Ann Surg Treat Res.
2024 Jul;107(1):1-7. 10.4174/astr.2024.107.1.1.
Treatment for appendicitis in cancer patients on chemotherapy: a retrospective cohort study
- Affiliations
-
- 1Center for Colorectal Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- KMID: 2557574
- DOI: http://doi.org/10.4174/astr.2024.107.1.1
Abstract
- Purpose
Whether to perform surgery or conservatively manage appendicitis in immunosuppressed patients is a concern for clinicians. This study aimed to compare the outcomes of these 2 treatment options for appendicitis in patients with cancer undergoing chemotherapy.
Methods
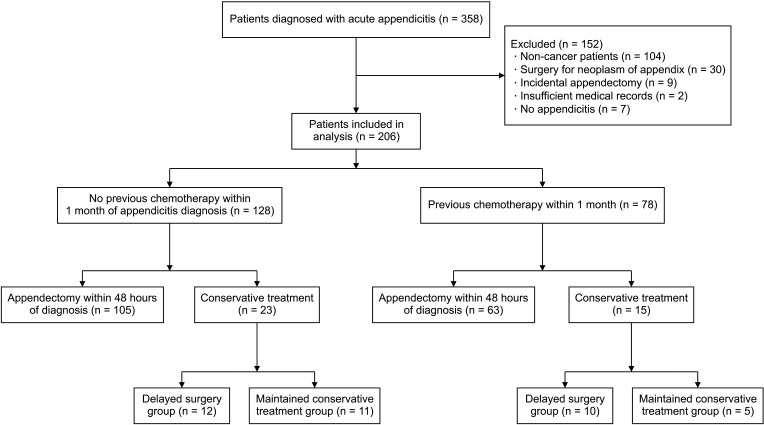
This retrospective study included 206 patients with cancer who were diagnosed with acute appendicitis between August 2001 and December 2021. Among them, patients who received chemotherapy within 1 month were divided into surgical and conservative groups. We evaluated the outcomes, including treatment success within 1 year, 1-year recurrence, and the number of days from the diagnosis of appendicitis to chemotherapy restart, between the 2 groups.
Results
Among the 206 patients with cancer who were diagnosed with acute appendicitis, 78 received chemotherapy within 1 month. The patients were divided into surgery (n = 63) and conservative (n = 15) groups. In the surgery group, the duration of antibiotic therapy (7.0 days vs. 16.0 days, P < 0.001) and length of hospital stay (8.0 days vs. 27.5 days, P = 0.002) were significantly shorter than conservative groups. The duration from the diagnosis of appendicitis to the restart of chemotherapy was shorter in the surgery group (20.8 ± 15.1 days vs. 35.2 ± 28.2 days, P = 0.028). The treatment success rate within 1 year was higher in the surgery group (100% vs. 33.3%, P < 0.001).
Conclusion
Surgical treatment showed a significantly higher success rate than conservative treatment for appendicitis in patients less than 1 month after chemotherapy. Further prospective studies will be needed to clinically determine treatment options.
Keyword
Figure
Reference
-
1. Bucher P, Mathe Z, Demirag A, Morel P. Appendix tumors in the era of laparoscopic appendectomy. Surg Endosc. 2004; 18:1063–1066. PMID: 15156378.2. Mason RJ. Surgery for appendicitis: is it necessary? Surg Infect (Larchmt). 2008; 9:481–488. PMID: 18687030.3. Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC Randomized Clinical Trial. JAMA. 2015; 313:2340–2348. PMID: 26080338.4. Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011; 377:1573–1579. PMID: 21550483.5. Yang HB, Song HB, Han JW, Youn JK, Ko D, Ryu YJ, et al. Clinical course in children with equivocal appendicitis on computed tomography: a retrospective cohort study. Ann Surg Treat Res. 2023; 104:51–59. PMID: 36685769.6. Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995; 82:166–169. PMID: 7749676.7. Hansson J, Körner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009; 96:473–481. PMID: 19358184.8. Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, et al. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006; 30:1033–1037. PMID: 16736333.9. Lang H, Schlitt HJ, Manns MP, Pichlmayr R. Surgery in immunosuppressed patients with emergency or elective indications. Chirurg. 1997; 68:675–680. PMID: 9340231.10. Skibber JM, Matter GJ, Pizzo PA, Lotze MT. Right lower quadrant pain in young patients with leukemia: a surgical perspective. Ann Surg. 1987; 206:711–716. PMID: 3318727.11. Mortellaro VE, Juang D, Fike FB, Saites CG, Potter DD Jr, Iqbal CW, et al. Treatment of appendicitis in neutropenic children. J Surg Res. 2011; 170:14–16. PMID: 21514602.12. Saillard C, Zafrani L, Darmon M, Bisbal M, Chow-Chine L, Sannini A, et al. The prognostic impact of abdominal surgery in cancer patients with neutropenic enterocolitis: a systematic review and meta-analysis, on behalf the Groupe de Recherche en Réanimation Respiratoire du patient d'Onco-Hématologie (GRRR-OH). Ann Intensive Care. 2018; 8:47. PMID: 29675758.13. Jolissaint JS, Harary M, Saadat LV, Madenci AL, Dieffenbach BV, Al Natour RH, et al. Timing and outcomes of abdominal surgery in neutropenic patients. J Gastrointest Surg. 2019; 23:643–650. PMID: 30659440.14. Jeong JH, Jung J, Kim HJ, Lee JW, Ko BS, Son BH, et al. Domestic medical travel from non-Seoul regions to Seoul for initial breast cancer treatment: a nationwide cohort study. Ann Surg Treat Res. 2023; 104:71–79. PMID: 36816739.15. Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-Jones E, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020; 371:m4087. PMID: 33148535.16. Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015; 372:1539–1548. PMID: 25875259.17. Bruniera FR, Ferreira FM, Saviolli LR, Bacci MR, Feder D, da Luz Gonçalves Pedreira M, et al. The use of vancomycin with its therapeutic and adverse effects: a review. Eur Rev Med Pharmacol Sci. 2015; 19:694–700. PMID: 25753888.18. Watkins RR, Deresinski S. Increasing evidence of the nephrotoxicity of piperacillin/tazobactam and vancomycin combination therapy: what is the clinician to do? Clin Infect Dis. 2017; 65:2137–2143. PMID: 29020249.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antibiotic therapy for appendicitis treatment
- Clinical course in children with equivocal appendicitis on computed tomography: a retrospective cohort study
- Ultrasonography Versus MRI for Diagnosing Acute Appendicitis During Pregnancy
- Preoperative Chemotherapy in Advanced Stomach Cancer (Cons)
- The acute appendicitis in elderly-clinical review of the acute appendicitis in the patients over the age of 60