Clin Transplant Res.
2024 Jun;38(2):128-135. 10.4285/ctr.24.0017.
Risk factors for renal impairment after liver transplantation in Mongolia: a retrospective single-center study
- Affiliations
-
- 1Graduate School, Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia
- 2Department of Surgery, Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia
- 3The Transplantation Center, The First Central Hospital of Mongolia, Ulaanbaatar, Mongolia
- 4Department of Internal Medicine, Health Development Center, Ulaanbaatar, Mongolia
- 5School of Medicine, University of Utah, Salt Lake City, UT, USA
- 6Department of Nephrology, Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia
- KMID: 2557606
- DOI: http://doi.org/10.4285/ctr.24.0017
Abstract
- Background
Renal impairment (RI) is a frequent complication of liver cirrhosis and is associated with increased mortality and morbidity. Liver transplantation (LT) serves as an effective treatment method for patients with cirrhosis who have impaired renal function. However, renal function often declines after LT, influenced by various factors. This study aimed to investigate the factors contributing to RI following LT in our cases.
Methods
We analyzed the demographic data, preoperative and perioperative parameters, and postoperative outcomes of patients who underwent LT at the First Central Hospital of Mongolia from September 2011 to December 2022. Renal function was assessed by measuring the glomerular filtration rate using the Cockcroft-Gault creatinine clearance formula pretransplantation and at 24 hours, 72 hours, 7 days, 14 days, and 28 days post-LT.
Results
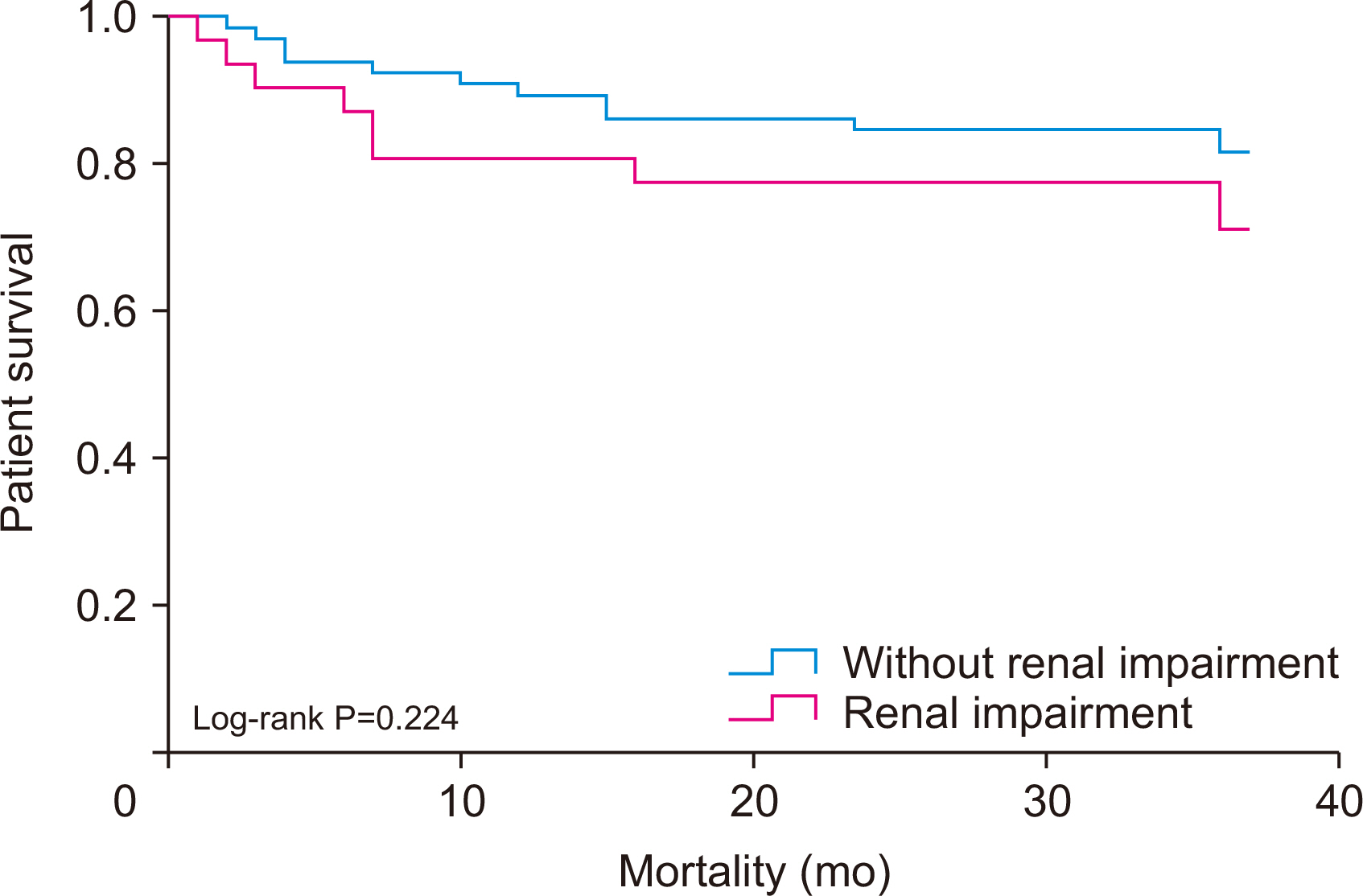
Several factors increased the risk of RI among recipients. These included female sex (odds ratio [OR], 3.06; 95% confidence interval [CI], 1.58–5.91), Child-TurcottePugh (CTP) scores of B and C (OR, 4.23; 95% CI, 0.92–19.41 and OR, 7.68; 95% CI, 1.67– 35.30, respectively), preoperative continuous renal replacement therapy (CRRT; OR, 5.86; 95% CI, 1.1–31.21), and a high graft-to-recipient weight ratio (GRWR; OR, 3.45; 95% CI, 1.23–9.63). Additionally, the survival rates for recipients with RI post-LT were 93.4% at 1 year and 78.1% at 3 years.
