Clin Transplant Res.
2024 Jun;38(2):106-115. 10.4285/ctr.24.0007.
Perioperative optic nerve sheath diameter variations in patients with end-stage renal failure undergoing robotic-assisted kidney transplant: a prospective observational study
- Affiliations
-
- 1Department of Anesthesia and Critical Care, Aster Medcity, Kochi, India
- KMID: 2557604
- DOI: http://doi.org/10.4285/ctr.24.0007
Abstract
- Background
Patients with chronic kidney disease (CKD) who undergo hemodialysis are predisposed to interstitial cerebral edema. Robotic-assisted laparoscopic surgery can increase optic nerve sheath diameter (ONSD) and intracranial pressure. The impact of robotic-assisted kidney transplant (RAKT) on ONSD is complicated by the presence of CKD, the administration of furosemide and mannitol, and the manipulation of hemodynamics. We examined ONSD variations in patients undergoing RAKT over a 1-year period at our institution. Furthermore, we attempted to identify any perioperative hemodynamic factors influencing these changes.
Methods
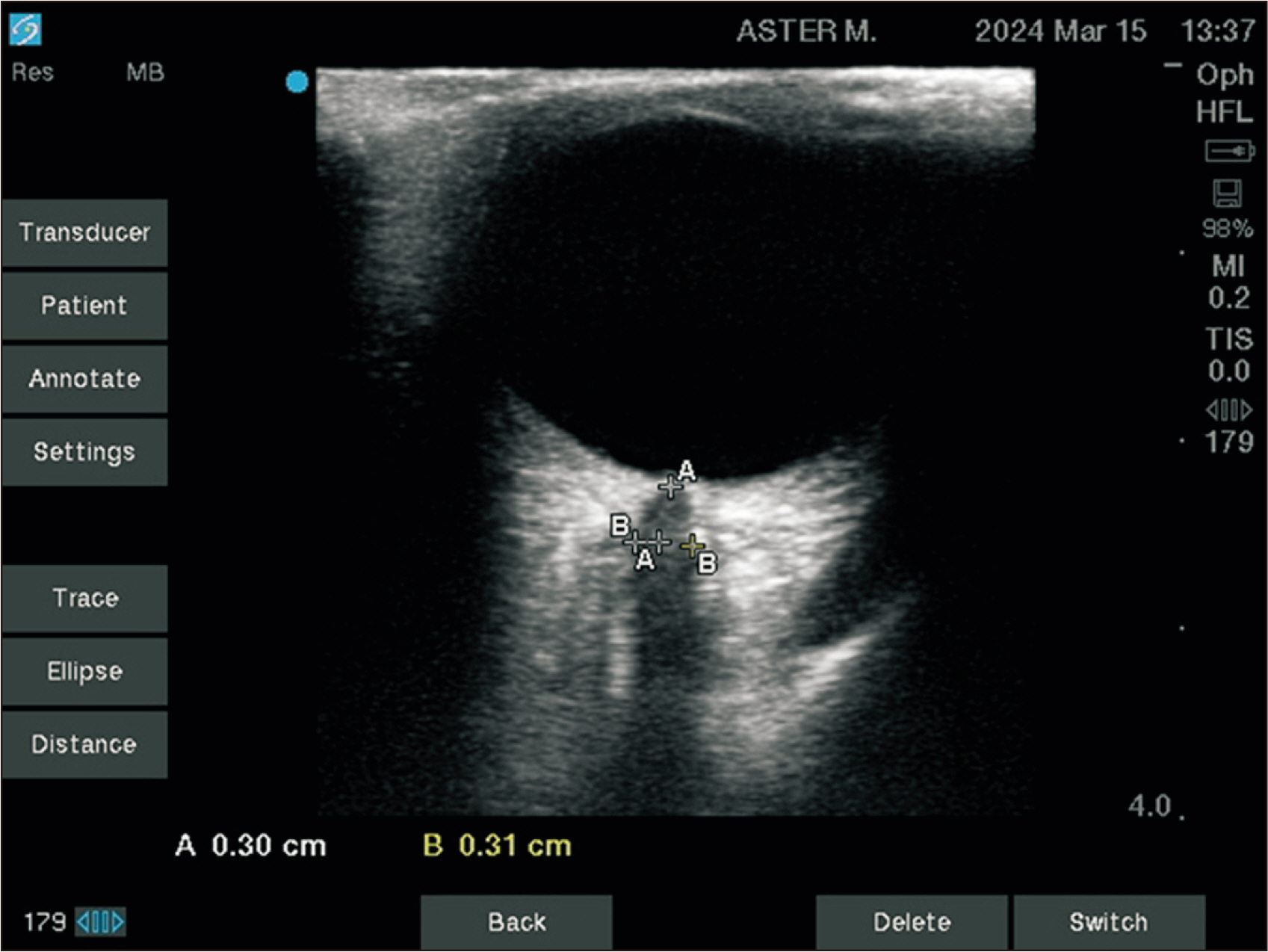
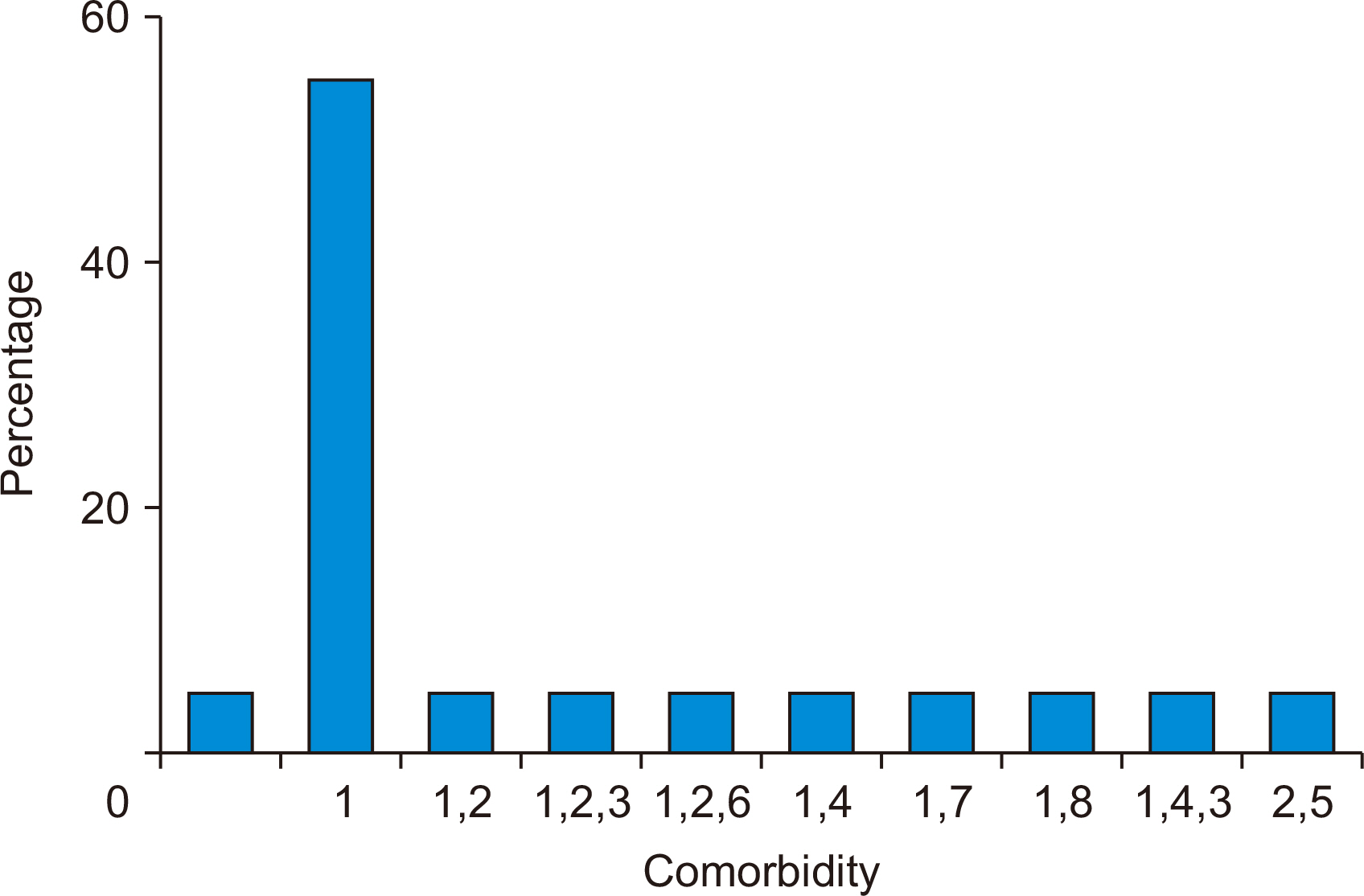
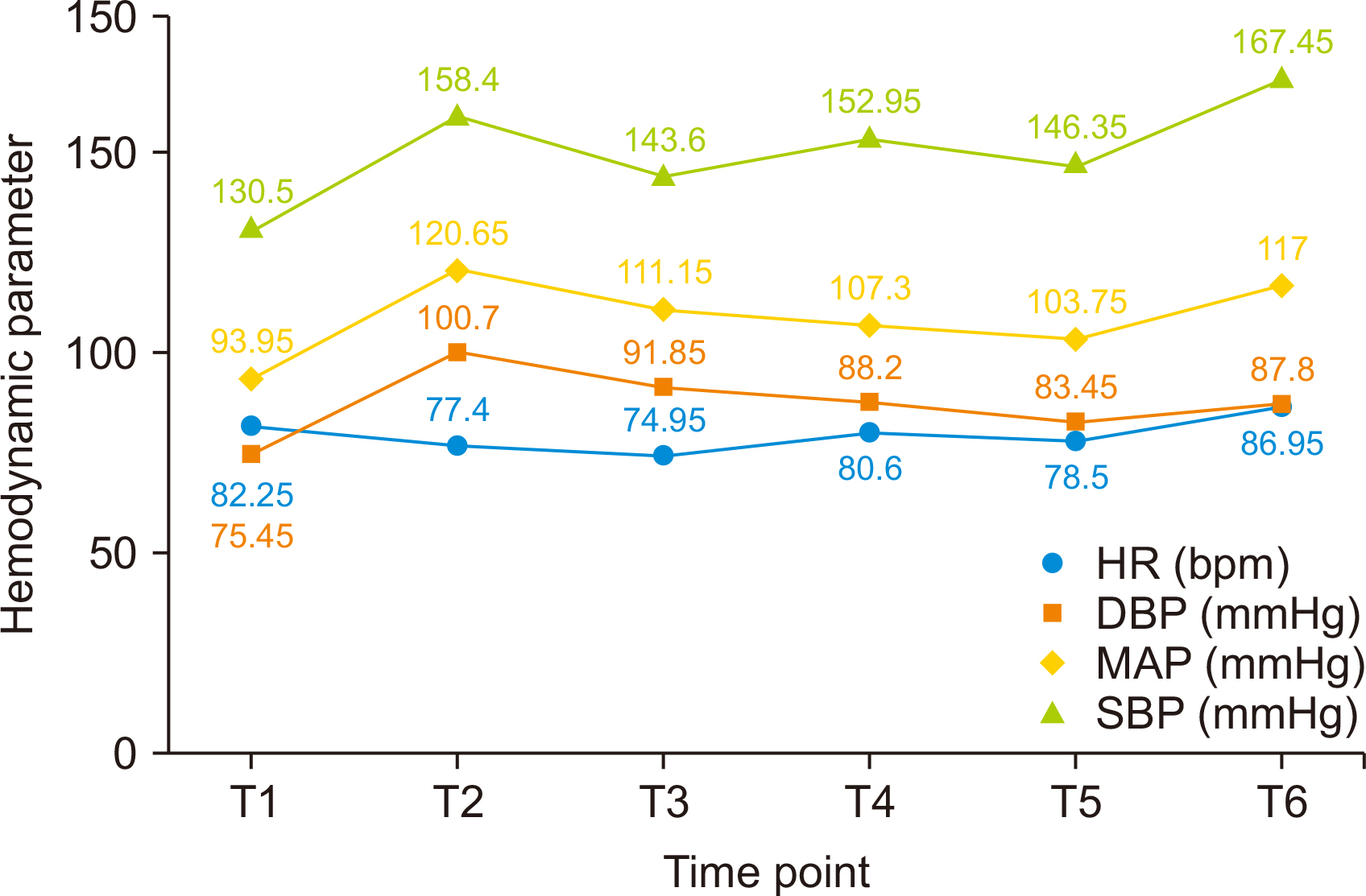
This prospective study included 20 patients undergoing RAKT. ONSD, heart rate, central venous pressure, systolic blood pressure, diastolic blood pressure (DBP), and mean arterial pressure (MAP) were measured following intubation (T1), after assuming the steep Trendelenburg position (T2), 1 hour after docking (T3), upon reperfusion (T4), after transition to the supine position (T5), and 3 hours postextubation (T6). Repeated measures analysis of variance with