Ann Surg Treat Res.
2024 Jul;107(1):42-49. 10.4174/astr.2024.107.1.42.
Comparing extracorporeal, semi-extracorporeal, and intracorporeal anastomosis in laparoscopic right hemicolectomy: introducing a bridging technique for colorectal surgeons
- Affiliations
-
- 1Division of Colorectal Surgery, Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Division of Colorectal Surgery, Department of Surgery, CHA Bundang Medical Center, CHA University College of Medicine, Seongnam, Korea
- KMID: 2557579
- DOI: http://doi.org/10.4174/astr.2024.107.1.42
Abstract
- Purpose
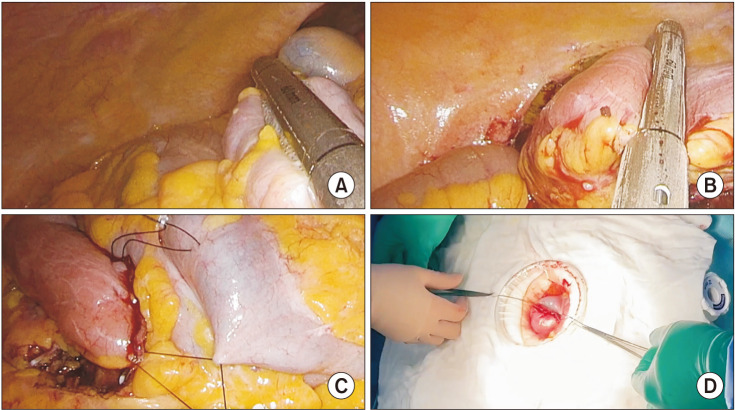
Intracorporeal anastomosis (IA) in laparoscopic right hemicolectomy has been associated with faster recovery in bowel function compared to extracorporeal anastomosis (EA). However, the technical difficulty of laparoscopic suturing technique and intraabdominal fecal contamination hinder many surgeons from implementing such a procedure. We introduce and compare a bridging technique designated as “semi-extracorporeal” anastomosis (SEA), which embraces the advantages and amends the drawbacks of IA and EA.
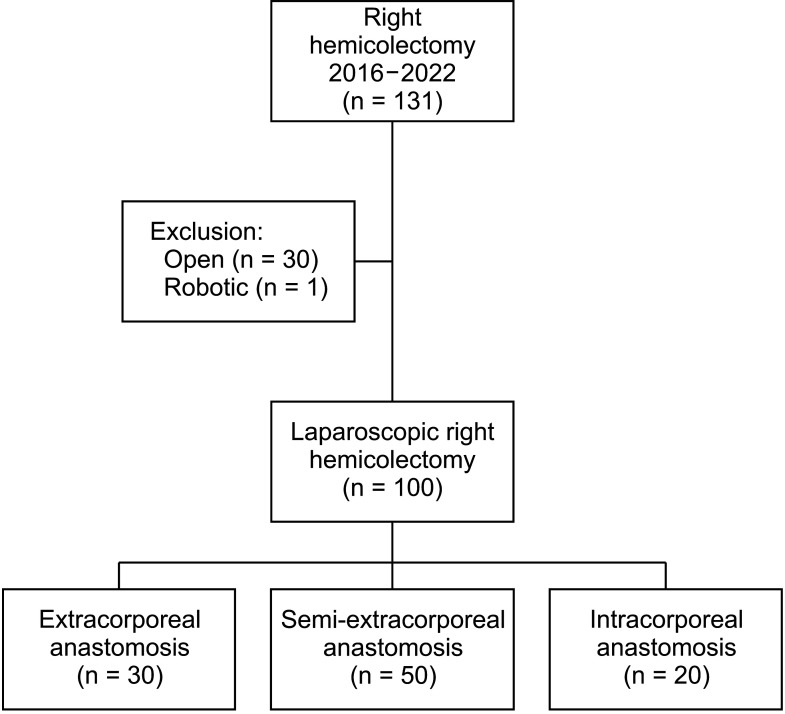
Methods
Between May 2016 and October 2022, 100 patients who underwent laparoscopic right hemicolectomy were analyzed. All patients who received laparoscopic right hemicolectomy underwent one of the 3 anastomosis methods (EA, SEA, and IA) by a single colorectal surgeon at a single tertiary care hospital. Data including perioperative parameters and postoperative outcomes were analyzed by each group.
Results
A total of 100 patients were reviewed. Thirty patients underwent EA; 50 and 20 patients underwent SEA and IA, respectively. Operation time (minute) was 170 (range, 100–285), 170 (range, 110–280), and 147.5 (range, 80–235) in EA, SEA, and IA, respectively (P = 0.010). Wound size was smaller in SEA and IA compared to EA (P < 0.001). IA was associated with a shorter time (day) to first flatus compared to SEA and EA (4 [range, 2–13] vs. 4 [range, 2–7] vs. 2.5 [range, 1–4], P < 0.001). Postoperative complication showed no statistical significance between the 3 groups.
Conclusion
Semi-extracorporeal was an attractive bridging option for colorectal surgeons worrisome of the technical difficulty of IA while maintaining faster bowel recovery and smaller wound incisions compared to EA.