Conclusions
Female sex, a high CTP score, preoperative CRRT, and high GRWR were identified as risk factors for RI after LT in Mongolia.
Figure
Reference
-
1. Garcia-Tsao G, Parikh CR, Viola A. 2008; Acute kidney injury in cirrhosis. Hepatology. 48:2064–77. DOI: 10.1002/hep.22605. PMID: 19003880.
Article2. Daugaard TR, Pommergaard HC, Rostved AA, Rasmussen A. 2018; Postoperative complications as a predictor for survival after liver transplantation - proposition of a prognostic score. HPB (Oxford). 20:815–22. DOI: 10.1016/j.hpb.2018.03.001. PMID: 29705344.
Article3. Feldkamp T, Bienholz A, Paul A, Saner FH. 2020; Renal damage after liver transplantation. Biosci Rep. 40:BSR20191187. DOI: 10.1042/BSR20191187. PMID: 31851363. PMCID: PMC6944654.
Article4. Hilmi IA, Damian D, Al-Khafaji A, Planinsic R, Boucek C, Sakai T, et al. 2015; Acute kidney injury following orthotopic liver transplantation: incidence, risk factors, and effects on patient and graft outcomes. Br J Anaesth. 114:919–26. DOI: 10.1093/bja/aeu556. PMID: 25673576.
Article5. Cabezuelo JB, Ramírez P, Ríos A, Acosta F, Torres D, Sansano T, et al. 2006; Risk factors of acute renal failure after liver transplantation. Kidney Int. 69:1073–80. DOI: 10.1038/sj.ki.5000216. PMID: 16528257.
Article6. O'Riordan A, Wong V, McQuillan R, McCormick PA, Hegarty JE, Watson AJ. 2007; Acute renal disease, as defined by the RIFLE criteria, post-liver transplantation. Am J Transplant. 7:168–76. DOI: 10.1111/j.1600-6143.2006.01602.x. PMID: 17109735.7. Baatarkhuu O, Gerelchimeg T, Munkh-Orshikh D, Batsukh B, Sarangua G, Amarsanaa J. 2018; Epidemiology, genotype distribution, prognosis, control, and management of viral hepatitis B, C, D, and hepatocellular carcinoma in Mongolia. Euroasian J Hepatogastroenterol. 8:57–62. DOI: 10.5005/jp-journals-10018-1260. PMID: 29963464. PMCID: PMC6024043.8. Baatarkhuu O, Uugantsetseg G, Munkh-Orshikh D, Naranzul N, Badamjav S, Tserendagva D, et al. 2017; Viral hepatitis and liver diseases in Mongolia. Euroasian J Hepatogastroenterol. 7:68–72. DOI: 10.5005/jp-journals-10018-1215. PMID: 29201776. PMCID: PMC5663778.
