J Rheum Dis.
2024 Jul;31(3):151-159. 10.4078/jrd.2024.0001.
The monocyte-to-high-density lipoprotein-cholesterol ratio at diagnosis is associated with cerebrovascular accident during follow-up in patients with antineutrophil cytoplasmic antibody-associated vasculitis
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Institute for Immunology and Immunological Diseases, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2557384
- DOI: http://doi.org/10.4078/jrd.2024.0001
Abstract
Objective
In this study, the association between the monocyte-to-high-density lipoprotein cholesterol ratio (MHR) at diagnosis and poor outcomes of atherosclerosis-related antineutrophil cytoplasmic antibody-associated vasculitis (AAV) during follow-up in patients with AAV was investigated.
Methods
This retrospective study included 138 patients diagnosed with AAV. Their comprehensive medical records were meticulously reviewed. All-cause mortality, cerebrovascular accident (CVA), and acute coronary syndrome (ACS) were evaluated as atherosclerosis-related poor outcomes of AAV. MHR was obtained by dividing monocyte counts (/mm3 ) by high-density lipoprotein cholesterol (mg/dL) levels.
Results
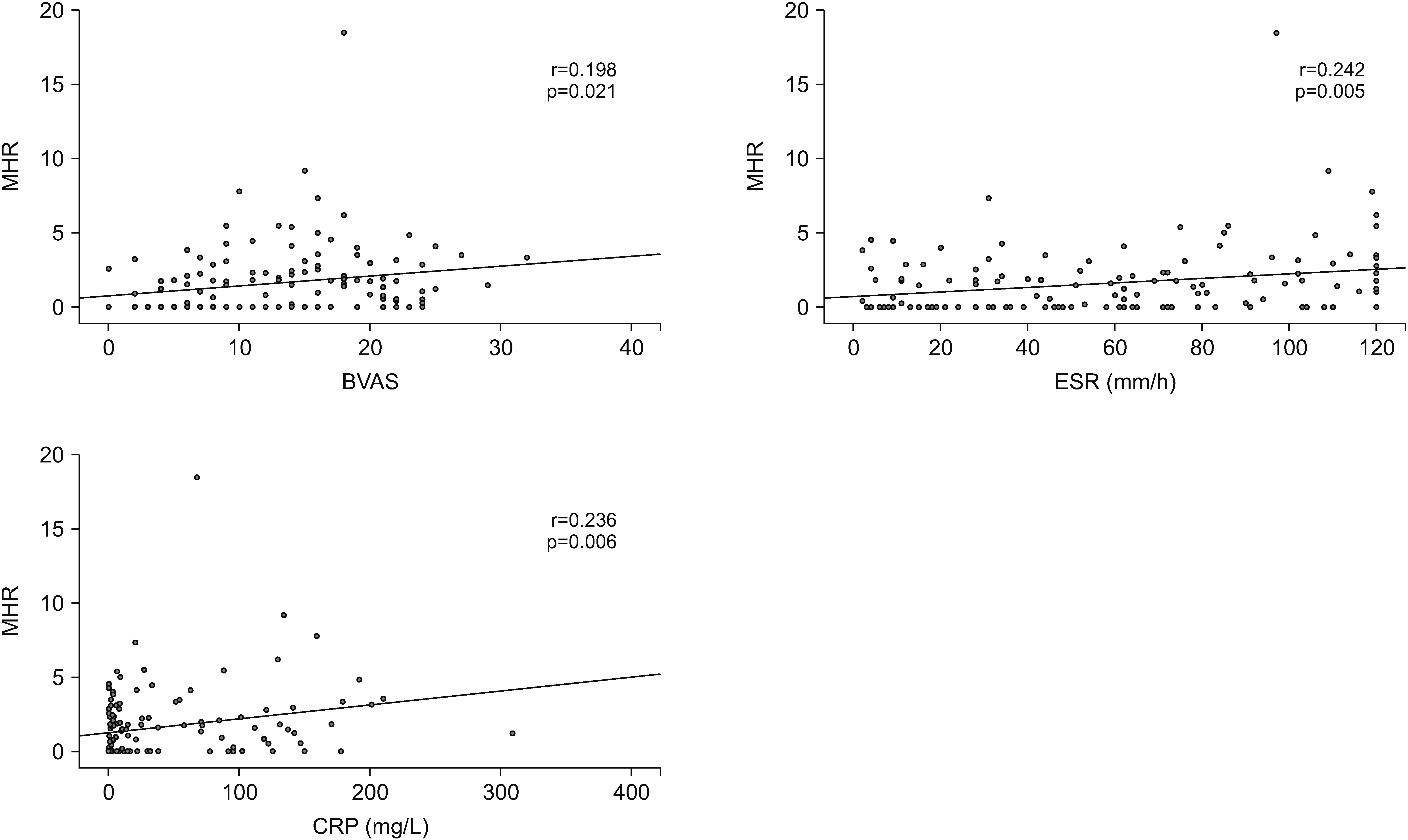
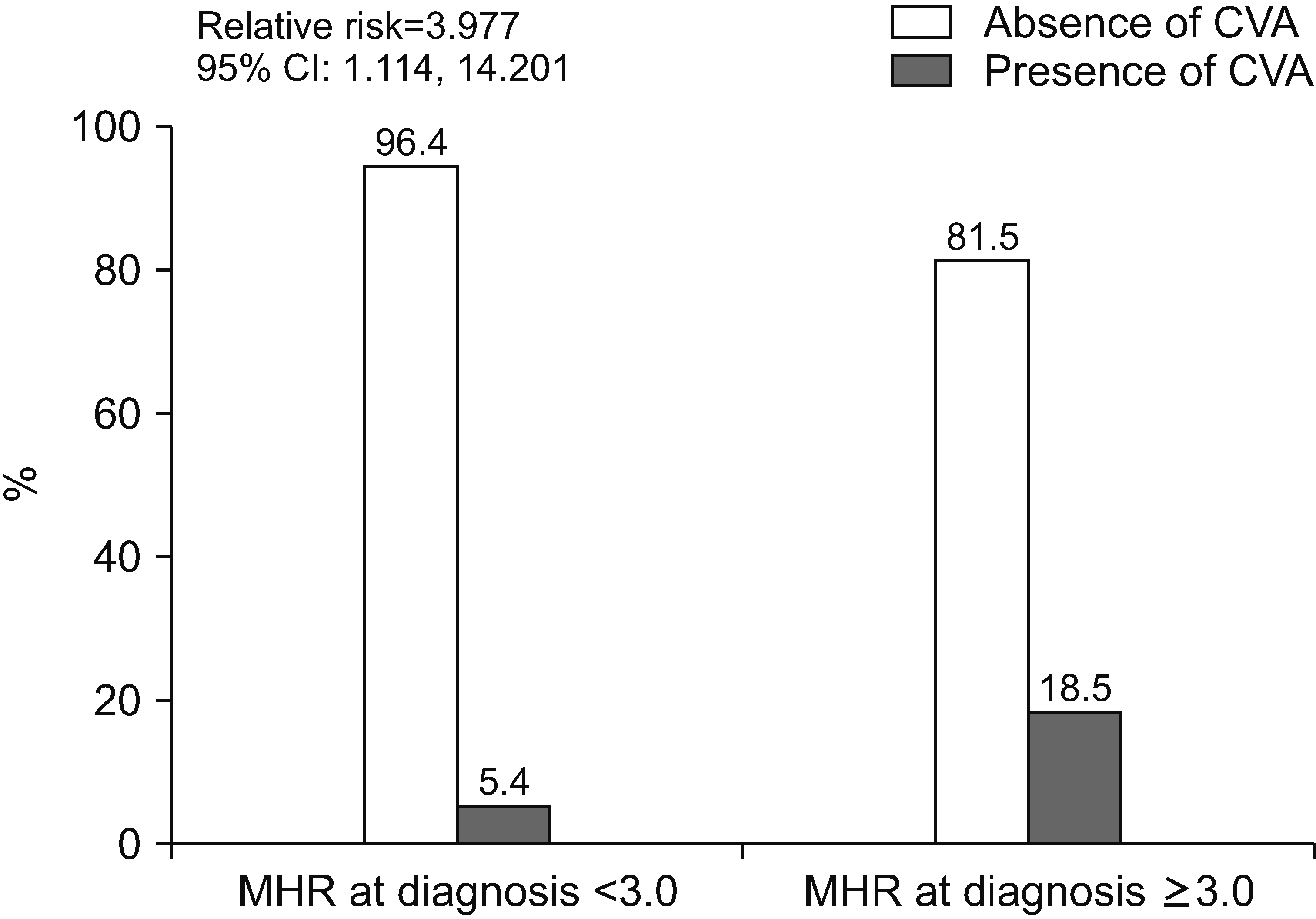
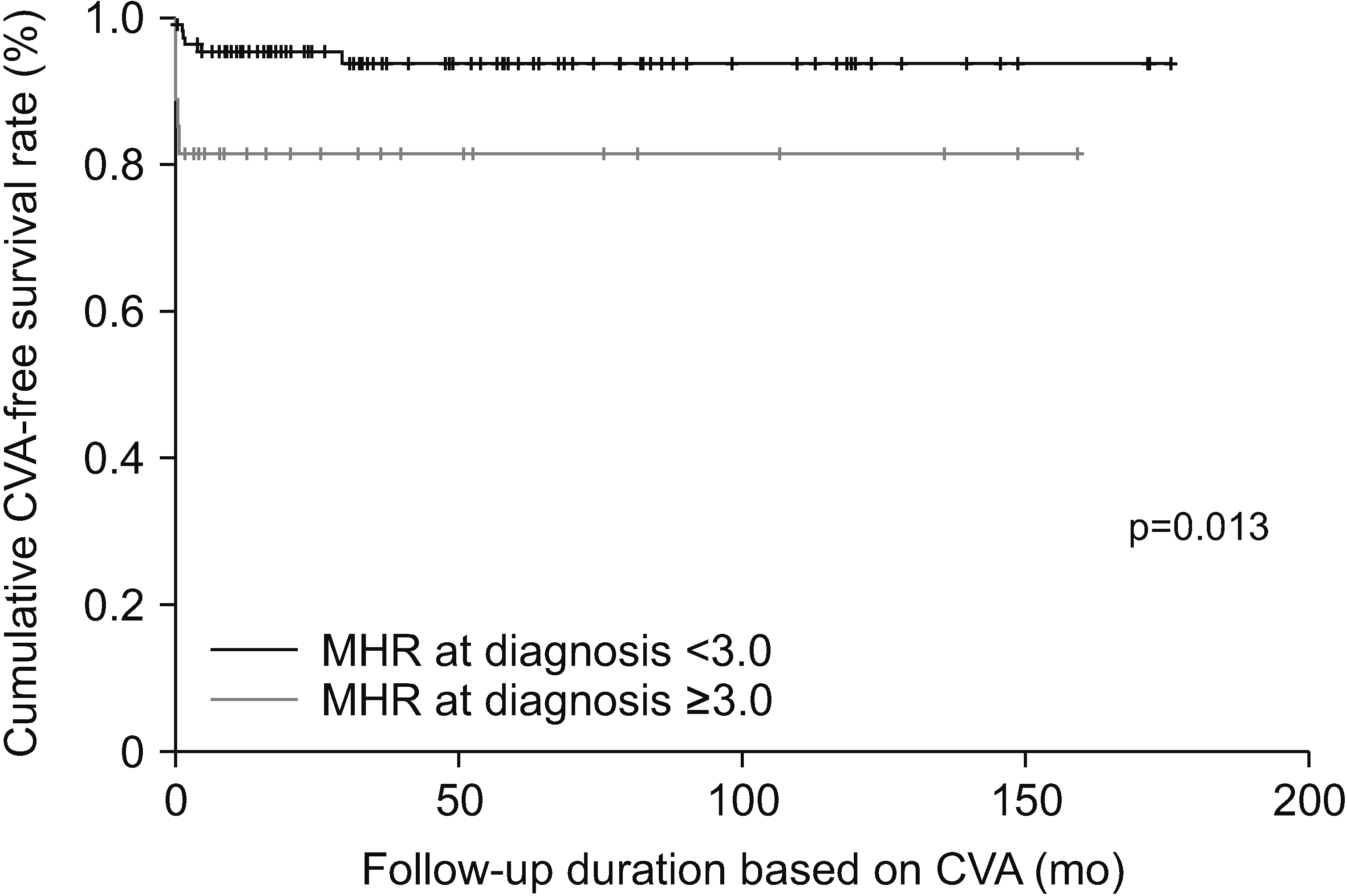
The median age of the 138 patients was 58.3 years with 44 being male (31.9%). Among the 138 patients, 11 (8.0%) died, and 11 (8.0%) and 9 (6.5%) had CVA, and ACS, respectively. MHR at diagnosis was significantly correlated with the Birmingham vasculitis activity score, erythrocyte sedimentation rate, and C-reactive protein at diagnosis. Among the three poor outcomes of AAV, only CVA during follow-up was significantly associated with MHR at diagnosis, and thus, only CVA was considered an atherosclerosis-related poor outcome of AAV. In the multivariable Cox hazards model analysis, MHR (hazard ratio [HR]: 1.195) and serum albumin (HR: 0.203) at diagnosis were independently associated with CVA during follow-up. Additionally, patients with MHR at diagnosis ≥3.0 exhibited a significantly higher risk for CVA and lower cumulative CVA-free survival rate than those with MHR at diagnosis <3.0.
Conclusion