post hoc Bonferroni correction was employed to compare variables at each time point. Pearson correlation analysis was utilized to assess relationships between variables. P-values ≤0.05 were considered to indicate statistical significance.
Results
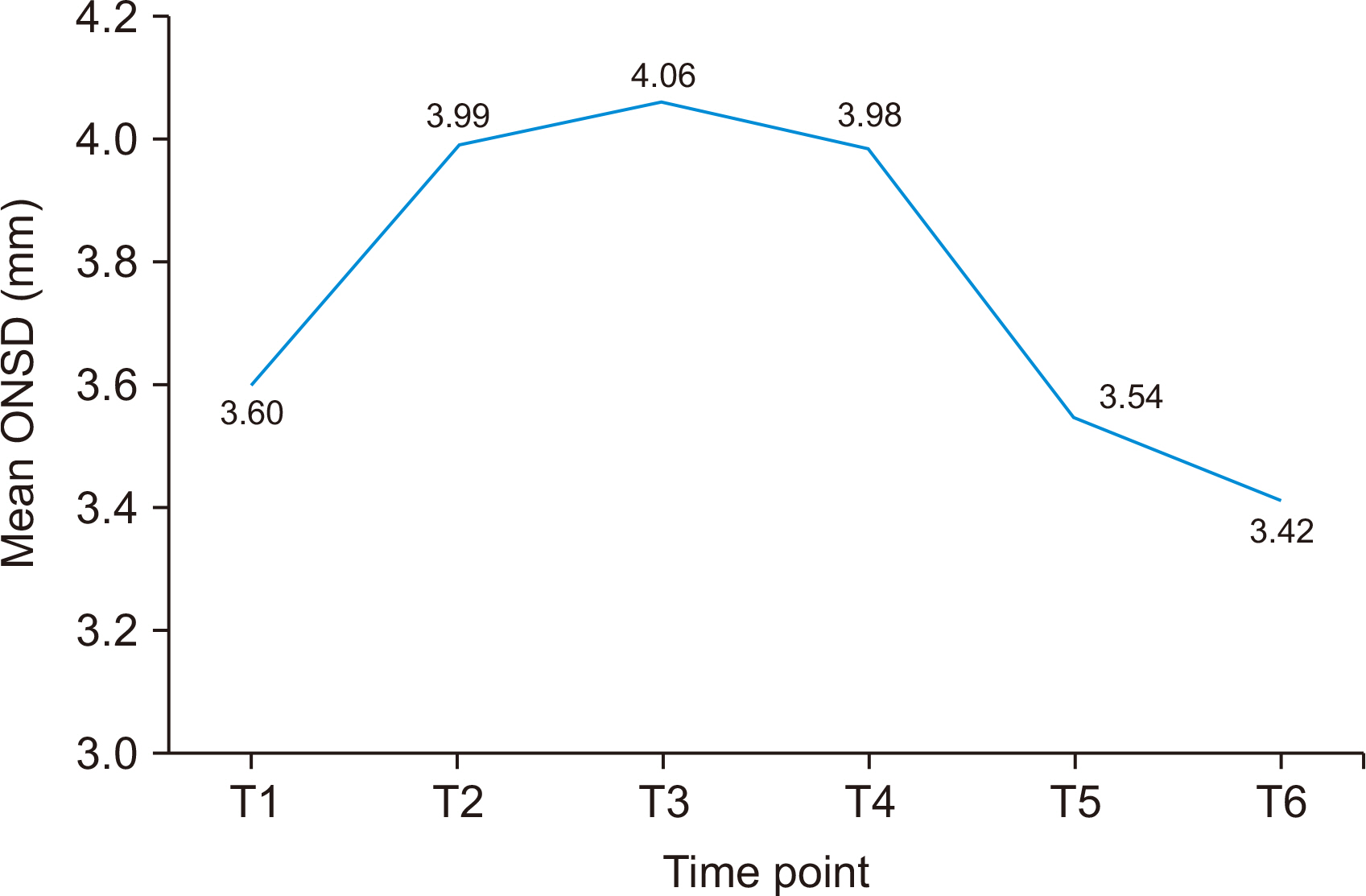
ONSD (in mm) increased from T1 (3.60±0.44) to T3 (4.06±0.45, P=0.002) and T4 (3.99±0.62, P=0.046), before falling to its lowest value at T6 (3.42±0.64, P=0.002). Pearson correlation analysis revealed significant correlations (P<0.05) between changes in ONSD at T3 and both DBP (r=0.637) and MAP (r=0.522).
Conclusions
During RAKT with open ureteric anastomosis, ONSD initially increased, then decreased following reperfusion. DBP and MAP displayed positive correlations with ONSD changes at T3.
Keyword
Figure
Reference
-
