J Gastric Cancer.
2013 Mar;13(1):34-43.
Comparison of Intracorporeal Reconstruction after Laparoscopic Distal Gastrectomy with Extracorporeal Reconstruction in the View of Learning Curve
- Affiliations
-
- 1Department of Surgery, Ajou University School of Medicine, Suwon, Korea. hansu@ajou.ac.kr
Abstract
- PURPOSE
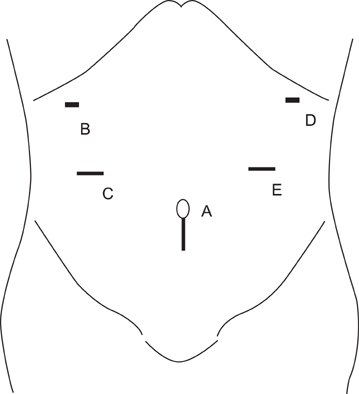
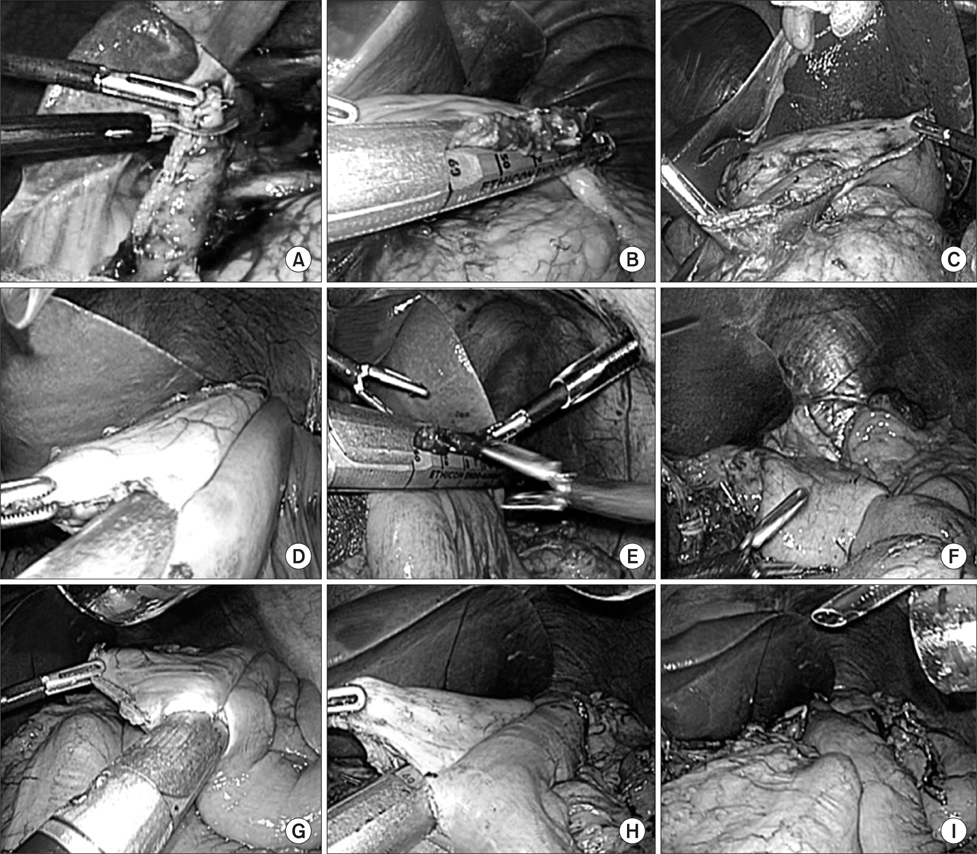
The intracorporeal reconstruction after laparoscopic gastrectomy can minimize postoperative pain, and give better cosmetic effect, while it may have technical difficulties and require the learning curve. This study aimed to analyze the surgical outcome of intracorporeal reconstruction according to the surgeon's experience comparing with extracorporeal procedure.
