Womens Health Nurs.
2024 Jun;30(2):117-127. 10.4069/whn.2024.05.21.1.
Prevalence of pre-obesity and above and its associated factors in adult women: an analysis of the 2020 Korea National Health and Nutrition Examination Survey
- Affiliations
-
- 1College of Nursing, Sangmyung University, Cheonan, Korea
- KMID: 2557359
- DOI: http://doi.org/10.4069/whn.2024.05.21.1
Abstract
- Purpose
This study was conducted to determine the prevalence of pre-obesity (overweight) and above in adult women and to identify associated factors.
Methods
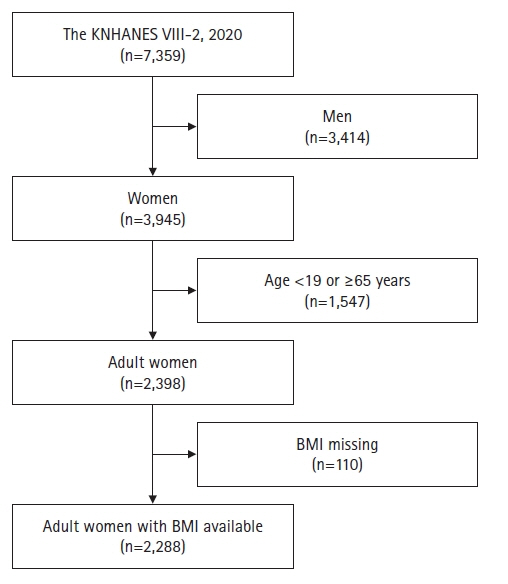
Data were obtained from the eighth Korea National Health and Nutrition Examination Survey (KNHANES VIII-2), conducted in 2020. The sample comprised 2,288 women aged 19–64 years who participated in the KNHANES VIII-2. Data were analyzed using complex sample design analysis with SPSS version 20.1.
Results
The prevalence of pre-obesity and above among adult women was 46.5%, with 18.6% classified as having pre-obesity and 27.9% as having obesity. A higher prevalence of pre-obesity and above was observed in women aged 50–59 years (odds ratio [OR]=1.67, p=.019) or 60–64 years (OR=1.80, p=.029); women whose highest educational attainment was high school (OR=1.28, p=.018) or middle school or less (OR=1.60, p=.017); those in middle-income households (OR=1.55, p=.005); those engaging in muscle-strengthening activities less than 2 days per week (OR=1.37, p=.019); and those sleeping less than 6 hours per night during the week (OR=1.37, p=.025).
Conclusion
As nearly half of all adult women have either pre-obesity or obesity, prevention and management strategies must target both groups. Interventions should be prioritized for women in their 50s and older, as well as those with low education or income levels. Additionally, receiving adequate sleep of 7 hours or more and engaging in muscle-strengthening activities at least 2 days per week are important components of obesity management.
Keyword
Figure
Reference
-
References
1. World Health Organization.. Obesity and overweight [Internet]. Geneva: Author;2021. [cited 2024 Jan 10]. Available from: https://www.who.int/news-room/fact-sheets/obesity-and-overweight.2. Keramat SA, Alam K, Sathi NJ, Gow J, Biddle SJH, Al-Hanawi MK. Self-reported disability and its association with obesity and physical activity in Australian adults: Results from a longitudinal study. SSM Popul Health. 2021; 14:100765. https://doi.org/10.1016/j.ssmph.2021.100765.
Article3. Organisation for Economic Co-operation and Development. Overweight and obesity [Internet]. Paris: Author;2023. [cited 2024 Jan 12]. Available from: https://www.oecd-ilibrary.org/sites/cba592fb-en/index.html?itemId=/content/component/cba592fb-en.4. Mangemba NT, San Sebastian M. Societal risk factors for overweight and obesity in women in Zimbabwe: a cross-sectional study. BMC Public Health. 2020; 20(1):103. https://doi.org/10.1186/s12889-020-8215-x.
Article5. Keramat SA, Alam K, Al-Hanawi MK, Gow J, Biddle SJH, Hashmi R. Trends in the prevalence of adult overweight and obesity in Australia, and its association with geographic remoteness. Sci Rep. 2021; 11(1):11320. https://doi.org/10.1038/s41598-021-90750-1.
