J Rheum Dis.
2024 Jul;31(3):160-170. 10.4078/jrd.2024.0007.
Clinical characteristics and courses of Korean patients with giant cell arteritis: a multi-center retrospective study
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Seoul National University Hospital, Department of Internal Medicine, Seoul, Korea
- 3Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 4Seoul University College of Medicine, Seoul, Korea
- 5Kangdong Sacred Heart Hospital, Seoul, Korea
- KMID: 2557385
- DOI: http://doi.org/10.4078/jrd.2024.0007
Abstract
Objective
Giant cell arteritis (GCA) is a large-vessel vasculitis that primarily affects elderly individuals. However, data regarding Korean patients with GCA are scarce owing to its extremely low prevalence in East Asia. This study aimed to investigate the clinical characteristics of Korean patients with GCA and their outcomes, focusing on relapse.
Methods
The medical records of 27 patients with GCA treated at three tertiary hospitals between 2007 and 2022 were retrospectively reviewed.
Results
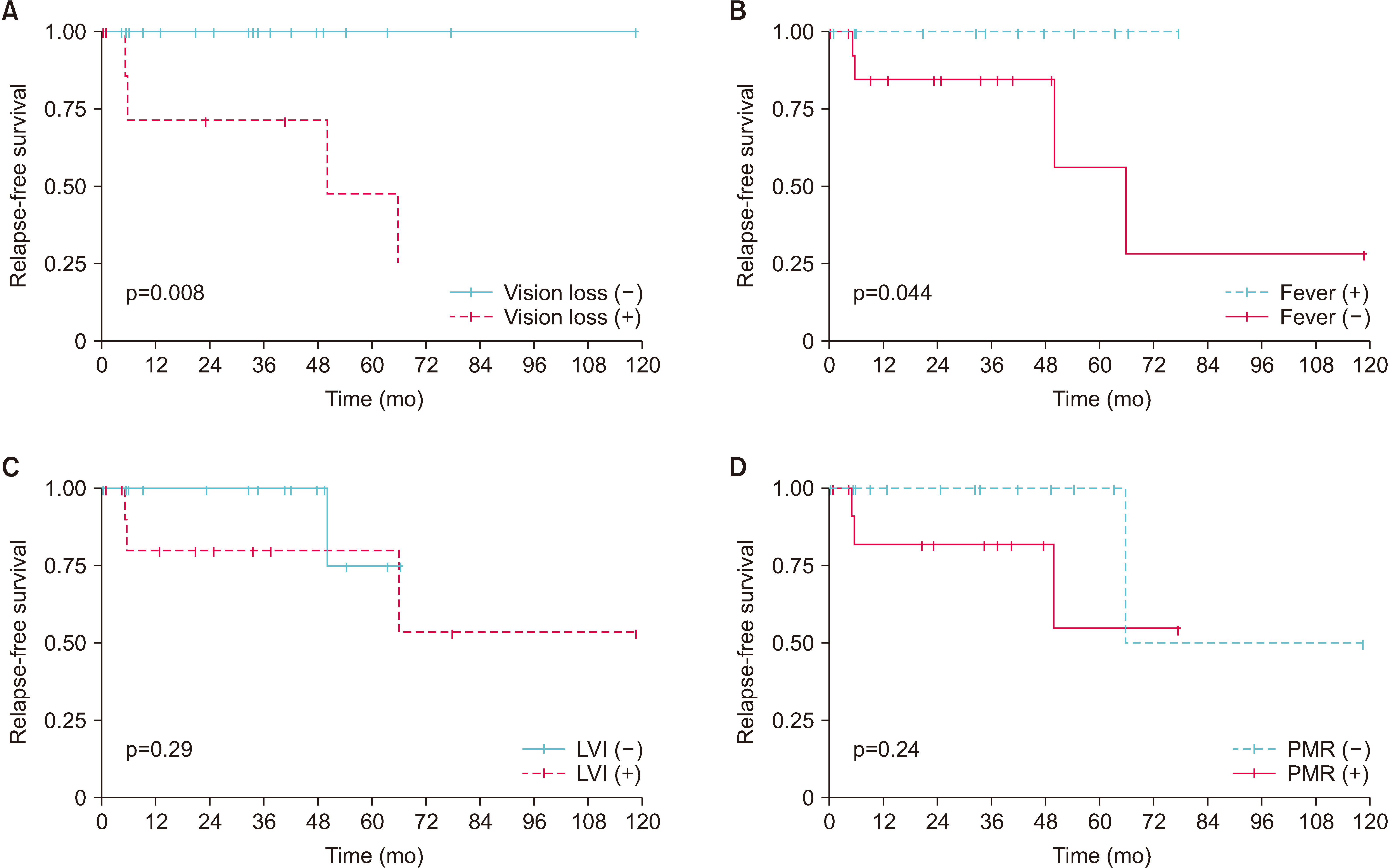
Seventeen (63.0%) patients were females, and the median age at diagnosis was 75 years. Large vessel involvement (LVI) was detected in 12 (44.4%) patients, and polymyalgia rheumatica (PMR) was present in 14 (51.9%) patients. Twelve (44.4%) patients had fever at onset. The presence of LVI or concurrent PMR at diagnosis was associated with a longer time to normalization of the C-reactive protein level (p=0.039) or erythrocyte sedimentation rate (p=0.034). During follow-up (median: 33.8 months), four (14.8%) patients experienced relapse. Kaplan-Meier analyses showed that relapse was associated with visual loss (p=0.008) and the absence of fever (p=0.004) at onset, but not with LVI or concurrent PMR.
