J Rheum Dis.
2024 Jul;31(3):171-177. 10.4078/jrd.2024.0029.
The effectiveness of tumor necrosis factor-α blocker therapy in patients with axial spondyloarthritis who failed conventional treatment: a comparative study focused on improvement in ASAS Health Index
- Affiliations
-
- 1Department of Rheumatology, Chonnam National University Medical School and Hospital, Gwangju, Korea
- 2College of Nursing, Chonnam National University, Gwangju, Korea
- 3Department of Biomedical Sciences, Graduate School of Chonnam National University, Gwangju, Korea
- KMID: 2557405
- DOI: http://doi.org/10.4078/jrd.2024.0029
Abstract
Objective
The purpose of this study is to evaluate the impact of tumor necrosis factor (TNF)-α blocker therapy on the Assessment of SpondyloArthritis international Society Health Index (ASAS-HI) among patients who have failed conventional nonsteroidal anti-inflammatory drugs.
Methods
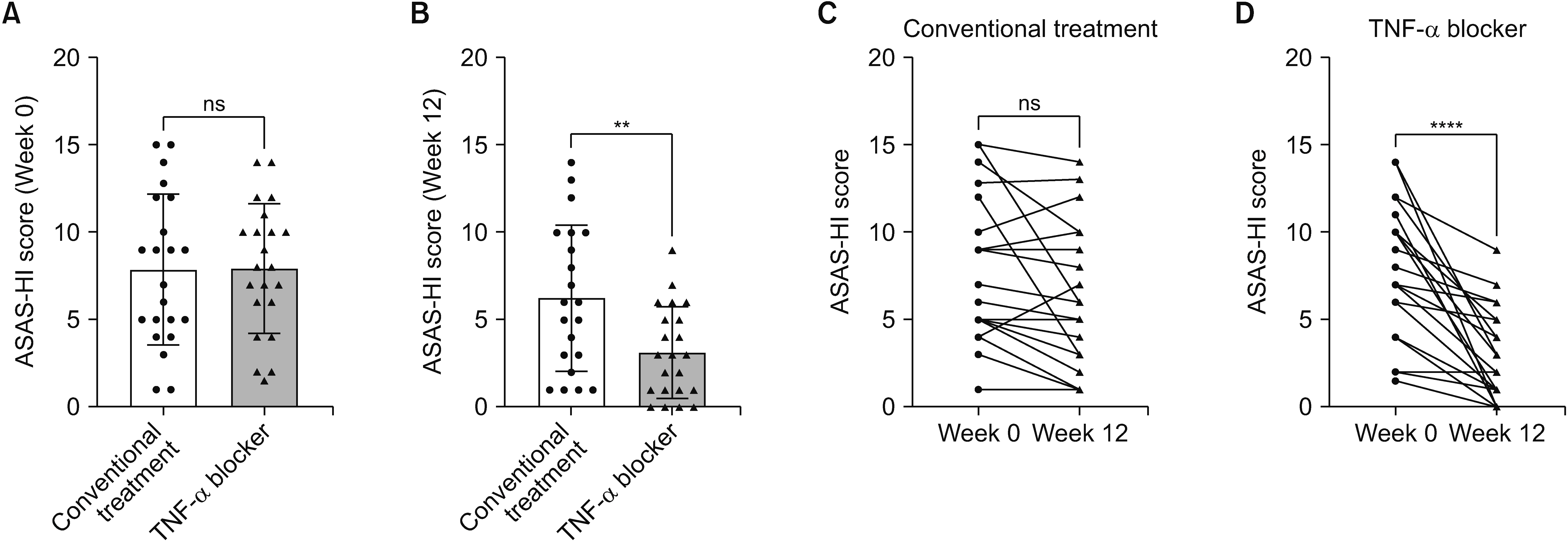
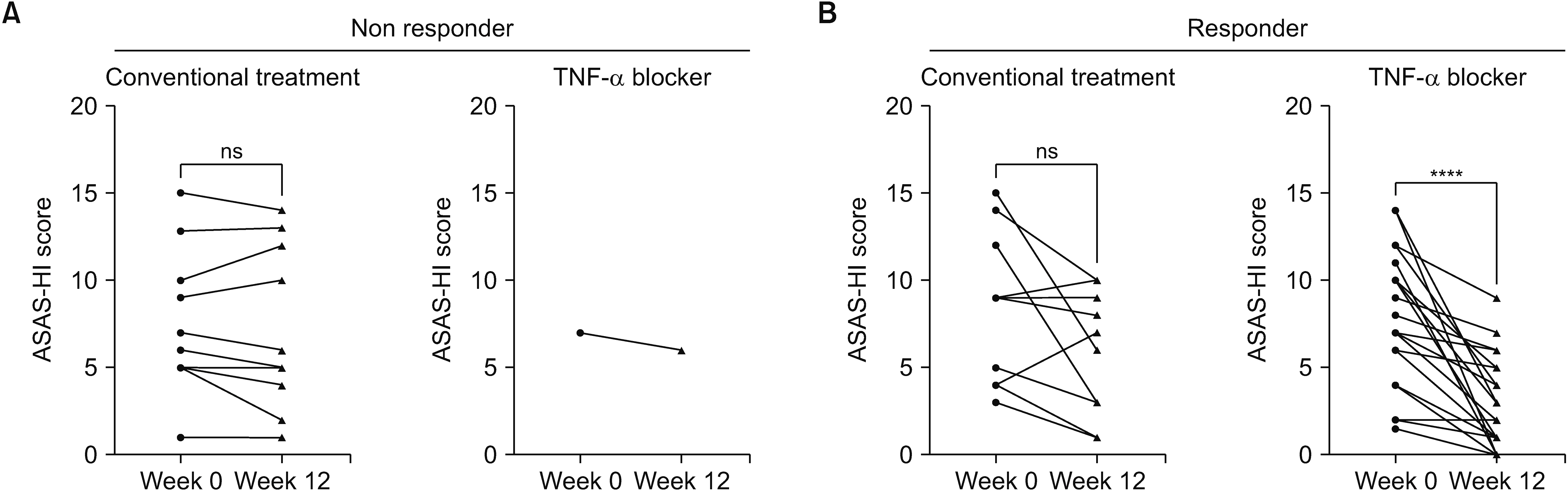
A comparative study was conducted involving axial spondyloarthritis (axSpA) patients treated with either TNF-α blocker or conventional therapy. Patient data, including demographics, disease characteristics, and ASAS-HI scores, were collected before and after treatment. Statistical analysis was performed to compare changes in ASAS-HI scores between the TNF-α blocker and the conventional therapy group.
Results
The study population consisted of patients with axSpA, with a mean age of 38.3 years in conventional treatment group and 29.3 years in TNF-α blocker group. Most variables, including C-reactive protein levels, other comorbidities, and disease assessment scores showed no significant difference between groups. Longitudinal analysis within each treatment group from Week 0 to 12 showed no significant change in the conventional treatment group, whereas the TNF-α blocker group experienced a significant reduction in ASAS-HI scores, demonstrating the effectiveness of the treatment. The TNF-α blocker group exhibited a significantly greater improvement in ASAS-HI scores compared to the conventional therapy group. The Bath Ankylosing Spondylitis Functional Index and the Bath Ankylosing Spondylitis Disease Activity Index demonstrated strong positive correlations with ASAS-HI scores, indicating higher disease activity and functional limitation are associated with worse health outcomes in patients.
