:CD007407.69. Lin TH, Tam KW, Yang YL, Liou TH, Hsu TH, Rau CL. Meditation-based therapy for chronic low back pain management: a systematic review and meta-analysis of randomized controlled trials. Pain Med. 2022; 23:1800–11.70. Lee HM, Weinstein JN, Meller ST, Hayashi N, Spratt KF, Gebhart GF. The role of steroids and their effects on phospholipase A2: an animal model of radiculopathy. Spine (Phila Pa 1976). 1998; 23:1191–6.71. Verheijen EJ, Bonke CA, Amorij EM, Vleggeert-Lankamp CL. Epidural steroid compared to placebo injection in sciatica: a systematic review and meta-analysis. Eur Spine J. 2021; 30:3255–64.72. Mahmoud AM, Shawky MA, Farghaly OS, Botros JM, Alsaeid MA, Ragab SG. A systematic review and network meta-analysis comparing different epidural steroid injection approaches. Pain Pract. 2024; 24:341–63.73. Manchikanti L, Manchukonda R, Pampati V, Damron KS, McManus CD. Prevalence of facet joint pain in chronic low back pain in postsurgical patients by controlled comparative local anesthetic blocks. Arch Phys Med Rehabil. 2007; 88:449–55.74. Cohen SP, Bhaskar A, Bhatia A, Buvanendran A, Deer T, Garg S, et al. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Reg Anesth Pain Med. 2020; 45:424–67.75. Cohen SP, Moon JY, Brummett CM, White RL, Larkin TM. Medial branch blocks or intra-articular injections as a prognostic tool before lumbar facet radiofrequency denervation: a multicenter, case-control study. Reg Anesth Pain Med. 2015; 40:376–83.76. Abd-Elsayed A, Hughes M, Narel E, Loebertman MD. The efficacy of radiofrequency ablation for pain management in patients with pre-existing hardware at the site of ablation. Pain Ther. 2020; 9:709–16.77. Lee CH, Chung CK, Kim CH. The efficacy of conventional radiofrequency denervation in patients with chronic low back pain originating from the facet joints: a meta-analysis of randomized controlled trials. Spine J. 2017; 17:1770–80.78. Karimi H, Rodrigues R, Patel S, Patel J, Kosarchuk J, Kryzanski J. A systematic review and update on diagnosis and treatment of new onset sacroiliac joint dysfunction after lumbar fusion. Acta Neurochir (Wien). 2024; 166:43.79. Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother. 2013; 13:99–116.80. Janapala RN, Knezevic E, Knezevic NN, Pasupuleti R, Sanapati MR, Kaye AD, et al. Systematic review and meta-analysis of effectiveness of therapeutic sacroiliac joint injections. Pain Physician. 2023; 26:E413–35.81. Liu Y, Suvithayasiri S, Kim JS. Comparative efficacy of clinical interventions for sacroiliac joint pain: systematic review and network meta-analysis with preliminary design of treatment algorithm. Neurospine. 2023; 20:997–1010.82. Manchikanti L, Soin A, Boswell MV, Kaye AD, Sanapati M, Hirsch JA. Effectiveness of percutaneous adhesiolysis in post lumbar surgery syndrome: a systematic analysis of findings of systematic reviews. Pain Physician. 2019; 22:307–22.83. Geudeke MW, Krediet AC, Bilecen S, Huygen FJ, Rijsdijk M. Effectiveness of epiduroscopy for patients with failed back surgery syndrome: a systematic review and meta-analysis. Pain Pract. 2021; 21:468–81.84. Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, Molet J, et al. The effects of spinal cord stimulation in neuropathic pain are sustained: a 24-month follow-up of the prospective randomized controlled multicenter trial of the effectiveness of spinal cord stimulation. Neurosurgery. 2008; 63:762–70.85. Grider JS, Manchikanti L, Carayannopoulos A, Sharma ML, Balog CC, Harned ME, et al. Effectiveness of spinal cord stimulation in chronic spinal pain: a systematic review. Pain Physician. 2016; 19:E33–54.86. North RB, Kidd DH, Farrokhi F, Piantadosi SA. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005; 56:98–107.87. North RB, Kidd DH, Olin J, Sieracki JM, Farrokhi F, Petrucci L, et al. Spinal cord stimulation for axial low back pain: a prospective, controlled trial comparing dual with single percutaneous electrodes. Spine (Phila Pa 1976). 2005; 30:1412–8.88. Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, Molet J, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007; 132:179–88.89. Al-Kaisy A, Palmisani S, Pang D, Sanderson K, Wesley S, Tan Y, et al. Prospective, randomized, sham-control, double blind, crossover trial of subthreshold spinal cord stimulation at various kilohertz frequencies in subjects suffering from failed back surgery syndrome (SCS frequency study). Neuromodulation. 2018; 21:457–65.90. Taylor RS, Ryan J, O’Donnell R, Eldabe S, Kumar K, North RB. The cost-effectiveness of spinal cord stimulation in the treatment of failed back surgery syndrome. Clin J Pain. 2010; 26:463–9.91. Traeger AC, Gilbert SE, Harris IA, Maher CG. Spinal cord stimulation for low back pain. Cochrane Database Syst Rev. 2023; 3:CD014789.92. Dhruva SS, Murillo J, Ameli O, Morin PE, Spencer DL, Redberg RF, et al. Long-term outcomes in use of opioids, nonpharmacologic pain interventions, and total costs of spinal cord stimulators compared with conventional medical therapy for chronic pain. JAMA Neurol. 2023; 80:18–29.93. Raphael JH, Southall JL, Gnanadurai TV, Treharne GJ, Kitas GD. Long-term experience with implanted intrathecal drug administration systems for failed back syndrome and chronic mechanical low back pain. BMC Musculoskelet Disord. 2002; 3:17.94. Lara NA Jr, Teixeira MJ, Fonoff ET. Long term intrathecal infusion of opiates for treatment of failed back surgery syndrome. Acta Neurochir Suppl. 2011; 108:41–7.95. Hayek SM, Veizi E, Hanes M. Intrathecal hydromorphone and bupivacaine combination therapy for post-laminectomy syndrome optimized with patient-activated bolus device. Pain Med. 2016; 17:561–71.96. Cook CE, Garcia AN, Park C, Gottfried O. True differences in poor outcome risks between revision and primary lumbar spine surgeries. HSS J. 2021; 17:192–9.97. Gatzinsky K, Eldabe S, Deneuville JP, Duyvendak W, Naiditch N, Van Buyten JP, et al. Optimizing the management and outcomes of failed back surgery syndrome: a proposal of a standardized multidisciplinary team care pathway. Pain Res Manag. 2019; 2019:8184592.98. Jurak I, Delaš K, Erjavec L, Stare J, Locatelli I. Effects of multidisciplinary biopsychosocial rehabilitation on short-term pain and disability in chronic low back pain: a systematic review with network meta-analysis. J Clin Med. 2023; 12:7489.99. Bailey JC, Kurklinsky S, Sletten CD, Osborne MD. The effectiveness of an intensive interdisciplinary pain rehabilitation program in the treatment of post-laminectomy syndrome in patients who have failed spinal cord stimulation. Pain Med. 2018; 19:385–92.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Etiology, Evaluation, and Treatment of Failed Back Surgery Syndrome
- Failed Back Surgery Syndrome: A Review Article
- Current strategy for chronic pain after spinal surgery
- The Factors Affecting the Fovorable Outcomes in the Treatment of the Failed Back Surgery Syndrome
- Spinal Cord Stimulation in Pain Management: A Review