1. Whiteley JR, Taylor J, Henry M, Epperson TI, Hand WR. 2015; Detection of elevated intracranial pressure in robot-assisted laparoscopic radical prostatectomy using ultrasonography of optic nerve sheath diameter. J Neurosurg Anesthesiol. 27:155–9. DOI: 10.1097/ANA.0000000000000106. PMID: 25105824.
Article2. Stern-Nezer S. 2021; Chronic and end-stage kidney disease in the neurological intensive care unit. J Stroke Cerebrovasc Dis. 30:105819. DOI: 10.1016/j.jstrokecerebrovasdis.2021.105819. PMID: 33926796.
Article3. Kong X, Wen JQ, Qi RF, Luo S, Zhong JH, Chen HJ, et al. 2014; Diffuse interstitial brain edema in patients with end-stage renal disease undergoing hemodialysis: a tract-based spatial statistics study. Medicine (Baltimore). 93:e313. DOI: 10.1097/MD.0000000000000313. PMID: 25526483. PMCID: PMC4603090.4. Wagener G, Bezinover D, Wang C, Kroepfl E, Diaz G, Giordano C, et al. 2021; Fluid management during kidney transplantation: a consensus statement of the committee on transplant anesthesia of the American Society of Anesthesiologists. Transplantation. 105:1677–84. DOI: 10.1097/TP.0000000000003581. PMID: 33323765.5. Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. 2011; Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit Care. 15:506–15. DOI: 10.1007/s12028-011-9606-8. PMID: 21769456.6. Kim MS, Bai SJ, Lee JR, Choi YD, Kim YJ, Choi SH. 2014; Increase in intracranial pressure during carbon dioxide pneumoperitoneum with steep Trendelenburg positioning proven by ultrasonographic measurement of optic nerve sheath diameter. J Endourol. 28:801–6. DOI: 10.1089/end.2014.0019. PMID: 24517270.
