Ann Surg Treat Res.
2024 Jul;107(1):16-26. 10.4174/astr.2024.107.1.16.
A personalized prognostic model for long-term survival in patients with intrahepatic cholangiocarcinoma: a retrospective cohort study
- Affiliations
-
- 1Center for Pre-Disease Treatment and Health Management, Affiliated Hospital of Hangzhou Normal University, Hangzhou Normal University, Hangzhou, China
- 2Hangzhou Normal University, Hangzhou, China
- KMID: 2557576
- DOI: http://doi.org/10.4174/astr.2024.107.1.16
Abstract
- Purpose
This study aimed to determine the optimal cutoff points for age and tumor size of patients with intrahepatic cholangiocarcinoma (ICC) and to establish and verify a predictive nomogram of overall survival at 1, 3, and 5 years.
Methods
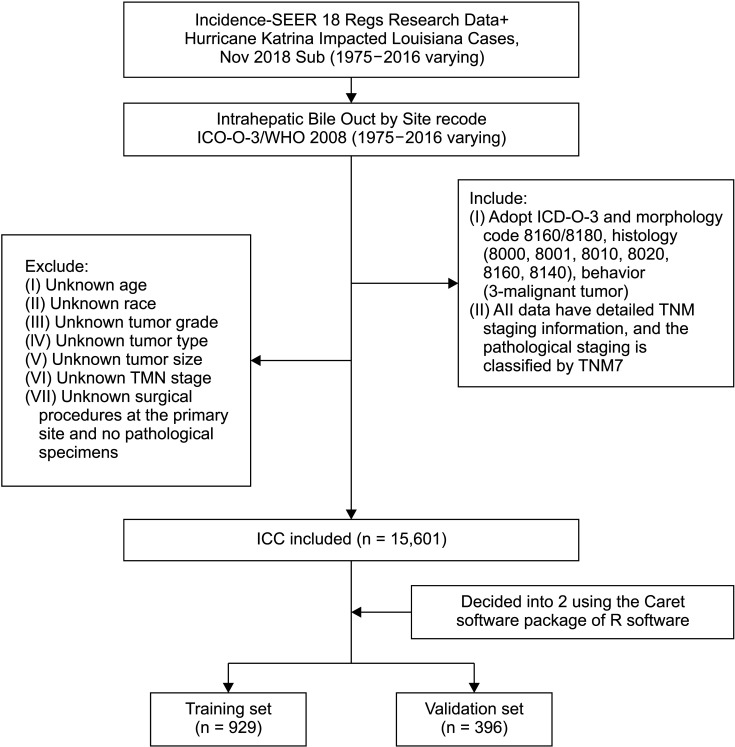
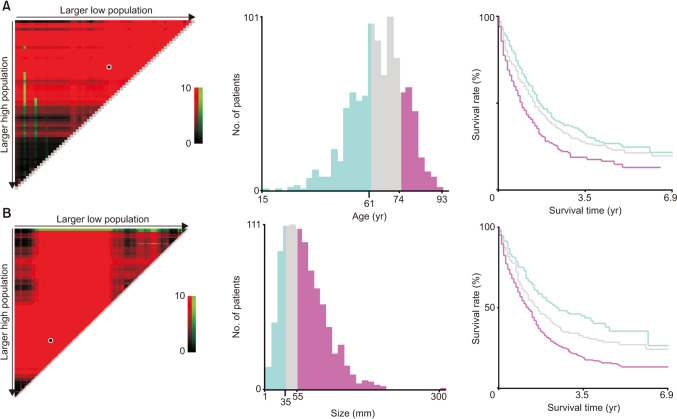
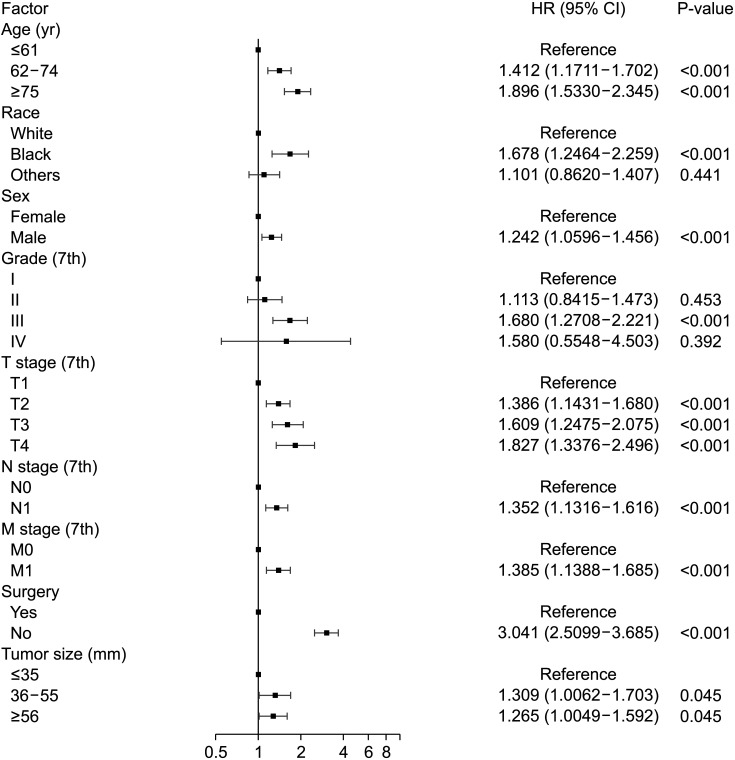
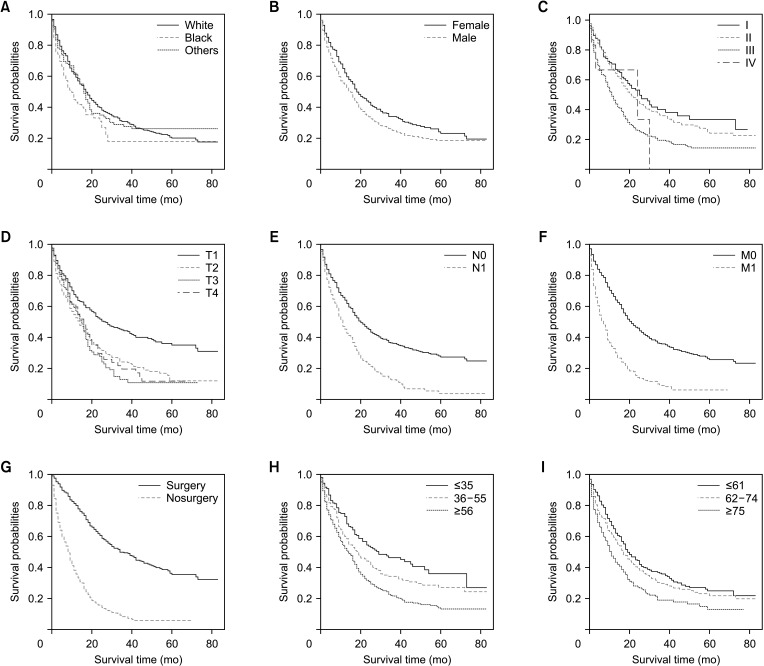
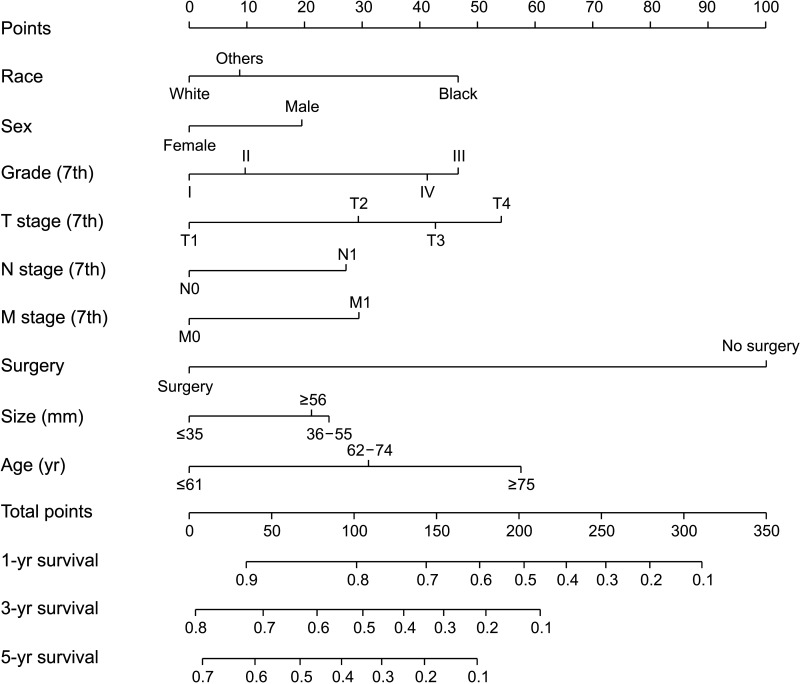
From the SEER (Surveillance, Epidemiology, and End Results) database, 1,325 ICC patients were selected and randomly divided into training and testing cohorts at a 7:3 ratio. Using the X-tile software, age and tumor size were classified into 3 subgroups: ≤61, 62–74, and ≥75 years and ≤35, 36–55, and ≥56 mm. Subsequently, univariate and multivariate Cox regression analyses were performed using the R software in the training cohort to determine independent risk factors, compile the prediction nomogram, and verify it with the testing cohort findings.
