Korean J Pain.
2024 Jul;37(3):275-279. 10.3344/kjp.24021.
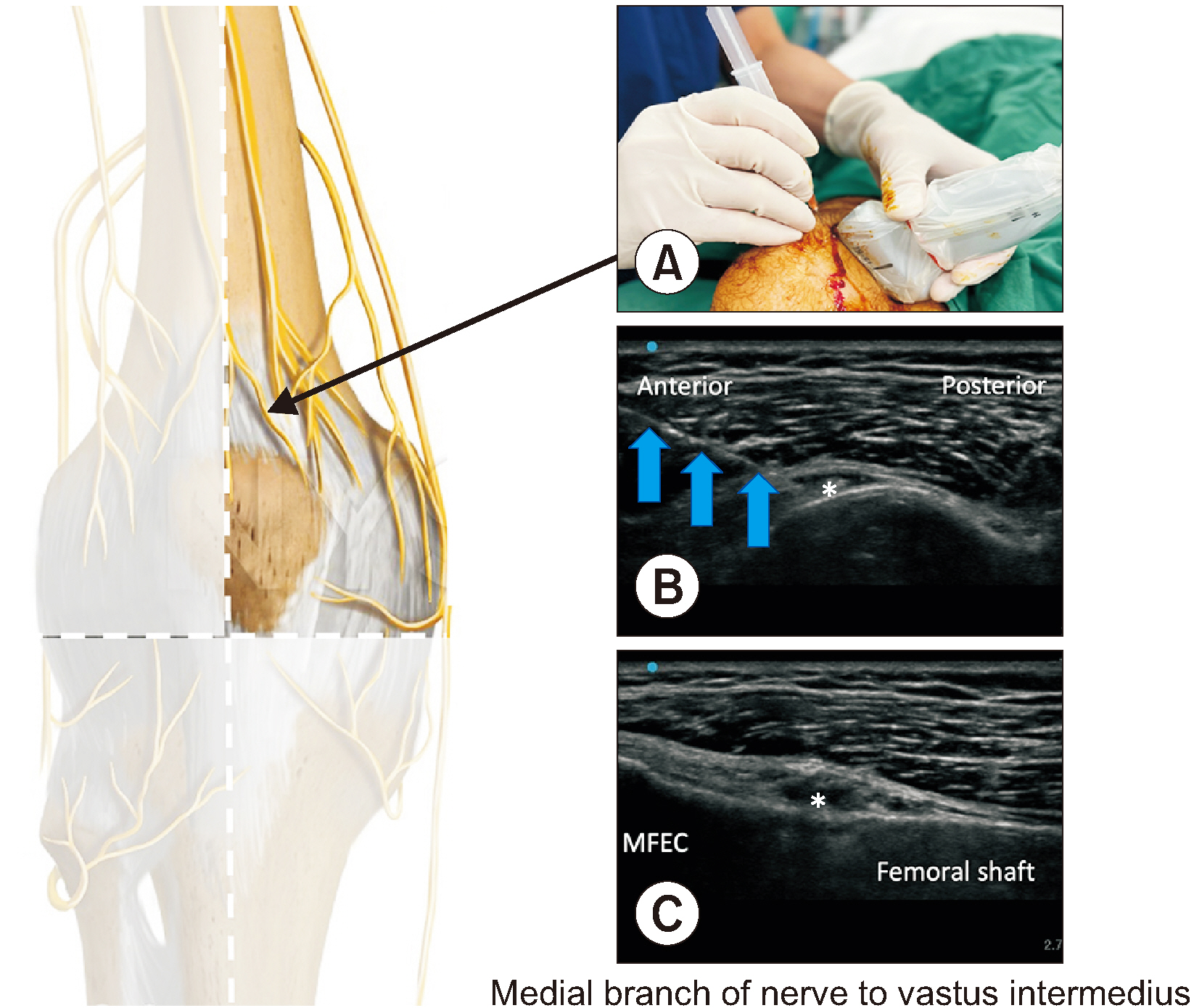
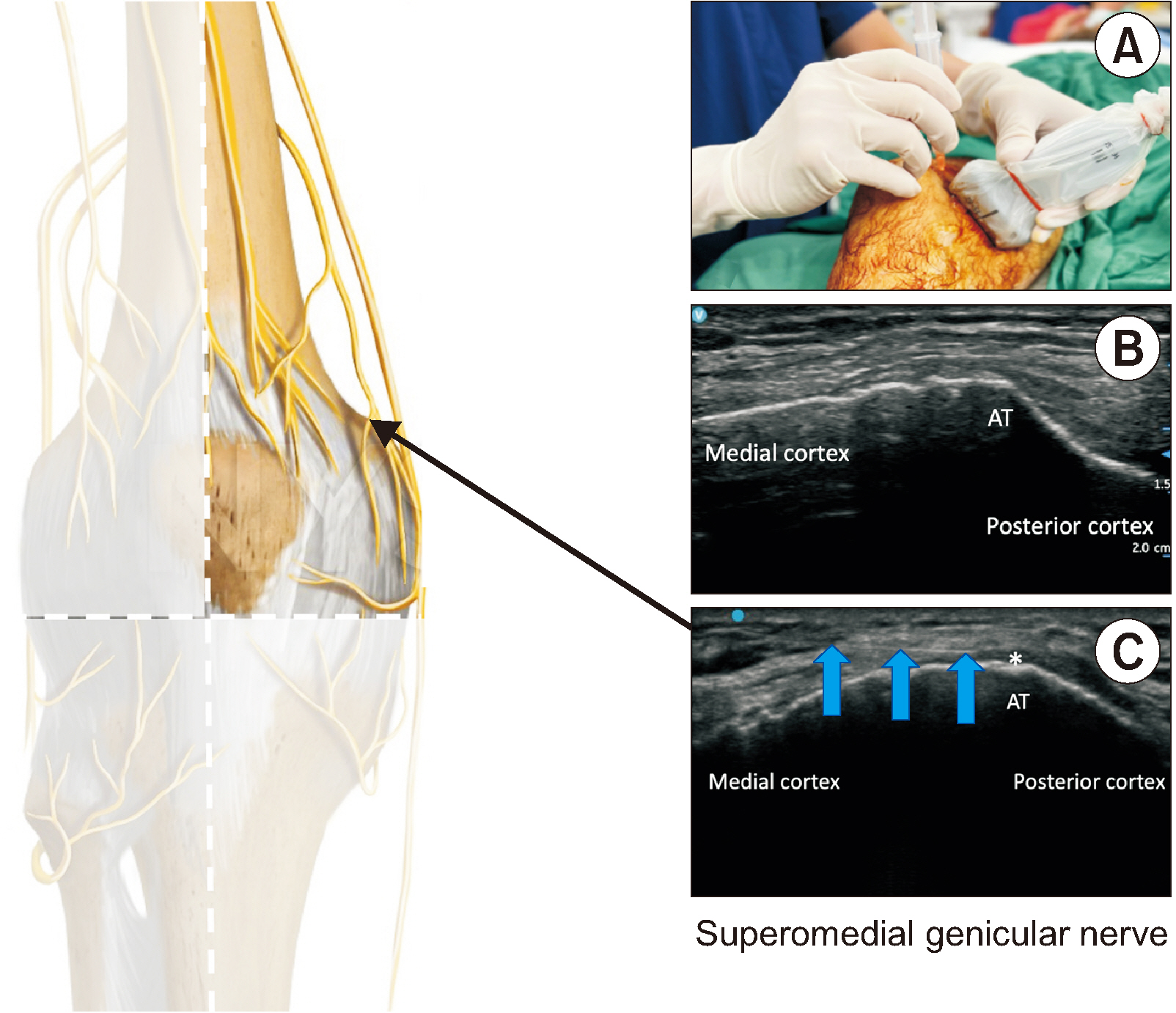
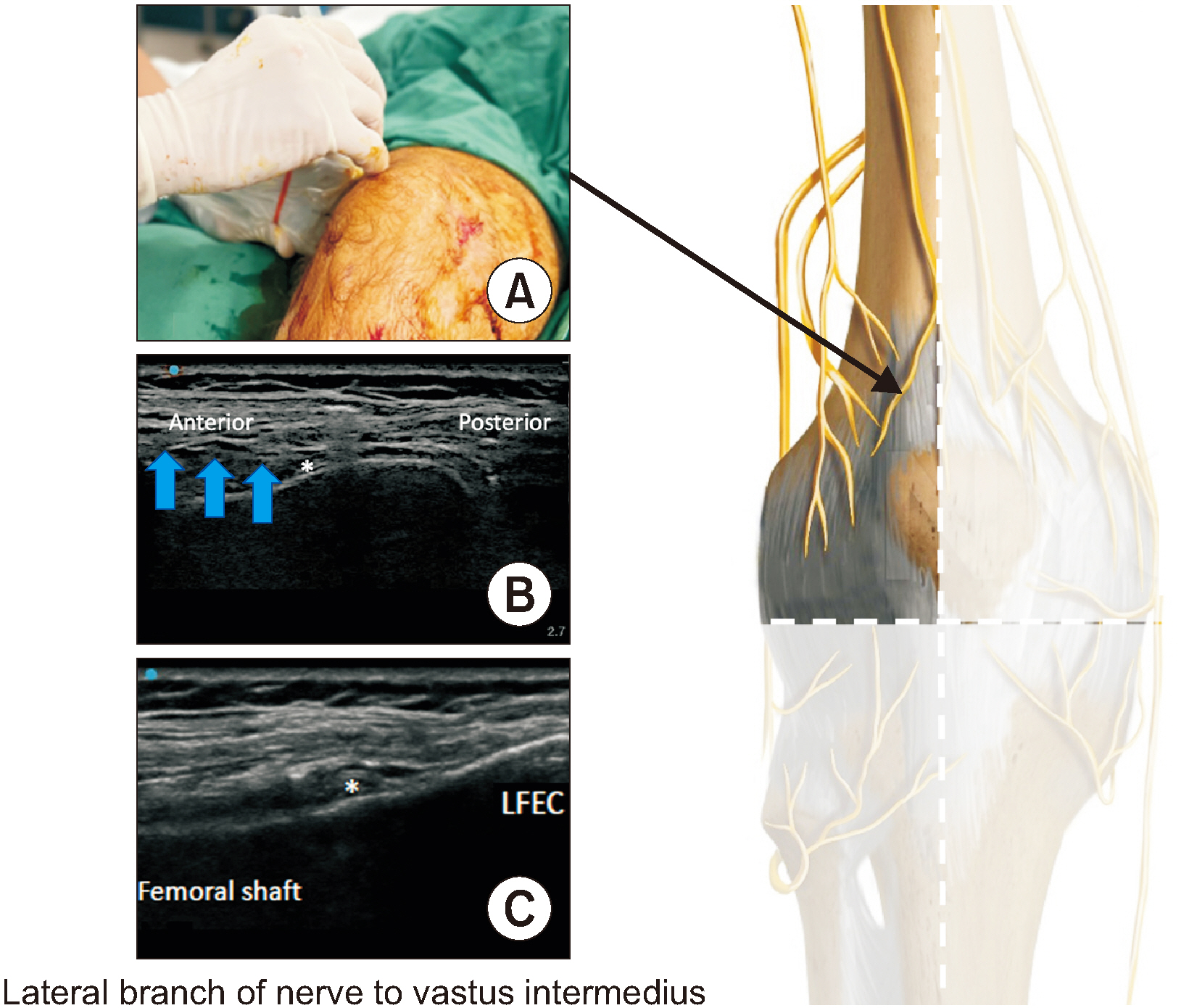
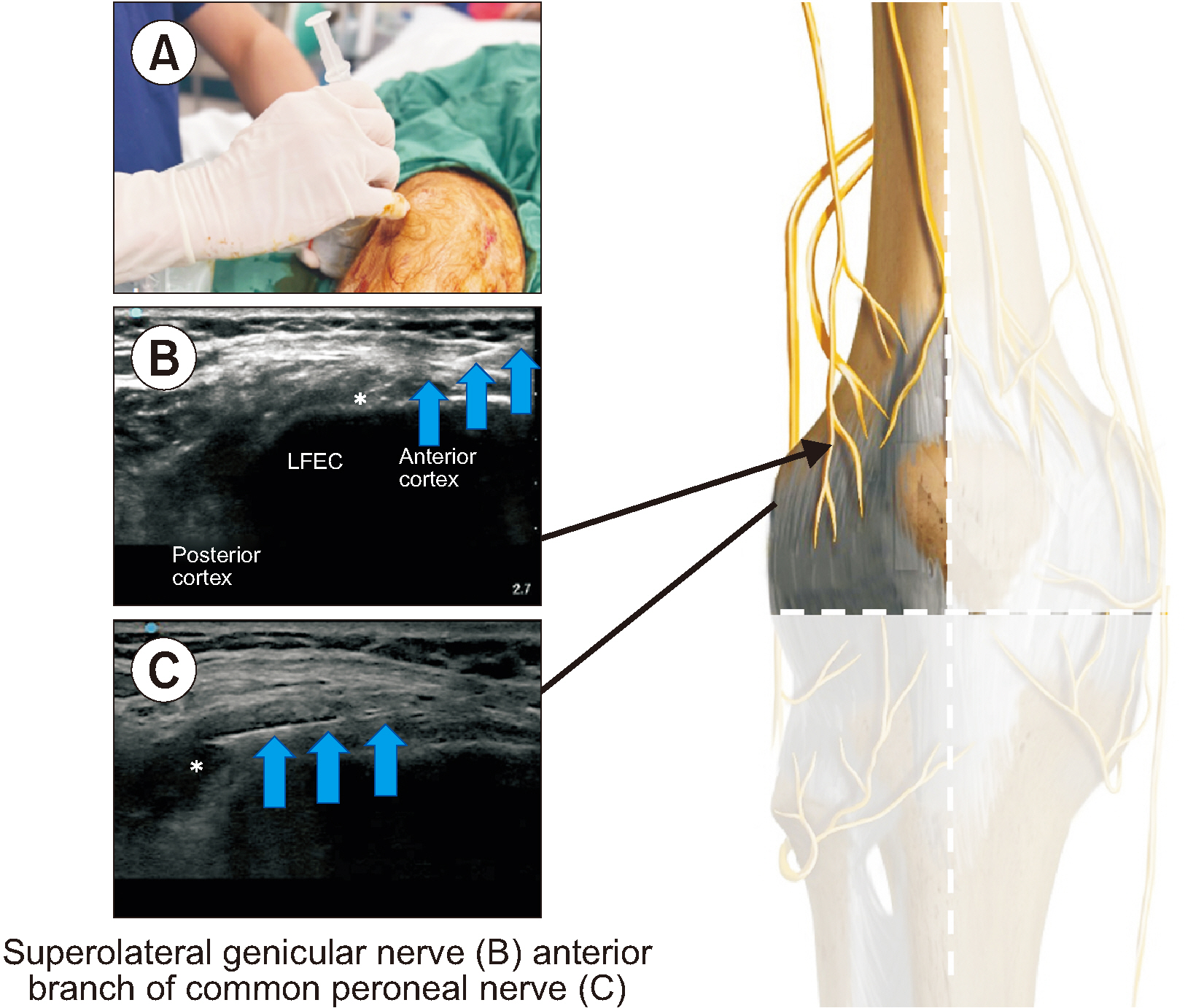
Optimizing genicular nerve chemical ablation
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, National Rehabilitation Center, San José, Costa Rica