Conclusion
Concurrent PMR and LVI were observed in approximately half of Korean patients with GCA, and the elapsed time to normalization of inflammatory markers in these patients was longer. The relapse rate in Korean GCA is lower than that in Western countries, and afebrile patients or patients with vision loss at onset have a higher risk of relapse, suggesting that physicians should carefully monitor patients with these characteristics.
Figure
Reference
-
1. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2013; 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 65:1–11. DOI: 10.1002/art.37715. PMID: 23045170.
Article2. Gonzalez-Gay MA, Vazquez-Rodriguez TR, Lopez-Diaz MJ, Miranda-Filloy JA, Gonzalez-Juanatey C, Martin J, et al. 2009; Epidemiology of giant cell arteritis and polymyalgia rheumatica. Arthritis Rheum. 61:1454–61. DOI: 10.1002/art.24459. PMID: 19790127.
Article3. Crowson CS, Matteson EL, Myasoedova E, Michet CJ, Ernste FC, Warrington KJ, et al. 2011; The lifetime risk of adult-onset rheumatoid arthritis and other inflammatory autoimmune rheumatic diseases. Arthritis Rheum. 63:633–9. DOI: 10.1002/art.30155. PMID: 21360492. PMCID: PMC3078757.
Article4. Yoshida M, Watanabe R, Ishii T, Machiyama T, Akita K, Fujita Y, et al. 2016; Retrospective analysis of 95 patients with large vessel vasculitis: a single center experience. Int J Rheum Dis. 19:87–94. DOI: 10.1111/1756-185X.12777. PMID: 26443306.
Article5. Kobayashi S, Yano T, Matsumoto Y, Numano F, Nakajima N, Yasuda K, et al. 2003; Clinical and epidemiologic analysis of giant cell (temporal) arteritis from a nationwide survey in 1998 in Japan: the first government-supported nationwide survey. Arthritis Rheum. 49:594–8. DOI: 10.1002/art.11195. PMID: 12910568.
Article6. Choi JH, Shin JH, Jung JH. 2019; Arteritic anterior ischemic optic neuropathy associated with giant-cell arteritis in Korean patients: a retrospective single-center analysis and review of the literature. J Clin Neurol. 15:386–92. DOI: 10.3988/jcn.2019.15.3.386. PMID: 31286712. PMCID: PMC6620454.
Article7. Gonzalez-Gay MA, Barros S, Lopez-Diaz MJ, Garcia-Porrua C, Sanchez-Andrade A, Llorca J. 2005; Giant cell arteritis: disease patterns of clinical presentation in a series of 240 patients. Medicine (Baltimore). 84:269–76. DOI: 10.1097/01.md.0000180042.42156.d1. PMID: 16148727.
Article8. Yamaguchi E, Kadoba K, Watanabe R, Iwasaki T, Kitagori K, Akizuki S, et al. 2023; Clinical profile and outcome of large-vessel giant cell arteritis in Japanese patients: a single-centre retrospective cohort study. Mod Rheumatol. 33:175–81. DOI: 10.1093/mr/roac013. PMID: 35141755.
Article9. Muratore F, Kermani TA, Crowson CS, Green AB, Salvarani C, Matteson EL, et al. 2015; Large-vessel giant cell arteritis: a cohort study. Rheumatology (Oxford). 54:463–70. DOI: 10.1093/rheumatology/keu329. PMID: 25193809. PMCID: PMC4425829.