Results
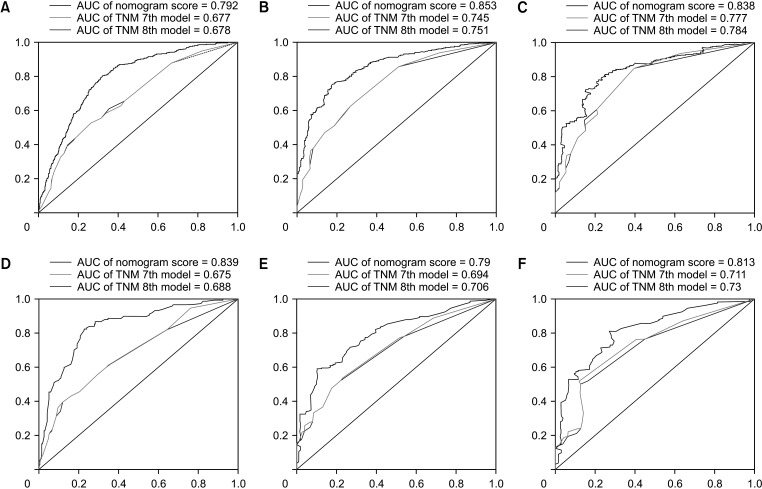
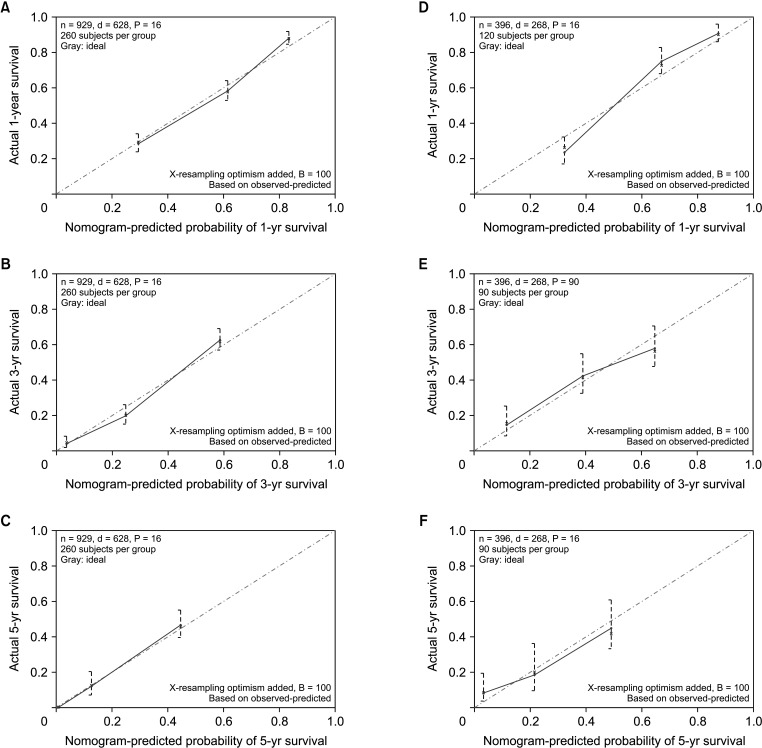
The C-indexes of the new prediction nomograms in the training and testing cohorts were 0.738 (95% confidence interval [CI], 0.718–0.758) and 0.750 (95% CI, 0.72–0.78), respectively. Furthermore, the areas under the 1-, 3-, and 5-year receiver operating characteristic (ROC) curves based on the nomogram were 0.792, 0.853, and 0.838, respectively, higher than the ROC based on the 7th and 8th editions of the American Joint Cancer Commission (AJCC) staging system.