MATERIALS AND METHODS
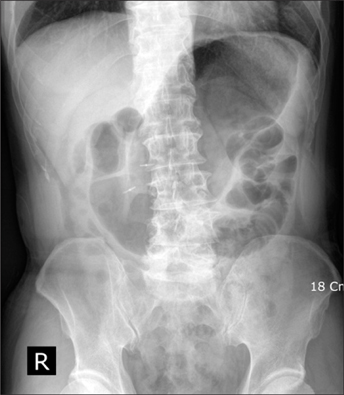
From January 2009 to September 2011, intracorporeal reconstruction in laparoscopic surgery for gastric cancer was performed for 71 patients (Intra group). During same period, 231 patients underwent laparoscopy-assisted gastrectomy (Extra group). These patients were classified into initial (1st to 20th case of intra group), intermediate (21th to 46th case), and experienced (after 47th case) phases.
RESULTS
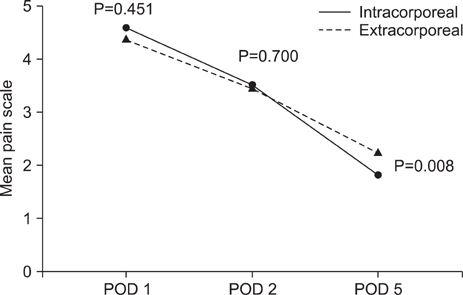
Intracorporeal procedures included 35 cases of Billroth-I, 30 Billroth-II and 6 Roux en Y reconstructions. In the initial phase, operation time (P=0.022) were significantly longer for the patients of intra group than them of extra group. Although the difference was not significant, the length of hospital stay was longer and complication rate was higher in the intra group. In intermediate and experienced phases, there was no difference between two groups in operation time and hospital stay. In these phases, complication rate was lower in the intra group than the extra group (3.9% versus 9.7%). The pain scale was significantly lower post operation day 5 in the intra group.
CONCLUSIONS
Intracorporeal reconstruction after laparoscopic distal gastrectomy was feasible and safe, and the technique was stabilized after 20th case if the surgeon has sufficient experiences when we compared it with extracorporeal reconstruction.
Keyword
MeSH Terms
Figure
Reference
-
1. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994. 4:146–148.2. Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002. 131:1 Suppl. S306–S311.
Article3. Kim MC, Kim KH, Kim HH, Jung GJ. Comparison of laparoscopy-assisted by conventional open distal gastrectomy and extraperigastric lymph node dissection in early gastric cancer. J Surg Oncol. 2005. 91:90–94.
Article4. Hosono S, Arimoto Y, Ohtani H, Kanamiya Y. Meta-analysis of short-term outcomes after laparoscopy-assisted distal gastrectomy. World J Gastroenterol. 2006. 12:7676–7683.
Article5. Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N. Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007. 245:68–72.
Article6. Kim HI, Woo Y, Hyung WJ. Laparoscopic distal gastrectomy with an intracorporeal gastroduodenostomy using a circular stapler. J Am Coll Surg. 2012. 214:e7–e13.
Article7. Kim JJ, Kim SK, Jun KH, Kang HC, Song KY, Chin HM, et al. Clinical usefulness of a totally laparoscopic gastrectomy. J Korean Gastric Cancer Assoc. 2007. 7:132–138.
Article8. Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N, Taomoto J, Masuda T, et al. Advantages of totally laparoscopic distal gastrectomy over laparoscopically assisted distal gastrectomy for gastric cancer. Surg Endosc. 2009. 23:2374–2379.
Article9. Kim JJ, Song KY, Chin HM, Kim W, Jeon HM, Park CH, et al. Totally laparoscopic gastrectomy with various types of intracorporeal anastomosis using laparoscopic linear staplers: preliminary experience. Surg Endosc. 2008. 22:436–442.
Article10. Oh DK, Hur H, Kim JY, Han SU, Cho YK. V-shaped liver retraction during a laparoscopic gastrectomy for gastric cancer. J Gastric Cancer. 2010. 10:133–136.
Article11. Song HM, Lee SL, Hur H, Cho YK, Han SU. Linear-shaped gastroduodenostomy in totally laparoscopic distal gastrectomy. J Gastric Cancer. 2010. 10:69–74.