Article10. Zhang Y, Wang D, Yin Y, Fan H, Zhang W, Zeng X. 2019; Clinical comparisons of patients with giant cell arteritis with versus without fever at onset. J Int Med Res. 47:5613–22. DOI: 10.1177/0300060519875379. PMID: 31547723. PMCID: PMC6862894.
Article11. Dumont A, Parienti JJ, Delmas C, Boutemy J, Maigné G, Martin Silva N, et al. 2020; Factors associated with relapse and dependence on glucocorticoids in giant cell arteritis. J Rheumatol. 47:108–16. DOI: 10.3899/jrheum.181127. PMID: 30877210.
Article12. Kermani TA, Warrington KJ, Cuthbertson D, Carette S, Hoffman GS, Khalidi NA, et al. 2015; Disease relapses among patients with giant cell arteritis: a prospective, longitudinal cohort study. J Rheumatol. 42:1213–7. DOI: 10.3899/jrheum.141347. PMID: 25877501. PMCID: PMC4505815.
Article13. Hocevar A, Rotar Z, Jese R, Semrl SS, Pizem J, Hawlina M, et al. 2016; Do early diagnosis and glucocorticoid treatment decrease the risk of permanent visual loss and early relapses in giant cell arteritis: a prospective longitudinal study. Medicine (Baltimore). 95:e3210. DOI: 10.1097/MD.0000000000003210. PMID: 27057850. PMCID: PMC4998766.14. Venerito V, Emmi G, Cantarini L, Leccese P, Fornaro M, Fabiani C, et al. 2022; Validity of machine learning in predicting giant cell arteritis flare after glucocorticoids tapering. Front Immunol. 13:860877. DOI: 10.3389/fimmu.2022.860877. PMID: 35450069. PMCID: PMC9017227.
Article15. Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, et al. 1990; The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 33:1122–8. DOI: 10.1002/art.1780330810. PMID: 2202311.
Article16. Ponte C, Grayson PC, Robson JC, Suppiah R, Gribbons KB, Judge A, et al. 2022; 2022 American College of Rheumatology/EULAR classification criteria for giant cell arteritis. Arthritis Rheumatol. 74:1881–9. DOI: 10.1002/art.42325. PMID: 36350123.
Article17. Dasgupta B, Cimmino MA, Kremers HM, Schmidt WA, Schirmer M, Salvarani C, et al. 2012; 2012 Provisional classification criteria for polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Arthritis Rheum. 64:943–54. DOI: 10.1002/art.34356. PMID: 22389040.
Article18. Koster MJ, Matteson EL, Warrington KJ. 2018; Large-vessel giant cell arteritis: diagnosis, monitoring and management. Rheumatology (Oxford). 57(suppl_2):ii32–42. DOI: 10.1093/rheumatology/kex424. PMID: 29982778.
Article19. Villiger PM, Adler S, Kuchen S, Wermelinger F, Dan D, Fiege V, et al. 2016; Tocilizumab for induction and maintenance of remission in giant cell arteritis: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 387:1921–7. DOI: 10.1016/S0140-6736(16)00560-2. PMID: 26952547.
Article20. Ponte C, Martins-Martinho J, Luqmani RA. 2020; Diagnosis of giant cell arteritis. Rheumatology (Oxford). 59(Suppl 3):iii5–16. DOI: 10.1093/rheumatology/kez553. PMID: 32348512.
Article21. Kermani TA, Warrington KJ, Crowson CS, Ytterberg SR, Hunder GG, Gabriel SE, et al. 2013; Large-vessel involvement in giant cell arteritis: a population-based cohort study of the incidence-trends and prognosis. Ann Rheum Dis. 72:1989–94. DOI: 10.1136/annrheumdis-2012-202408. PMID: 23253927. PMCID: PMC4112513.
Article22. Nuenninghoff DM, Hunder GG, Christianson TJ, McClelland RL, Matteson EL. 2003; Incidence and predictors of large-artery complication (aortic aneurysm, aortic dissection, and/or large-artery stenosis) in patients with giant cell arteritis: a population-based study over 50 years. Arthritis Rheum. 48:3522–31. DOI: 10.1002/art.11353. PMID: 14674004.
Article23. Brack A, Martinez-Taboada V, Stanson A, Goronzy JJ, Weyand CM. 1999; Disease pattern in cranial and large-vessel giant cell arteritis. Arthritis Rheum. 42:311–7. DOI: 10.1002/1529-0131(199902)42:2<311::AID-ANR14>3.0.CO;2-F. PMID: 10025926.