Conclusion
This study established and verified a prognostic nomogram that improved the accuracy of the 1-, 3-, and 5-year survival predictions for ICC patients, compared with that based on the 7th and 8th editions of the AJCC staging system, and can help clinicians make personalized survival predictions.
Keyword
Figure
Reference
-
1. Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014; 60:1268–1289. PMID: 24681130.2. El-Diwany R, Pawlik TM, Ejaz A. Intrahepatic cholangiocarcinoma. Surg Oncol Clin N Am. 2019; 28:587–599. PMID: 31472907.3. Moris D, Palta M, Kim C, Allen PJ, Morse MA, Lidsky ME. Advances in the treatment of intrahepatic cholangiocarcinoma: an overview of the current and future therapeutic landscape for clinicians. CA Cancer J Clin. 2023; 73:198–222. PMID: 36260350.4. Mazzaferro V, Gorgen A, Roayaie S, Droz Dit Busset M, Sapisochin G. Liver resection and transplantation for intrahepatic cholangiocarcinoma. J Hepatol. 2020; 72:364–377. PMID: 31954498.5. Ma CH, Hwang DW, Song KB, Kim SC, Shin SH, Lee JH. Prognostic factors predicting survival rate over 10 years of patients with intrahepatic cholangiocarcinoma after hepatic resection. Ann Surg Treat Res. 2020; 98:116–123. PMID: 32158731.6. Sohn HJ, Kim H, Kim JR, Kang JS, Han Y, Lee M, et al. Predicting prognosis and evaluating the benefits of adjuvant chemotherapy depending on the tumor location in intrahepatic cholangiocarcinoma: focusing on the involvement of below 2nd bile duct confluence. Ann Surg Treat Res. 2022; 102:248–256. PMID: 35611087.7. Vitale A, Spolverato G, Bagante F, Gani F, Popescu I, Marques HP, et al. A multi-institutional analysis of elderly patients undergoing a liver resection for intrahepatic cholangiocarcinoma. J Surg Oncol. 2016; 113:420–426. PMID: 27100027.8. Phan K, An VV, Ha H, Phan S, Lam V, Pleass H. Hepatic resection for malignant liver tumours in the elderly: a systematic review and meta-analysis. ANZ J Surg. 2015; 85:815–822. PMID: 26073054.9. van Keulen AM, Büttner S, Erdmann JI, Hagendoorn J, Hoogwater FJ, IJzermans JN, et al. Major complications and mortality after resection of intrahepatic cholangiocarcinoma: a systematic review and meta-analysis. Surgery. 2023; 173:973–982. PMID: 36577599.10. Chinchilla-López P, Aguilar-Olivos NE, García-Gómez J, Hernández-Alejandro KK, Chablé-Montero F, Motola-Kuba D, et al. Prevalence, risk factors, and survival of patients with intrahepatic cholangiocarcinoma. Ann Hepatol. 2017; 16:565–568. PMID: 28611259.11. Raoof M, Dumitra S, Ituarte PH, Melstrom L, Warner SG, Fong Y, et al. Development and validation of a prognostic score for intrahepatic cholangiocarcinoma. JAMA Surg. 2017; 152:e170117. PMID: 28297009.12. Liu J, Zhong M, Feng Y, Zeng S, Wang Y, Xu H, et al. Prognostic factors and treatment strategies for intrahepatic cholangiocarcinoma from 2004 to 2013: population-based SEER analysis. Transl Oncol. 2019; 12:1496–1503. PMID: 31446308.13. Nathan H, Aloia TA, Vauthey JN, Abdalla EK, Zhu AX, Schulick RD, et al. A proposed staging system for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2009; 16:14–22. PMID: 18987916.14. Liver Cancer Study Group of Japan. The general rules for the clinical and pathological study of primary liver cancer. Jpn J Surg. 1989; 19:98–129. PMID: 2659865.15. Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017; 67:93–99. PMID: 28094848.16. Li Y, Tang C, Zhao B, Dong F. Redefining the T1 category of the 8th American Joint Committee on Cancer Staging System for intrahepatic cholangiocarcinoma: a SEER database analysis. Oncol Lett. 2020; 19:527–532. PMID: 31897167.17. