J Korean Assoc Oral Maxillofac Surg.
2024 Jun;50(3):134-139. 10.5125/jkaoms.2024.50.3.134.
Synchronous occurrence of oral squamous cell carcinoma and Warthin’s tumor: systematic review and case report
- Affiliations
-
- 1Departments of Oral and Maxillofacial Surgery, Yonsei University College of Dentistry, Seoul, Korea
- 2Departments of Oral Pathology, Yonsei University College of Dentistry, Seoul, Korea
- 3BK21 FOUR Project, Yonsei University College of Dentistry, Seoul, Korea
- 4Center for Genome Engineering, Institute for Basic Science, Daejeon, Korea
- KMID: 2557629
- DOI: http://doi.org/10.5125/jkaoms.2024.50.3.134
Abstract
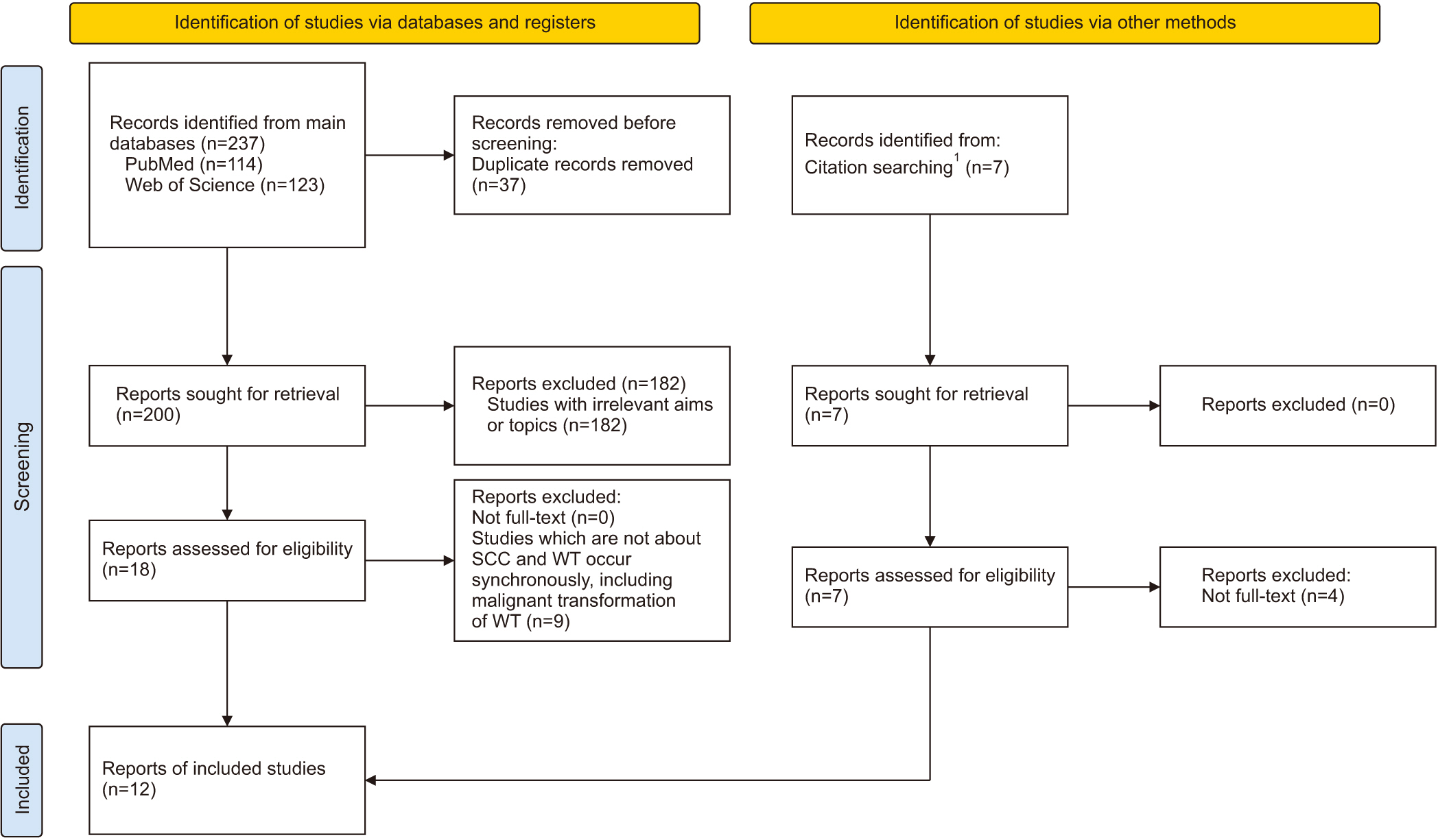
- We systematically reviewed the literature on the co-occurrence of squamous cell carcinoma (SCC) and Warthin’s tumor (WT), thought to be quite rare, to help reduce misdiagnosis and improve treatment planning. For this systematic review, we searched for articles in the Web of Science and PubMed databases, analyzed relevant studies for forward and backward citations, and identified only articles reporting on the “co-occurrence” of WT and SCC. Of the 237 studies identified, 12 comprising 18 patients met the inclusion criteria, to which we added one study from our institution. Most WTs were associated with SCC in the parotid gland or cervical lymph nodes. Most patients (89.5%) underwent selective or radical neck dissection due to identification of lesions separate from the primary SCC. Despite its frequent co-occurrence with other neoplasms, WT in the parotid or cervical lymph nodes tends to be misdiagnosed as a metastatic node when SCC is observed as the primary tumor. Factors to consider in diagnosis and neck management include identification of an association other than growth or development by lymphangiogenesis and whether the patient is a smoker, a strong risk factor.