Keyword
Figure
Reference
-
1. Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991; 1:144–150. PMID: 1688289.2. Lechaux D. Intra-corporeal anastomosis in laparoscopic right hemicolectomy. J Chir (Paris). 2005; 142:102–104. PMID: 15976634.3. Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg. 2008; 143:762–768. PMID: 18711036.4. Allaix ME, Degiuli M, Bonino MA, Arezzo A, Mistrangelo M, Passera R, et al. Intracorporeal or extracorporeal ileocolic anastomosis after laparoscopic right colectomy: a double-blinded randomized controlled trial. Ann Surg. 2019; 270:762–767. PMID: 31592811.5. Bollo J, Turrado V, Rabal A, Carrillo E, Gich I, Martinez MC, et al. Randomized clinical trial of intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy (IEA trial). Br J Surg. 2020; 107:364–372. PMID: 31846067.6. Ricci C, Casadei R, Alagna V, Zani E, Taffurelli G, Pacilio CA, et al. A critical and comprehensive systematic review and meta-analysis of studies comparing intracorporeal and extracorporeal anastomosis in laparoscopic right hemicolectomy. Langenbecks Arch Surg. 2017; 402:417–427. PMID: 27595589.7. van Oostendorp S, Elfrink A, Borstlap W, Schoonmade L, Sietses C, Meijerink J, et al. Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc. 2017; 31:64–77. PMID: 27287905.8. Lowson D. Resection of the caecum, greater part of ascending colon and five inches of ileum for malignant disease of ascending colon. Lancet. 1893; 141:648–649.9. Matsuda T, Yamashita K, Hasegawa H, Utsumi M, Kakeji Y. Current status and trend of laparoscopic right hemicolectomy for colon cancer. Ann Gastroenterol Surg. 2020; 4:521–527. PMID: 33005847.10. Colon Cancer Laparoscopic or Open Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009; 10:44–52. PMID: 19071061.11. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005; 365:1718–1726. PMID: 15894098.12. Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007; 25:3061–3068. PMID: 17634484.13. Arezzo A, Passera R, Ferri V, Gonella F, Cirocchi R, Morino M. Laparoscopic right colectomy reduces short-term mortality and morbidity: results of a systematic review and meta-analysis. Int J Colorectal Dis. 2015; 30:1457–1472. PMID: 26137968.14. Athanasiou CD, Markides GA, Kotb A, Jia X, Gonsalves S, Miskovic D. Open compared with laparoscopic complete mesocolic excision with central lymphadenectomy for colon cancer: a systematic review and meta-analysis. Colorectal Dis. 2016; 18:O224–O235. PMID: 27187520.15. Widmar M, Keskin M, Strombom P, Beltran P, Chow OS, Smith JJ, et al. Lymph node yield in right colectomy for cancer: a comparison of open, laparoscopic and robotic approaches. Colorectal Dis. 2017; 19:888–894. PMID: 28649796.16. Corman M. Colon and rectal surgery. 6th ed. Lippincott Williams & Wilkins;2012.17. Ravitch MM, Brown IW, Daviglus GF. Experimental and clinical use of the Soviet bronchus stapling instrument. Surgery. 1959; 46:97–108. PMID: 13668819.18. Alves A, Panis Y, Trancart D, Regimbeau JM, Pocard M, Valleur P. Factors associated with clinically significant anastomotic leakage after large bowel resection: multivariate analysis of 707 patients. World J Surg. 2002; 26:499–502. PMID: 11910487.19. Isbister WH. Anastomotic leak in colorectal surgery: a single surgeon’s experience. ANZ J Surg. 2001; 71:516–520. PMID: 11527260.20. Lipska MA, Bissett IP, Parry BR, Merrie AE. Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg. 2006; 76:579–585. PMID: 16813622.21. Lustosa SA, Matos D, Atallah AN, Castro AA. Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev. 2001; (3):CD003144. PMID: 11687041.22. MacRae HM, McLeod RS. Handsewn vs. stapled anastomoses in colon and rectal surgery: a meta-analysis. Dis Colon Rectum. 1998; 41:180–189. PMID: 9556242.23. Choy PY, Bissett IP, Docherty JG, Parry BR, Merrie A, Fitzgerald A. Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev. 2011; (9):CD004320. PMID: 21901690.24. Emile SH, Elfeki H, Shalaby M, Sakr A, Bassuni M, Christensen P, et al. Intracorporeal versus extracorporeal anastomosis in minimally invasive right colectomy: an updated systematic review and meta-analysis. Tech Coloproctol. 2019; 23:1023–1035. PMID: 31646396.25. Feo CF, Feo CV, Fancellu A, Ginesu GC, Cherchi G, Zese M, et al. Laparoscopic versus open transverse-incision right hemicolectomy: a retrospective comparison study. ANZ J Surg. 2019; 89:E292–E296. PMID: 31066197.26. Hellan M, Anderson C, Pigazzi A. Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. JSLS. 2009; 13:312–317. PMID: 19793468.27. Frigault J, Avoine S, Drolet S, Letarte F, Bouchard A, Gagné JP, et al. Intracorporeal versus extracorporeal anastomosis in laparoscopic right hemicolectomy: a retrospective cohort study of anastomotic complications. Ann Coloproctol. 2023; 39:147–155. PMID: 35345307.28. Kim Y, Choi S, Jeong S, Lee S, Kang I, Jang J. Risk factors of incisional hernia after single-incision cholecystectomy and safety of barbed suture material for wound closure. J Minim Invasive Surg. 2021; 24:145–151. PMID: 35600106.29. Lam TJ, Udonwa SA, Yaow CY, Nistala KR, Chong CS. Intracorporeal versus extracorporeal anastomosis in laparoscopic colectomy: a meta-analysis and systematic review. Curr Colorectal Cancer Rep. 2022; 18:1–17.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes of intracorporeal versus extracorporeal anastomosis in laparoscopic colectomy surgery
- Intracorporeal versus extracorporeal anastomosis in laparoscopic right hemicolectomy: a retrospective cohort study of anastomotic complications
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Extracorporeal versus intracorporeal anastomosis for right colon cancer surgery
- Comparison of Intracorporeal Reconstruction after Laparoscopic Distal Gastrectomy with Extracorporeal Reconstruction in the View of Learning Curve