- 2Frankston Pain Management, Melbourne, Australia
- 3The Faculty of Medicine, The University of Hong Kong, Hong Kong
- 4The Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong
- 5The Board of Clinical Research, The Hong Kong Institute of Musculoskeletal Medicine, Hong Kong
- 6Center for Regional Anesthesia and Pain Medicine, Wan Fang Hospital, Taipei Medical University, Taipei, Taiwan
- 7Center for Regional Anesthesia and Pain Medicine, Chung Shan Medical University Hospital, Taichung, Taiwan
- 8Department of Anaesthesia and Operating Theatre Services, Tuen Mun Hospital, Hong Kong
- 9Department of Anaesthesia, Boxhill Hospital, Melbourne, Australia
- KMID: 2557731
- DOI: http://doi.org/10.3344/kjp.24021
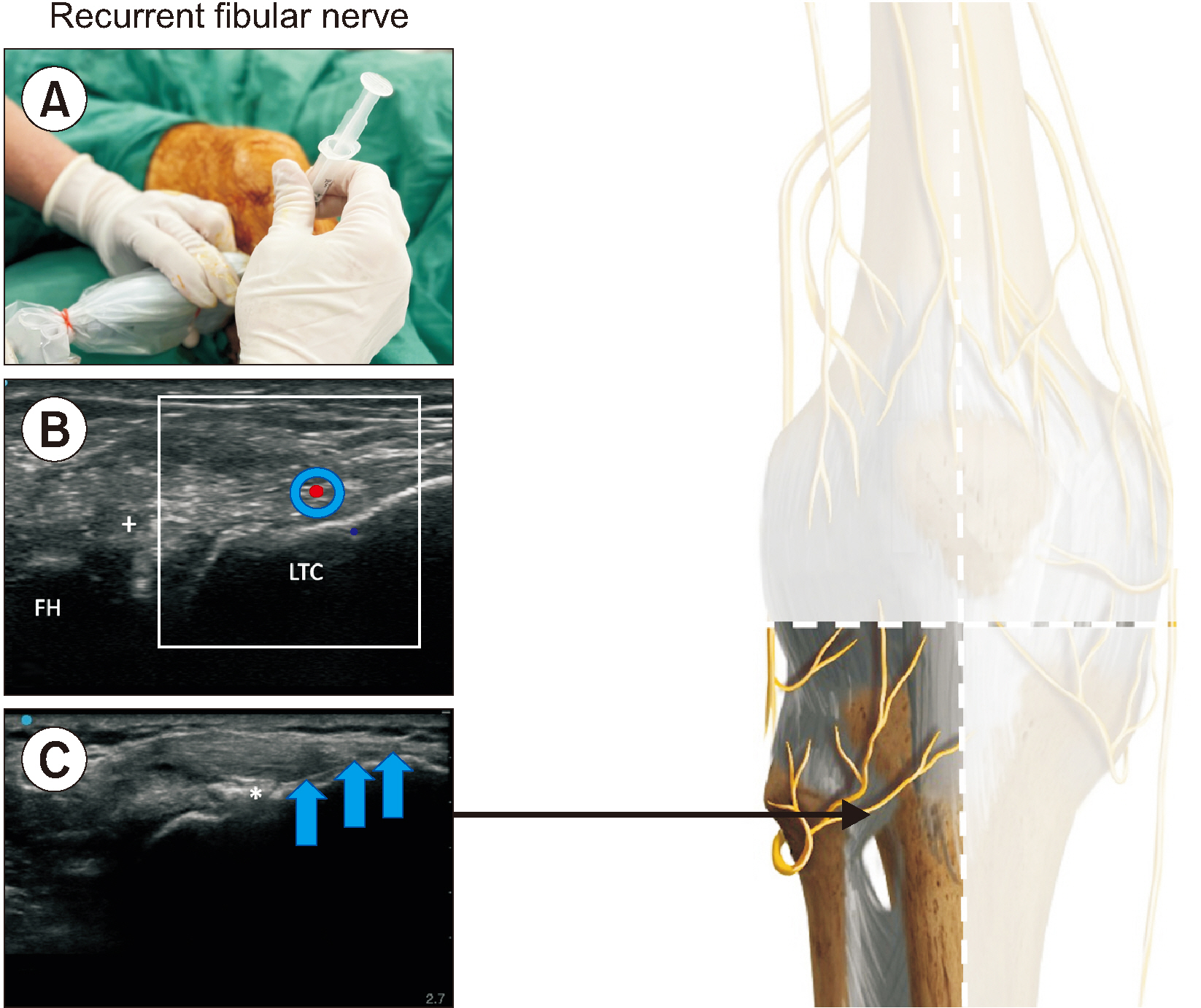
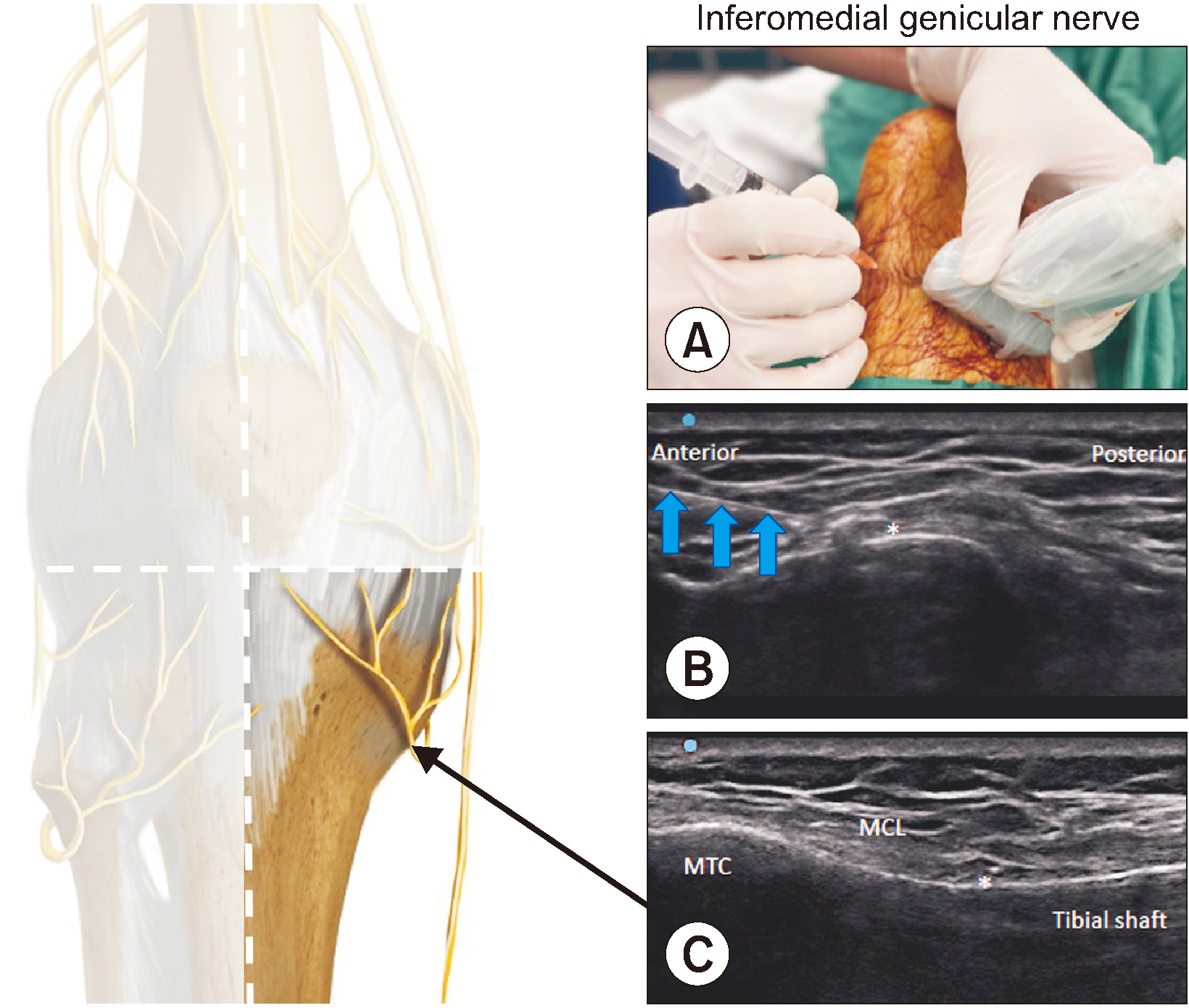
Figure
Cited by 1 articles
-
Genicular nerve radiofrequency ablation: proposal of a technical protocol for managing procedural pain
Andrés Rocha-Romero, Tony Kwun Tung Ng, Guilherme Ferreira-Dos-Santos
Korean J Pain. 2025;38(1):81-84. doi: 10.1136/rapm-2023-105127.
Reference
-
1. Yildiz G, Perdecioglu GRG, Yuruk D, Can E, Akkaya OT. 2023; Comparison of the efficacy of genicular nerve phenol neurolysis and radiofrequency ablation for pain management in patients with knee osteoarthritis. Korean J Pain. 36:450–7. DOI: 10.3344/kjp.23200. PMID: 37732409. PMCID: PMC10551393.
Article2. McCormick ZL, Cohen SP, Walega DR, Kohan L. 2021; Technical considerations for genicular nerve radiofrequency ablation: optimizing outcomes. Reg Anesth Pain Med. 46:518–23. DOI: 10.1136/rapm-2020-102117. PMID: 33483425.