Article12. Tanimura S, Higashino M, Fukunaga Y, Kishida S, Nishikawa M, Ogata A, et al. Laparoscopic distal gastrectomy with regional lymph node dissection for gastric cancer. Surg Endosc. 2005. 19:1177–1181.
Article13. Kim HH. Laparoscopic Billroth-II gastrectomy for benign gastric disease. Korean Soc Endosc Laparosc Surg. 1999. 2:11–18.14. Korean Laparoscopic Gastrointestinal Surgery Study Group. Nationwide survey of laparoscopic gastric surgery in Korea, 2004. J Korean Gastric Cancer Assoc. 2005. 5:295–303.15. Jin SH, Kim DY, Kim H, Jeong IH, Kim MW, Cho YK, et al. Multidimensional learning curve in laparoscopy-assisted gastrectomy for early gastric cancer. Surg Endosc. 2007. 21:28–33.
Article16. Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol. 2005. 11:7508–7511.
Article17. Kunisaki C, Makino H, Yamamoto N, Sato T, Oshima T, Nagano Y, et al. Learning curve for laparoscopy-assisted distal gastrectomy with regional lymph node dissection for early gastric cancer. Surg Laparosc Endosc Percutan Tech. 2008. 18:236–241.
Article18. Kim KC, Yook JH, Choi JE, Cheong O, Lim JT, Oh ST, et al. The learning curve of laparoscopy-assisted distal gastrectomy (LADG) for cancer. J Korean Gastric Cancer Assoc. 2008. 8:232–236.
Article19. Yoo CH, Kim HO, Hwang SI, Son BH, Shin JH, Kim H. Short-term outcomes of laparoscopic-assisted distal gastrectomy for gastric cancer during a surgeon's learning curve period. Surg Endosc. 2009. 23:2250–2257.
Article20. Kojima K, Yamada H, Inokuchi M, Kawano T, Sugihara K. A comparison of Roux-en-Y and Billroth-I reconstruction after laparoscopy-assisted distal gastrectomy. Ann Surg. 2008. 247:962–967.
Article21. Kinoshita T, Shibasaki H, Oshiro T, Ooshiro M, Okazumi S, Katoh R. Comparison of laparoscopy-assisted and total laparoscopic Billroth-I gastrectomy for gastric cancer: a report of short-term outcomes. Surg Endosc. 2011. 25:1395–1401.
Article22. Hyung WJ, Lim JS, Cheong JH, Kim J, Choi SH, Song SY, et al. Intraoperative tumor localization using laparoscopic ultrasonography in laparoscopic-assisted gastrectomy. Surg Endosc. 2005. 19:1353–1357.
Article23. Chan DC, Fan YM, Lin CK, Chen CJ, Chen CY, Chao YC. Roux-en-Y reconstruction after distal gastrectomy to reduce enterogastric reflux and Helicobacter pylori infection. J Gastrointest Surg. 2007. 11:1732–1740.
Article24. Fukuhara K, Osugi H, Takada N, Takemura M, Higashino M, Kinoshita H. Reconstructive procedure after distal gastrectomy for gastric cancer that best prevents duodenogastroesophageal reflux. World J Surg. 2002. 26:1452–1457.
Article25. Sah BK, Zhu ZG, Chen MM, Xiang M, Chen J, Yan M, et al. Effect of surgical work volume on postoperative complication: superiority of specialized center in gastric cancer treatment. Langenbecks Arch Surg. 2009. 394:41–47.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Totally Laparoscopic Roux-en-Y Gastrojejunostomy after Laparoscopic Distal Gastrectomy: Analysis of Initial 50 Consecutive Cases of Single Surgeon in Comparison with Totally Laparoscopic Billroth I Reconstruction
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Totally Laparoscopic Distal Gastrectomy after Learning Curve Completion: Comparison with Laparoscopy-Assisted Distal Gastrectomy
- Comparison of laparoscopy-assisted and totally laparoscopic Billroth-II distal gastrectomy for gastric cancer
- Solo Intracorporeal Esophagojejunostomy Reconstruction Using a Laparoscopic Scope Holder in Single-Port Laparoscopic Total Gastrectomy for Early Gastric Cancer