Article7. Robba C, Cardim D, Donnelly J, Bertuccio A, Bacigaluppi S, Bragazzi N, et al. 2016; Effects of pneumoperitoneum and Trendelenburg position on intracranial pressure assessed using different non-invasive methods. Br J Anaesth. 117:783–91. DOI: 10.1093/bja/aew356. PMID: 27956677.
Article8. Kamine TH, Papavassiliou E, Schneider BE. 2014; Effect of abdominal insufflation for laparoscopy on intracranial pressure. JAMA Surg. 149:380–2. DOI: 10.1001/jamasurg.2013.3024. PMID: 24522521.
Article9. Schaier M, Wolf RC, Kubera K, Nagel S, Bartsch A, Zeier M, et al. 2021; Vasogenic brain edema during maintenance hemodialysis: preliminary results from tract-based spatial statistics and voxel-based morphometry. Clin Neuroradiol. 31:217–24. DOI: 10.1007/s00062-019-00865-2. PMID: 31848644.
Article10. Ahmed US, Bacaj P, Iqbal HI, Onder S. 2016; IgA Nephropathy in a patient presenting with pseudotumor cerebri. Case Rep Nephrol. 2016:5273207. DOI: 10.1155/2016/5273207. PMID: 26989531. PMCID: PMC4771878.
Article11. Choi B, Crouzet C, Lau WL, Cribbs DH, Fisher MJ. 2021; Cerebral blood flow in chronic kidney disease. J Stroke Cerebrovasc Dis. 30:105702. DOI: 10.1016/j.jstrokecerebrovasdis.2021.105702. PMID: 33714675. PMCID: PMC8384649.
Article12. Arnold R, Issar T, Krishnan AV, Pussell BA. Neurological complications in chronic kidney disease. JRSM Cardiovasc Dis. 2016; 5:DOI: 10.1177/2048004016677687. PMID: 27867500. PMCID: PMC5102165.
Article13. Nehring SM, Tadi P, Tenny S. Cerebral Edema. StatPearls Treasure Island;2023.14. Weber ED, Colyer MH, Lesser RL, Subramanian PS. 2007; Posterior ischemic optic neuropathy after minimally invasive prostatectomy. J Neuroophthalmol. 27:285–7. DOI: 10.1097/WNO.0b013e31815b9f67. PMID: 18090562.
Article15. Lee LA, Posner KL, Bruchas R, Roth S, Domino KB. Visual loss after prostatectomy. In : Proceedings of the 2010 Annual Meeting of the American Society Anesthesiologists; 2010 Oct 16-20; San Diego, CA, USA [abstract].16. Pandey R, Garg R, Darlong V, Punj J, Chandralekha , Kumar A. 2010; Unpredicted neurological complications after robotic laparoscopic radical cystectomy and ileal conduit formation in steep trendelenburg position: two case reports. Acta Anaesthesiol Belg. 61:163–6. PMID: 21268573.17. Rajmohan N, Omkarappa S, Srinivasan SP, Nair SG, Rajgopal R, Eldo N. 2022; Anesthetic challenges and perioperative factors affecting delayed graft function in robotic-assisted kidney transplant: a review of a single-center experience of 100 cases. Cureus. 14:e28957. DOI: 10.7759/cureus.28957. PMID: 36237794. PMCID: PMC9547721.
Article18. Snoeijs MG, Wiermans B, Christiaans MH, van Hooff JP, Timmerman BE, Schurink GW, et al. 2007; Recipient hemodynamics during non-heart-beating donor kidney transplantation are major predictors of primary nonfunction. Am J Transplant. 7:1158–66. DOI: 10.1111/j.1600-6143.2007.01744.x. PMID: 17331108.