This study is the first to demonstrate clinical implications of MHR suggesting that MHR at diagnosis is significantly and independently associated with CVA during follow-up in patients with AAV.
Keyword
Figure
Reference
-
1. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2013; 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 65:1–11. DOI: 10.1002/art.37715. PMID: 23045170.
Article2. Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, et al. 2007; Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis. 66:222–7. DOI: 10.1136/ard.2006.054593. PMID: 16901958. PMCID: PMC1798520.
Article3. Millet A, Pederzoli-Ribeil M, Guillevin L, Witko-Sarsat V, Mouthon L. 2013; Antineutrophil cytoplasmic antibody-associated vasculitides: is it time to split up the group? Ann Rheum Dis. 72:1273–9. DOI: 10.1136/annrheumdis-2013-203255. PMID: 23606701.
Article4. Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, et al. 2009; Modification and validation of the Birmingham Vasculitis Activity Score (version 3). Ann Rheum Dis. 68:1827–32. DOI: 10.1136/ard.2008.101279. PMID: 19054820.
Article5. Jiang M, Yang J, Zou H, Li M, Sun W, Kong X. 2022; Monocyte-to-high-density lipoprotein-cholesterol ratio (MHR) and the risk of all-cause and cardiovascular mortality: a nationwide cohort study in the United States. Lipids Health Dis. 21:30. DOI: 10.1186/s12944-022-01638-6. PMID: 35300686. PMCID: PMC8931976.
Article6. Chen JW, Li C, Liu ZH, Shen Y, Ding FH, Shu XY, et al. 2019; The role of monocyte to high-density lipoprotein cholesterol ratio in prediction of carotid intima-media thickness in patients with type 2 diabetes. Front Endocrinol (Lausanne). 10:191. DOI: 10.3389/fendo.2019.00191. PMID: 31019490. PMCID: PMC6458254.
Article7. Xi J, Men S, Nan J, Yang Q, Dong J. 2022; The blood monocyte to high density lipoprotein cholesterol ratio (MHR) is a possible marker of carotid artery plaque. Lipids Health Dis. 21:130. Erratum in: Lipids Health Dis 2022;21:144. DOI: 10.1186/s12944-022-01741-8. PMID: 36463176. PMCID: PMC9719628.
Article8. Lee SW, Park YB. 2019; Classification of antineutrophil cytoplasmic antibody-associated vasculitis. J Rheum Dis. 26:156–64. DOI: 10.4078/jrd.2019.26.3.156.