Figure
Reference
-
References
1. El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ. El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ, editors. 2017. Tumours of salivary glands. WHO classification of head and neck tumours. 4th ed. IARC Publications;p. 159–201.2. Patterson JW, Wright ED, Camden S. 1999; Extraparotid Warthin's tumor. J Am Acad Dermatol. 40:468–70. https://doi.org/10.1016/s0190-9622(99)70499-8. DOI: 10.1016/S0190-9622(99)70499-8. PMID: 10071320.
Article3. Nupehewa D, Jayasooriya PR, Attygalla M, Tilakaratne WM. 2009; Synchronous occurrence of oral squamous cell carcinoma and Warthin tumor. Oral Med Pathol. 13:115–7. https://doi.org/10.3353/omp.13.115. DOI: 10.3353/omp.13.115.
Article4. Bhatlawande H, Desai KM, Kale AD, Angadi P, Hallikerimath S, Chibborah R. 2020; Co-occurrence of Warthin's tumor with oral squamous cell carcinoma - overlapping risk factors and implications. Oral Oncol. 100:104449. https://doi.org/10.1016/j.oraloncology.2019.104449. DOI: 10.1016/j.oraloncology.2019.104449. PMID: 31648865.
Article5. Sheahan P, Hafidh M, Toner M, Timon C. 2005; Unexpected findings in neck dissection for squamous cell carcinoma: incidence and implications. Head Neck. 27:28–35. https://doi.org/10.1002/hed.20110. DOI: 10.1002/hed.20110. PMID: 15459919.
Article6. Maiorano E, Lo Muzio L, Favia G, Piattelli A. 2002; Warthin's tumour: a study of 78 cases with emphasis on bilaterality, multifocality and association with other malignancies. Oral Oncol. 38:35–40. https://doi.org/10.1016/s1368-8375(01)00019-7. DOI: 10.1016/S1368-8375(01)00019-7. PMID: 11755819.
Article7. Sato T, Ishibashi K. 1998; Multicentric Warthin tumor of the paraparotid region mimicking lymph node metastases of homolateral oral and oropharyngeal squamous cell carcinoma: reports of two cases. J Oral Maxillofac Surg. 56:75–80. https://doi.org/10.1016/s0278-2391(98)90920-x. DOI: 10.1016/S0278-2391(98)90920-X. PMID: 9437986.
Article8. Schwarz E, Hürlimann S, Soyka JD, Bortoluzzi L, Strobel K. 2009; FDG-positive Warthin's tumors in cervical lymph nodes mimicking metastases in tongue cancer staging with PET/CT. Otolaryngol Head Neck Surg. 140:134–5. https://doi.org/10.1016/j.otohns.2008.09.019. DOI: 10.1016/j.otohns.2008.09.019. PMID: 19130980.
Article9. Enomoto A, Nakahara H, Uchihashi T, Tsuji H, Hamada S. 2011; Fluorodeoxyglucose-positive Warthin tumor in a neck node mimicking metastasis in primary intraosseous left posterior mandibular cancer staging with positron emission tomography/computed tomography. J Oral Maxillofac Surg. 69:2052–4. https://doi.org/10.1016/j.joms.2011.01.047. DOI: 10.1016/j.joms.2011.01.047. PMID: 21549478.
Article10. Iwai T, Baba J, Shibasaki M, Omura S, Hirota M, Mitsudo K, et al. 2012; 18F-fluorodeoxyglucose-positive Warthin tumor in a contralateral cervical lymph node mimicking metastasis in tongue cancer staging with PET/CT. J Craniofac Surg. 23:e507–9. https://doi.org/10.1097/scs.0b013e318266f750. DOI: 10.1097/SCS.0b013e318266f750. PMID: 22976724.