Article6. Seo MH, Lee WY, Kim SS, Kang JH, Kang JH, Kim KK, et al. 2018 Korean Society for the Study of Obesity guideline for the management of obesity in Korea. J Obes Metab Syndr. 2019; 28(1):40–45. https://doi.org/10.7570/jomes.2019.28.1.40.
Article7. Kim SJ, Cho KW, Oh CS, Lee SM. Gender differences in obesity-related socioeconomic costs. J Health Info Stat. 2020; 45(2):181–190. https://doi.org/10.21032/jhis.2020.45.2.181.
Article8. Kapoor E, Faubion SS, Kling JM. Obesity update in women. J Womens Health (Larchmt). 2019; 28(12):1601–1605. https://doi.org/10.1089/jwh.2019.8041.
Article9. Kim DY, Park SY, Kim YJ, Oh KW. National Health Statistics Plus: Current status of obesity prevalence in Korean adults and related factors [Internet]. Cheongju, Korea: Korea Disease Control and Prevention Agency;2021. [cited 2024 Feb 6]. Available from: https://knhanes.kdca.go.kr/knhanes/sub04/sub04_04_02.do.10. Kim KB, Shin YA. Males with obesity and overweight. J Obes Metab Syndr. 2020; 29(1):18–25. https://doi.org/10.7570/jomes20008.
Article11. GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017; 377(1):13–27. https://doi.org/10.1056/NEJMoa1614362.
Article12. Li W, Fang W, Huang Z, Wang X, Cai Z, Chen G, et al. Association between age at onset of overweight and risk of hypertension across adulthood. Heart. 2022; 108(9):683–688. https://doi.org/10.1136/heartjnl-2021-320278.
Article13. Jardim PCBV. Overweight, the cardiovascular risk of the century. Arq Bras Cardiol. 2019; 113(2):185–187. https://doi.org/10.5935/abc.20190171.
Article14. Korean Society for the Study of Obesity. The Korean Society of Obesity publishes the revised “Clinical practice guidelines for obesity 2018” in 2018 [Internet]. Seoul: Korea Society for the Study of Obesity;2019. [cited 2024 Jan 1]. Available from: https://www.kosso.or.kr/newsletter/201905/sub02.html.15. Stoś K, Rychlik E, Woźniak A, Ołtarzewski M, Jankowski M, Gujski M, et al. Prevalence and sociodemographic factors associated with overweight and obesity among adults in Poland: a 2019/2020 nationwide cross-sectional survey. Int J Environ Res Public Health. 2022; 19(3):1502. https://doi.org/10.3390/ijerph19031502.
Article16. Asosega KA, Aidoo EN, Adebanji AO, Owusu-Dabo E. Examining the risk factors for overweight and obesity among women in Ghana: a multilevel perspective. Heliyon. 2023; 9(5):e16207. https://doi.org/10.1016/j.heliyon.2023.e16207.
Article17. Kwak JW, Jeon CH, Kwak MH, Kim JH, Park YS. Relationship between obesity and lifestyle factors in young Korean women: the seventh Korea National Health and Nutrition Examination Survey 2016. Korean J Health Promot. 2019; 19(1):9–15. https://doi.org/10.15384/kjhp.2019.19.1.9.
Article18. Johnson VR, Anekwe CV, Washington TB, Chhabria S, Tu L, Stanford FC. A women’s health perspective on managing obesity. Prog Cardiovasc Dis. 2023; 78:11–16. https://doi.org/10.1016/j.pcad.2023.04.007.
Article19. Tauqeer Z, Gomez G, Stanford FC. Obesity in women: insights for the clinician. J Womens Health (Larchmt). 2018; 27(4):444–457. https://doi.org/10.1089/jwh.2016.6196.
Article20. Link DG. Obesity in women: paying a high price. Nurs Clin North Am. 2021; 56(4):609–617. https://doi.org/10.1016/j.cnur.2021.07.005.