Article9. Suppiah R, Robson JC, Grayson PC, Ponte C, Craven A, Khalid S, et al. 2022; 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology classification criteria for microscopic polyangiitis. Ann Rheum Dis. 81:321–6. DOI: 10.1136/annrheumdis-2021-221796. PMID: 35110332.
Article10. Robson JC, Grayson PC, Ponte C, Suppiah R, Craven A, Judge A, et al. 2022; 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology classification criteria for granulomatosis with polyangiitis. Ann Rheum Dis. 81:315–20. DOI: 10.1136/annrheumdis-2021-221795. PMID: 35110333.
Article11. Grayson PC, Ponte C, Suppiah R, Robson JC, Craven A, Judge A, et al. 2022; 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology classification criteria for eosinophilic granulomatosis with polyangiitis. Ann Rheum Dis. 81:309–14. DOI: 10.1136/annrheumdis-2021-221794. PMID: 35110334.
Article12. Pyo JY, Lee LE, Park YB, Lee SW. 2023; Comparison of the 2022 ACR/EULAR classification criteria for antineutrophil cytoplasmic antibody-associated vasculitis with previous criteria. Yonsei Med J. 64:11–7. DOI: 10.3349/ymj.2022.0435. PMID: 36579374. PMCID: PMC9826961.
Article13. Kim JH, Lim S, Park KS, Jang HC, Choi SH. 2017; Total and differential WBC counts are related with coronary artery atherosclerosis and increase the risk for cardiovascular disease in Koreans. PLoS One. 12:e0180332. DOI: 10.1371/journal.pone.0180332. PMID: 28753607. PMCID: PMC5533311.
Article14. Li Y, Zhang M, Xue M, Liu D, Sun J. 2022; Elevated monocyte-to-HDL cholesterol ratio predicts post-stroke depression. Front Psychiatry. 13:902022. DOI: 10.3389/fpsyt.2022.902022. PMID: 35935403. PMCID: PMC9354071.
Article15. Liu Z, Fan Q, Wu S, Lei Y. 2021; Associations of monocytes and the monocyte/high-density lipoprotein ratio with extracranial and intracranial atherosclerotic stenosis. Front Neurol. 12:756496. DOI: 10.3389/fneur.2021.756496. PMID: 34925216. PMCID: PMC8678066.
Article16. Geovanini GR, Libby P. 2018; Atherosclerosis and inflammation: overview and updates. Clin Sci (Lond). 132:1243–52. DOI: 10.1042/CS20180306. PMID: 29930142.
Article17. Singh SK, Suresh MV, Voleti B, Agrawal A. 2008; The connection between C-reactive protein and atherosclerosis. Ann Med. 40:110–20. DOI: 10.1080/07853890701749225. PMID: 18293141. PMCID: PMC3364506.
Article18. Tabakovic D, Smith R, Jayne D, Mohammad AJ. 2023; High risk of stroke in ANCA-associated vasculitis-a population-based study. Rheumatology (Oxford). 62:2806–12. DOI: 10.1093/rheumatology/keac669. PMID: 36440920. PMCID: PMC10393431.
Article19. Kelly-Hayes M. 2010; Influence of age and health behaviors on stroke risk: lessons from longitudinal studies. J Am Geriatr Soc. 58(Suppl 2):S325–8. DOI: 10.1111/j.1532-5415.2010.02915.x. PMID: 21029062. PMCID: PMC3006180.20. Shi C, Pamer EG. 2011; Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 11:762–74. DOI: 10.1038/nri3070. PMID: 21984070. PMCID: PMC3947780.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ANCA : The Marker Antibody of Vasculitis
- ANCA-Associated Vasculitic Neuropathy with Concurrent Pulmonary Tuberculosis
- ANCA-Associated Vasculitis Presenting with Hypertrophic Pachymeningitis
- A Case of Propylthiouracil-induced Lupus Erythematosus Accompanied by Antineutrophil Cytoplasmic Antibody-positive Vasculitis
- Monocytes and High-density Lipoprotein Cholesterol in Branch Retinal Vein Occlusion