Conclusion
The research demonstrates that ASAS-HI scores significantly improve with TNF-α blocker therapy in axSpA patients, underscoring ASAS-HI's effectiveness as a tool for evaluating drug responses.
Keyword
Figure
Reference
-
1. Seo MR, Yeo J, Park JW, Lee YA, Lee JH, Kang EH, et al. 2023; Korean treatment recommendations for patients with axial spondyloarthritis. J Rheum Dis. 30:151–69. Erratum in: J Rheum Dis 2024;31:62-3. DOI: 10.4078/jrd.2023.0025C. PMID: 38164191. PMCID: PMC10730801.
Article2. Kiltz U, van der Heijde D, Boonen A, Akkoc N, Bautista-Molano W, Burgos-Vargas R, et al. 2018; Measurement properties of the ASAS Health Index: results of a global study in patients with axial and peripheral spondyloarthritis. Ann Rheum Dis. 77:1311–7. DOI: 10.1136/annrheumdis-2017-212076. PMID: 29858176.
Article3. Rudwaleit M, Landewé R, van der Heijde D, Listing J, Brandt J, Braun J, et al. 2009; The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis. 68:770–6. Erratum in: Ann Rheum Dis 2011;70:1519. DOI: 10.1136/ard.2009.108217. PMID: 19297345.
Article4. van der Heijde D, Lie E, Kvien TK, Sieper J, Van den Bosch F, Listing J, et al. 2009; ASDAS, a highly discriminatory ASAS-endorsed disease activity score in patients with ankylosing spondylitis. Ann Rheum Dis. 68:1811–8. DOI: 10.1136/ard.2008.100826. PMID: 19060001.
Article5. Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. 1994; A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 21:2286–91.6. Calin A, Garrett S, Whitelock H, Kennedy LG, O'Hea J, Mallorie P, et al. 1994; A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol. 21:2281–5.7. Kiltz U, van der Heijde D, Boonen A, Braun J. 2014; The ASAS Health Index (ASAS-HI)- a new tool to assess the health status of patients with spondyloarthritis. Clin Exp Rheumatol. 32(5 Suppl 8):S-105–8.8. Kiltz U, van der Heijde D, Boonen A, Cieza A, Stucki G, Khan MA, et al. 2015; Development of a health index in patients with ankylosing spondylitis (ASAS-HI): final result of a global initiative based on the ICF guided by ASAS. Ann Rheum Dis. 74:830–5. DOI: 10.1136/annrheumdis-2013-203967. PMID: 24399232. PMCID: PMC4511705.