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008; 26:1364–1370. PMID: 18323559.18. Rocco B, Sighinolfi MC, Sandri M, Puliatti S, Bianchi G. A novel nomogram for predicting ECE of prostate cancer. BJU Int. 2018; 122:916–918. PMID: 30460784.19. Wu J, Zhou Q, Pan Z, Wang Y, Hu L, Chen G, et al. Development and validation of a nomogram for predicting long-term overall survival in nasopharyngeal carcinoma: a population-based study. Medicine (Baltimore). 2020; 99:e18974. PMID: 31977914.20. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A III. AJCC cancer staging manual. 7th ed. Springer;2010.21. Kim Y, Moris DP, Zhang XF, Bagante F, Spolverato G, Schmidt C, et al. Evaluation of the 8th edition American Joint Commission on Cancer (AJCC) staging system for patients with intrahepatic cholangiocarcinoma: a surveillance, epidemiology, and end results (SEER) analysis. J Surg Oncol. 2017; 116:643–650. PMID: 28608424.22. Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004; 10:7252–7259. PMID: 15534099.23. Zhang Y, Wu Z, Wang X, Li C, Chang J, Jiang W, et al. Development and external validation of a nomogram for predicting the effect of tumor size on survival of patients with perihilar cholangiocarcinoma. BMC Cancer. 2020; 20:1044. PMID: 33126868.24. Thomas JA, Kendall BJ, El-Serag HB, Thrift AP, Macdonald GA. Hepatocellular and extrahepatic cancer risk in people with non-alcoholic fatty liver disease. Lancet Gastroenterol Hepatol. 2024; 9:159–169. PMID: 38215780.25. Hyder O, Marques H, Pulitano C, Marsh JW, Alexandrescu S, Bauer TW, et al. A nomogram to predict long-term survival after resection for intrahepatic cholang iocarcinoma: an Eastern and Western experience. JAMA Surg. 2014; 149:432–438. PMID: 24599477.26. Ji GW, Jiao CY, Xu ZG, Li XC, Wang K, Wang XH. Development and validation of a gradient boosting machine to predict prognosis after liver resection for intrahepatic cholangiocarcinoma. BMC Cancer. 2022; 22:258. PMID: 35277130.27. Delva F, Marien E, Fonck M, Rainfray M, Demeaux JL, Moreaud P, et al. Factors influencing general practitioners in the referral of elderly cancer patients. BMC Cancer. 2011; 11:5. PMID: 21211031.28. Kim JH, Cheon YK, Lee TY, Lee SH, Chung H. Effect of age on the prognosis of intrahepatic cholangiocarcinoma. Korean J Intern Med. 2023; 38:39–47. PMID: 36541019.29. Zhu H. Describing treatment patterns for elderly patients with intrahepatic cholangiocarcinoma and predicting outcomes by a prognostic model: a seer based study [dissertation]. Nanjing Medical University;2021.30. Ruzzenente A, Conci S, Viganò L, Ercolani G, Manfreda S, Bagante F, et al. Role of lymph node dissection in small (≤ 3 cm) intrahepatic cholangiocarcinoma. J Gastrointest Surg. 2019; 23:1122–1129. PMID: 30820796.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Review: Analysis of Survival Rate and Prognostic Factors of Intrahepatic Cholangiocarcinoma: 318 Cases in Single Institute
- Natural History and Prognostic Factors of Advanced Cholangiocarcinoma without Surgery, Chemotherapy, or Radiotherapy: A Large-Scale Observational Study
- Prognostic factors predicting survival rate over 10 years of patients with intrahepatic cholangiocarcinoma after hepatic resection
- A Clinical Review for Resected Intrahepatic Cholangiocarcinoma
- Prognostic Factors for Intrahepatic Cholangiocarcinoma Treated with Surgical Resection