Article19. Campos L, Parada B, Furriel F, Castelo D, Moreira P, Mota A. 2012; Do intraoperative hemodynamic factors of the recipient influence renal graft function? Transplant Proc. 44:1800–3. DOI: 10.1016/j.transproceed.2012.05.042. PMID: 22841277.
Article20. Parikh BK, Shah VR, Modi PR, Butala BP, Parikh GP. 2013; Anaesthesia for laparoscopic kidney transplantation: influence of Trendelenburg position and CO2 pneumoperitoneum on cardiovascular, respiratory and renal function. Indian J Anaesth. 57:253–8. DOI: 10.4103/0019-5049.115607. PMID: 23983283. PMCID: PMC3748679.
Article21. Blecha S, Harth M, Schlachetzki F, Zeman F, Blecha C, Flora P, et al. 2017; Changes in intraocular pressure and optic nerve sheath diameter in patients undergoing robotic-assisted laparoscopic prostatectomy in steep 45° Trendelenburg position. BMC Anesthesiol. 17:40. DOI: 10.1186/s12871-017-0333-3. PMID: 28284189. PMCID: PMC5351936.
Article22. Balkan B, Emir NS, Demirayak B, Çetingök H, Bayrak B. 2021; The effect of robotic surgery on intraocular pressure and optic nerve sheath diameter: a prospective study. Braz J Anesthesiol. 71:607–11. DOI: 10.1016/j.bjane.2021.02.035. PMID: 33762188. PMCID: PMC9373701.23. Jun IJ, Kim M, Lee J, Park SU, Hwang JH, Hong JH, et al. 2018; Effect of mannitol on ultrasonographically measured optic nerve sheath diameter as a surrogate for intracranial pressure during robot-assisted laparoscopic prostatectomy with pneumoperitoneum and the Trendelenburg position. J Endourol. 32:608–13. DOI: 10.1089/end.2017.0828. PMID: 29415565.
Article24. Launey Y, Nesseler N, Le Maguet P, Mallédant Y, Seguin P. 2014; Effect of osmotherapy on optic nerve sheath diameter in patients with increased intracranial pressure. J Neurotrauma. 31:984–8. DOI: 10.1089/neu.2012.2829. PMID: 24372319.25. Sujata N, Tobin R, Mehta P, Girotra G. 2019; Optic nerve sheath diameter-guided extubation plan in obese patients undergoing robotic pelvic surgery in steep Trendelenburg position: a report of three cases. Indian J Anaesth. 63:138–41. DOI: 10.4103/ija.IJA_88_19. PMID: 30814752. PMCID: PMC6383485.
Article26. Maeda S, Tomoyasu Y, Higuchi H, Ishii-Maruhama M, Egusa M, Miyawaki T. 2015; Independent predictors of delay in emergence from general anesthesia. Anesth Prog. 62:8–13. DOI: 10.2344/0003-3006-62.1.8. PMID: 25849468. PMCID: PMC4389560.
Article27. Singh Shah D, Shrestha M, Khatri B, Chhetri S, Shrestha K, Sedhai S, et al. 2023; Equity in transplantation access in Nepal: an analysis of gender, geographic, and caste-based disparities in transplants. Transpl Int. 36:11635. DOI: 10.3389/ti.2023.11635. PMID: 38099085. PMCID: PMC10719117.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the effects of normal and low blood pressure regulation on the optic nerve sheath diameter in robot assisted laparoscopic radical prostatectomy
- Optic Nerve Sheath Meningocele with Optic Disc Pit
- Visualizing kidney transplant techniques: a comparative study of open and robotic surgery
- Robotic assisted adrenalectomy: Is it ready for prime time?
- End-stage renal failure in 124 children: analysis of etiology, age and interal from early renal failure to the end stage