Article9. Navarro-Compán V, Boel A, Boonen A, Mease PJ, Dougados M, Kiltz U, et al. 2023; Instrument selection for the ASAS core outcome set for axial spondyloarthritis. Ann Rheum Dis. 82:763–72. DOI: 10.1136/annrheumdis-2022-222747. PMID: 35680390.
Article10. Navarro-Compán V, Boel A, Boonen A, Mease P, Landewé R, Kiltz U, et al. 2021; The ASAS-OMERACT core domain set for axial spondyloarthritis. Semin Arthritis Rheum. 51:1342–9. DOI: 10.1016/j.semarthrit.2021.07.021. PMID: 34489113.
Article11. Molto A, López-Medina C, Van den Bosch FE, Boonen A, Webers C, Dernis E, et al. 2021; Efficacy of a tight-control and treat-to-target strategy in axial spondyloarthritis: results of the open-label, pragmatic, cluster-randomised TICOSPA trial. Ann Rheum Dis. 80:1436–44. DOI: 10.1136/annrheumdis-2020-219585. PMID: 33958325. PMCID: PMC8522451.
Article12. Choi JH, Kim TJ, Shin K, Choi CB, Kim JH, Kim SH, et al. 2014; The reliability and validity of a Korean translation of the ASAS Health Index and Environmental Factors in Korean patients with axial spondyloarthritis. J Korean Med Sci. 29:334–7. DOI: 10.3346/jkms.2014.29.3.334. PMID: 24616580. PMCID: PMC3945126.
Article13. Di Carlo M, Lato V, Carotti M, Salaffi F. 2016; Clinimetric properties of the ASAS health index in a cohort of Italian patients with axial spondyloarthritis. Health Qual Life Outcomes. 14:78. DOI: 10.1186/s12955-016-0463-1. PMID: 27188166. PMCID: PMC4869300.
Article14. Akgul O, Bodur H, Ataman S, Yurdakul FG, Capkin E, Gurer G, et al. 2020; Clinical performance of ASAS Health Index in patients with ankylosing spondylitis and non-radiographic axial spondyloarthritis: real-world evidence from Multicenter Nationwide Registry. Rheumatol Int. 40:1793–801. DOI: 10.1007/s00296-020-04680-8. PMID: 32814986.
Article15. Redeker I, Landewé R, van der Heijde D, Ramiro S, Boonen A, Dougados M, et al. 2023; Impact of disease outcomes on the Assessment of SpondyloArthritis International Society Health Index (ASAS-HI): a Bayesian network analysis of the DESIR cohort. RMD Open. 9:e003587. DOI: 10.1136/rmdopen-2023-003587. PMID: 38123481. PMCID: PMC10748975.16. Regierer AC, Weiß A, Kiltz U, Sieper J, Schwarze I, Bohl-Bühler M, et al. 2023; The sensitivity to change of the ASAS Health Index in an observational real-life cohort study. J Rheumatol. 50:185–91. DOI: 10.3899/jrheum.220212. PMID: 35914790.
Article17. Başkan BM, Sivas F, Inal EE, Duran S, Elverici E, Ozoran K, et al. 2010; Comparison of the Bath Ankylosing Spondylitis Radiology Index and the modified Stoke Ankylosing Spondylitis Spine Score in Turkish patients with ankylosing spondylitis. Clin Rheumatol. 29:65–70. DOI: 10.1007/s10067-009-1290-0. PMID: 19813046.
Article18. Landewé R, Dougados M, Mielants H, van der Tempel H, van der Heijde D. 2009; Physical function in ankylosing spondylitis is independently determined by both disease activity and radiographic damage of the spine. Ann Rheum Dis. 68:863–7. DOI: 10.1136/ard.2008.091793. PMID: 18628283.
Article19. Machado P, Landewé R, Braun J, Hermann KG, Baker D, van der Heijde D. 2010; Both structural damage and inflammation of the spine contribute to impairment of spinal mobility in patients with ankylosing spondylitis. Ann Rheum Dis. 69:1465–70. DOI: 10.1136/ard.2009.124206. PMID: 20498215.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MRI Features of Axial Spondyloarthritis and Differential Diagnosis: Focusing on the Spine and Sacroiliac Joint
- Tailored Treatment of Ankylosing Spondylitis
- The Reliability and Validity of a Korean Translation of the ASAS Health Index and Environmental Factors in Korean Patients with Axial Spondyloarthritis
- Study on Clinical Effectiveness of the Korean Version of Assessment of SpondyloArthritis International Society-Health Index
- Treatment of Ankylosing Spondylitis