Article3. Fonkoue L, Stoenoiu MS, Behets CW, Steyaert A, Kouassi JK, Detrembleur C, et al. 2021; Validation of a new protocol for ultrasound-guided genicular nerve radiofrequency ablation with accurate anatomical targets: cadaveric study. Reg Anesth Pain Med. 46:210–6. DOI: 10.1136/rapm-2020-101936. PMID: 33273065.
Article4. Ng TK, Lam KHS, Allam AE. 2022; Motor-sparing neural ablation with modified techniques for knee pain: case series on knee osteoarthritis and updated review of the underlying anatomy and available techniques. Biomed Res Int. 2022:2685898. DOI: 10.1155/2022/2685898. PMID: 35686229. PMCID: PMC9173899.
Article5. Guven Kose S, Kirac Unal Z, Kose HC, Celikel F, Akkaya OT. 2023; Ultrasound-guided genicular nerve radiofrequency treatment: prospective randomized comparative trial of a 3-nerve protocol versus a 5-nerve protocol. Pain Med. 24:758–67. DOI: 10.1093/pm/pnad025. PMID: 36869680.
Article6. Forero M, Olejnik LJ, Stager SC. 2023; Six-target radiofrequency ablation of the genicular nerve for the treatment of chronic knee pain. Reg Anesth Pain Med. doi: 10.1136/rapm-2023-104643. DOI: 10.1136/rapm-2023-104643. PMID: 37316307.
Article7. Krijgh DD, List EB, Teunis T, Bleys RLAW, Coert JH. 2022; The origin and course of the infrapatellar branch of the saphenous nerve: an anatomical study. JPRAS Open. 34:144–51. DOI: 10.1016/j.jpra.2022.08.006. PMID: 36304072. PMCID: PMC9593300.
Article8. Tran J, Peng PWH, Lam K, Baig E, Agur AMR, Gofeld M. 2018; Anatomical study of the innervation of anterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med. 43:407–14. DOI: 10.1097/AAP.0000000000000778. PMID: 29557887.9. Rocha-Romero A, Juárez-Lemus ÁM, Hernández-Porras BC. 2021; A safer step-by-step approach for erector spinae plane phenol neurolytic blocks. Can J Anaesth. 68:585–6. DOI: 10.1007/s12630-020-01901-3. PMID: 33420676. PMCID: PMC7793616.10. Risso RC, Ferraro LHC, Nouer Frederico T, Peng PWH, Luzo MV, Debieux P, et al. 2021; Chemical ablation of genicular nerve with phenol for pain relief in patients with knee osteoarthritis: a prospective study. Pain Pract. 21:438–44. DOI: 10.1111/papr.12972. PMID: 33277760.
Article11. Tran J, Peng P, Agur A. 2020; Evaluation of nerve capture using classical landmarks for genicular nerve radiofrequency ablation: 3D cadaveric study. Reg Anesth Pain Med. 45:898–906. DOI: 10.1136/rapm-2020-101894. PMID: 32928998.12. Rocha-Romero A. 2023; Diagnosis and treatment of post-radiofrequency synovial knee fistula: case report. A A Pract. 17:e01731. DOI: 10.1213/XAA.0000000000001731. PMID: 37991193.
Article13. Cosman ER Jr, Dolensky JR, Hoffman RA. 2014; Factors that affect radiofrequency heat lesion size. Pain Med. 15:2020–36. DOI: 10.1111/pme.12566. PMID: 25312825.
Article14. Bordoni B, Varacallo MA, Morabito B, Simonelli M. 2019; Biotensegrity or fascintegrity? Cureus. 11:e4819. DOI: 10.7759/cureus.4819.
Article15. Bordoni B, Myers T. 2020; A review of the theoretical fascial models: biotensegrity, fascintegrity, and myofascial chains. Cureus. 12:e7092. DOI: 10.7759/cureus.7092.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the efficacy of genicular nerve phenol neurolysis and radiofrequency ablation for pain management in patients with knee osteoarthritis
- Investigation of the existence of and a block technique for the inferior lateral genicular nerve: cadaveric study
- Predictive factors associated with successful response to utrasound guided genicular radiofrequency ablation
- Comparison of ultrasound guided pulsed radiofrequency of genicular nerve with local anesthetic and steroid block for management of osteoarthritis knee pain
- Retraction: Comparison of the efficacy of genicular nerve phenol neurolysis and radiofrequency ablation for pain management in patients with knee osteoarthritis