Article9. McCauley J, Van Thiel DH, Starzl TE, Puschett JB. 1990; Acute and chronic renal failure in liver transplantation. Nephron. 55:121–8. DOI: 10.1159/000185938. PMID: 2362625. PMCID: PMC2957102.
Article10. Rimola A, Gavaler JS, Schade RR, el-Lankany S, Starzl TE, Van Thiel DH. 1987; Effects of renal impairment on liver transplantation. Gastroenterology. 93:148–56. DOI: 10.1016/0016-5085(87)90327-1. PMID: 3556303.
Article11. Bilbao I, Charco R, Balsells J, Lazaro JL, Hidalgo E, Llopart L, et al. 1998; Risk factors for acute renal failure requiring dialysis after liver transplantation. Clin Transplant. 12:123–9. PMID: 9575400.12. Colliou É, Del Bello A, Milongo D, Muscari F, Vallet M, Tack I, et al. 2022; Kidney failure after liver transplantation. Nephrol Ther. 18:89–103. DOI: 10.1016/j.nephro.2021.11.002. PMID: 35151596.
Article13. Wilhelm SM, Kale-Pradhan PB. 2011; Estimating creatinine clearance: a meta-analysis. Pharmacotherapy. 31:658–64. DOI: 10.1592/phco.31.7.658. PMID: 21923452.
Article14. Cockcroft DW, Gault MH. 1976; Prediction of creatinine clearance from serum creatinine. Nephron. 16:31–41. DOI: 10.1159/000180580. PMID: 1244564.
Article15. Jo JY, Ryu SA, Kim JI, Lee EH, Choi IC. 2019; Comparison of five glomerular filtration rate estimating equations as predictors of acute kidney injury after cardiovascular surgery. Sci Rep. 9:11072. DOI: 10.1038/s41598-019-47559-w. PMID: 31363147. PMCID: PMC6667489.
Article16. Moore RD, Smith CR, Lipsky JJ, Mellits ED, Lietman PS. 1984; Risk factors for nephrotoxicity in patients treated with aminoglycosides. Ann Intern Med. 100:352–7. DOI: 10.7326/0003-4819-100-3-352. PMID: 6364908.17. Park Y, Hirose R, Dang K, Xu F, Behrends M, Tan V, et al. 2008; Increased severity of renal ischemia-reperfusion injury with venous clamping compared to arterial clamping in a rat model. Surgery. 143:243–51. DOI: 10.1016/j.surg.2007.07.041. PMID: 18242341.
Article18. Pacheco MP, Carneiro-D'Albuquerque LA, Mazo DF. 2022; Current aspects of renal dysfunction after liver transplantation. World J Hepatol. 14:45–61. DOI: 10.4254/wjh.v14.i1.45. PMID: 35126839. PMCID: PMC8790396.
Article19. Leithead JA, Ferguson JW, Hayes PC. 2012; Modifiable patient factors are associated with the late decline in renal function following liver transplantation. Clin Transplant. 26:E316–23. DOI: 10.1111/j.1399-0012.2012.01650.x. PMID: 22686956.
Article20. Fussner LA, Charlton MR, Heimbach JK, Fan C, Dierkhising R, Coss E, et al. 2014; The impact of gender and NASH on chronic kidney disease before and after liver transplantation. Liver Int. 34:1259–66. DOI: 10.1111/liv.12381. PMID: 24262002.21. Braun N, Dette S, Viebahn R. 2003; Impairment of renal function following liver transplantation. Transplant Proc. 35:1458–60. DOI: 10.1016/S0041-1345(03)00486-X. PMID: 12826191.
Article22. Guitard J, Cointault O, Kamar N, Muscari F, Lavayssière L, Suc B, et al. 2006; Acute renal failure following liver transplantation with induction therapy. Clin Nephrol. 65:103–12. DOI: 10.5414/CNP65103. PMID: 16509459.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact factors leading to renal impairment after liver transplant surgery: a single center study
- Donor’s quality of life after living donor liver transplantation and influencing factors in Mongolia
- Four-year experience of liver transplantation in National Cancer Center of Mongolia
- Pediatric kidney transplantation in Mongolia
- Blood product transfusion in liver transplantation in First Clinical Hospital of Mongolia