Article24. Nielsen AW, Frølund LL, Våben C, Bonde AR, Gormsen LC, de Thurah AL, et al. 2022; Concurrent baseline diagnosis of giant cell arteritis and polymyalgia rheumatica - a systematic review and meta-analysis. Semin Arthritis Rheum. 56:152069. DOI: 10.1016/j.semarthrit.2022.152069. PMID: 35858507.
Article25. Blockmans D, De Ceuninck L, Vanderschueren S, Knockaert D, Mortelmans L, Bobbaers H. 2007; Repetitive 18-fluorodeoxyglucose positron emission tomography in isolated polymyalgia rheumatica: a prospective study in 35 patients. Rheumatology (Oxford). 46:672–7. DOI: 10.1093/rheumatology/kel376. PMID: 17114803.
Article26. Camellino D, Matteson EL, Buttgereit F, Dejaco C. 2020; Monitoring and long-term management of giant cell arteritis and polymyalgia rheumatica. Nat Rev Rheumatol. 16:481–95. Erratum in: Nat Rev Rheumatol 2020;16:662. DOI: 10.1038/s41584-020-0458-5. PMID: 32759996.
Article27. Unizony SH, Bao M, Han J, Luder Y, Pavlov A, Stone JH. 2021; Treatment failure in giant cell arteritis. Ann Rheum Dis. 80:1467–74. DOI: 10.1136/annrheumdis-2021-220347. PMID: 34049857. PMCID: PMC8522464.
Article28. Stone JH, Tuckwell K, Dimonaco S, Klearman M, Aringer M, Blockmans D, et al. 2017; Trial of tocilizumab in giant-cell arteritis. N Engl J Med. 377:317–28. DOI: 10.1056/NEJMoa1613849. PMID: 28745999.
Article29. Tal S, Guller V, Gurevich A, Levi S. 2002; Fever of unknown origin in the elderly. J Intern Med. 252:295–304. DOI: 10.1046/j.1365-2796.2002.01042.x. PMID: 12366602.
Article30. Liozon E, Boutros-Toni F, Ly K, Loustaud-Ratti V, Soria P, Vidal E. 2003; Silent, or masked, giant cell arteritis is associated with a strong inflammatory response and a benign short term course. J Rheumatol. 30:1272–6.31. Labarca C, Koster MJ, Crowson CS, Makol A, Ytterberg SR, Matteson EL, et al. 2016; Predictors of relapse and treatment outcomes in biopsy-proven giant cell arteritis: a retrospective cohort study. Rheumatology (Oxford). 55:347–56. DOI: 10.1093/rheumatology/kev348. PMID: 26385368. PMCID: PMC4939727.
Article32. Martinez-Lado L, Calviño-Díaz C, Piñeiro A, Dierssen T, Vazquez-Rodriguez TR, Miranda-Filloy JA, et al. 2011; Relapses and recurrences in giant cell arteritis: a population-based study of patients with biopsy-proven disease from northwestern Spain. Medicine (Baltimore). 90:186–93. DOI: 10.1097/MD.0b013e31821c4fad. PMID: 21512412.33. Matsumoto K, Kaneko Y, Takeuchi T. 2019; Body mass index associates with disease relapse in patients with giant cell arteritis. Int J Rheum Dis. 22:1782–6. DOI: 10.1111/1756-185X.13642. PMID: 31245915.
Article34. Nesher G, Poltorak V, Hindi I, Nesher R, Dror Y, Orbach H, et al. 2019; Survival of patient with giant cell arteritis: impact of vision loss and treatment with aspirin. Autoimmun Rev. 18:831–4. DOI: 10.1016/j.autrev.2019.06.003. PMID: 31176872.
Article35. Ince B, Artan S, Yalcinkaya Y, Artim-Esen B, Gul A, Ocal L, et al. 2021; Long-term follow-up of 89 patients with giant cell arteritis: a retrospective observational study on disease characteristics, flares and organ damage. Rheumatol Int. 41:439–48. DOI: 10.1007/s00296-020-04730-1. PMID: 33113000.
Article36. Kermani TA, Warrington KJ. 2018; Prognosis and monitoring of giant cell arteritis and associated complications. Expert Rev Clin Immunol. 14:379–88. DOI: 10.1080/1744666X.2018.1467758. PMID: 29676201.
Article37. Hernández-Rodríguez J, Segarra M, Vilardell C, Sánchez M, García-Martínez A, Esteban MJ, et al. 2003; Elevated production of interleukin-6 is associated with a lower incidence of disease-related ischemic events in patients with giant-cell arteritis: angiogenic activity of interleukin-6 as a potential protective mechanism. Circulation. 107:2428–34. DOI: 10.1161/01.CIR.0000066907.83923.32. PMID: 12742994.