Article11. Sato K, Hayashi Y, Watanabe K, Hibi H. 2020; A case of Warthin tumors that were suspected to be lymph node metastases of maxillary gingival cancer. J Oral Maxillofac Surg Med Pathol. 32:291–5. https://doi.org/10.1016/j.ajoms.2020.03.011. DOI: 10.1016/j.ajoms.2020.03.011.
Article12. Kumar U, Rajkumar B, Kumar A, Kishore S, Jat B. 2020; Squamous cell carcinoma larynx with concurrent Warthin's tumor of the submandibular gland: a rarely reported co-existence. Indian J Pathol Microbiol. 63:331–3. https://doi.org/10.4103/ijpm.ijpm_436_19. DOI: 10.4103/IJPM.IJPM_436_19. PMID: 32317550.
Article13. Yang Y, Yang P, Liu X, Zhang Q. 2021; Warthin's tumor unexpectedly detected in submandibular gland after neck dissection in carcinoma of floor of mouth: a case report. J Maxillofac Oral Surg. 20:594–6. https://doi.org/10.1007/s12663-020-01330-1. DOI: 10.1007/s12663-020-01330-1. PMID: 34776691. PMCID: PMC8554888.
Article14. Goh Y, Ramanathan A, George Kallarakkal T, Kadir K. 2022; Oral squamous cell carcinoma and warthin tumour occurring as synchronous tumours: a report of two cases. Cureus. 14:e22547. https://doi.org/10.7759/cureus.22547. DOI: 10.7759/cureus.22547. PMID: 35345750. PMCID: PMC8956501.
Article15. Gontarz M, Gąsiorowski K, Bargiel J, Marecik T, Szczurowski P, Zapała J, et al. 2022; Extraparotid Warthin tumors imitating metastasis of oral cancers. Int Arch Otorhinolaryngol. 26:e278–80. https://doi.org/10.1055/s-0041-1724090. DOI: 10.1055/s-0041-1724090. PMID: 35602271. PMCID: PMC9122773.
Article16. Regional Office for the Western Pacific of World Health Organization. 2000; The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia. 378–420.17. Bishop JA, Thompson LDR, Wakely PE Jr, Weinreb I. 2021; Tumors of the salivary glands. American Registry of Pathology. DOI: 10.55418/9781933477947.
Article18. Anzai Y, Brunberg JA, Lufkin RB. 1997; Imaging of nodal metastases in the head and neck. J Magn Reson Imaging. 7:774–83. https://doi.org/10.1002/jmri.1880070503. DOI: 10.1002/jmri.1880070503. PMID: 9307901.
Article19. David O, Blaney S, Hearp M. 2007; Parotid gland fine-needle aspiration cytology: an approach to differential diagnosis. Diagn Cytopathol. 35:47–56. https://doi.org/10.1002/dc.20581. DOI: 10.1002/dc.20581. PMID: 17173301.
Article20. Park YM, Oh KH, Cho JG, Baek SK, Kwon SY, Jung KY, et al. 2018; Analysis of efficacy and safety of core-needle biopsy versus fine-needle aspiration cytology in patients with cervical lymphadenopathy and salivary gland tumour. Int J Oral Maxillofac Surg. 47:1229–35. https://doi.org/10.1016/j.ijom.2018.04.003. DOI: 10.1016/j.ijom.2018.04.003. PMID: 29706240.
Article21. Atula T, Greénman R, Laippala P, Klemi PJ. 1996; Fine-needle aspiration biopsy in the diagnosis of parotid gland lesions: evaluation of 438 biopsies. Diagn Cytopathol. 15:185–90. https://doi.org/10.1002/(sici)1097-0339(199609)15:3%3C185::aid-dc2%3E3.0.co;2-g. DOI: 10.1002/(SICI)1097-0339(199609)15:3<185::AID-DC2>3.0.CO;2-G.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Synchronous thyroid carcinoma and squamous cell carcinoma: A case report
- Spindle cell carcinoma of the tongue combined with double primary cancer of the thyroid gland: a case report
- Fine Needle Aspiration Cytology of the Warthin's Tumor Misinterpretated as Squamous Cell Carcinoma: A Case Report
- A Case of Synchronous Squamous Cell Carcinoma of the Bladder and Transitional Cell Carcinoma of the Ureter
- Synchronous Verrucous Carcinoma and Squamous Cell Carcinoma of Penis by Different Human Papillomavirus Infections