Article21. Korean Society for the Study of Obesity. Clinical practice guidelines for obesity 2022. 8th ed. Seoul: Korea Society for the Study of Obesity;2022.22. Korea Disease Control and Prevention Agency (KDCA). Korea Health Statistics 2020: Korea National Health and Nutrition Examination Survey (KNHNES VIII-2). Cheongju, Korea: KDCA;2022.23. World Health Organization (WHO). WHO guidelines on physical activity and sedentary behavior. Geneva: WHO;2020.24. Lima MG, Barros MB, Ceolim MF, Zancanella E, Cardoso TA. Sleep duration, health status, and subjective well-being: a population-based study. Rev Saude Publica. 2018; 52:82. https://doi.org/10.11606/S1518-8787.2018052000602.
Article25. Mohammadi-Nasrabadi M, Sadeghi R, Rahimiforushani A, Mohammadi-Nasrabadi F, Shojaeizadeh D, Montazeri A. Socioeconomic determinants of excess weight and central obesity among Iranian women: Application of information, motivation, and behavioral skills model. J Educ Health Promot. 2019; 8:75. https://doi.org/10.4103/jehp.jehp_427_18.
Article26. Motswagole B, Jackson J, Kobue-Lekalake R, Maruapula S, Mongwaketse T, Kwape L, et al. The association of general and central obesity with dietary patterns and socioeconomic status in adult women in Botswana. J Obes. 2020; 2020:4959272. https://doi.org/10.1155/2020/4959272.
Article27. Seidu AA, Ahinkorah BO, Agbaglo E, Nyaaba AA. Overweight and obesity among women of reproductive age in Mali: what are the determinants? Int Health. 2021; 13(5):428–435. https://doi.org/10.1093/inthealth/ihaa094.
Article28. Son C, Na W, Kim C, Choi S, Kim OY, Lee J, et al. Comparison of the levels of energy intake from dish and food groups by gender and age among Korean obese adults: data obtained from the 2013-2018 Korea National Health and Nutrition Examination Survey. J Nurt Health. 2022; 55(6):670–683. https://doi.org/10.4163/jnh.2022.55.6.670.
Article29. Kim J, Lim GE, Kang S, Lee K, Park TJ, Kim JS. The relationship between daily sodium intake and obesity in Korean adult. Korean J Health Promot. 2015; 15(4):175–184. https://doi.org/10.15384/kjhp.2015.15.4.175.
Article30. Chae H. Relationships between obesity, body image perception, and weight control in adult women. Korean J Women Health Nurs. 2019; 25(2):129–142. https://doi.org/10.4069/kjwhn.2019.25.2.129.
Article31. Gu HM, Ryu SY, Park J, Han MA, Son YE. Comparison of diet quality and diversity according to obesity type among 19-64 year old Korean adults. Korean J Community Nutr. 2016; 21(6):545–557. https://doi.org/10.5720/kjcn.2016.21.6.545.
Article32. Albawardi NM, Jradi H, Al-Hazzaa HM. Levels and correlates of physical activity, inactivity and body mass index among Saudi women working in office jobs in Riyadh city. BMC Womens Health. 2016; 16:33. https://doi.org/10.1186/s12905-016-0312-8.
Article33. Mehboob B, Safdar NF, Zaheer S. Socio-economic, environmental and demographic determinants of rise in obesity among Pakistani women: a systematic review. J Pak Med Assoc. 2016; 66(9):1165–1172.34. Keshavarz M, Sénéchal M, Dombrowski SU, Meister D, Bouchard DR. Examining the role of sex on the benefits of muscle-strengthening activities for people living with obesity: a cross-sectional study. Health Sci Rep. 2022; 5(4):e720. https://doi.org/10.1002/hsr2.720.
Article35. Bennie JA, Ding D, De Cocker K. Dose-dependent associations of joint aerobic and muscle-strengthening exercise with obesity: a cross-sectional study of 280,605 adults. J Sport Health Sci. 2023; 12(2):186–193. https://doi.org/10.1016/j.jshs.2021.01.002.
Article36. Bellicha A, van Baak MA, Battista F, Beaulieu K, Blundell JE, Busetto L, et al. Effect of exercise training on weight loss, body composition changes, and weight maintenance in adults with overweight or obesity: an overview of 12 systematic reviews and 149 studies. Obes Rev. 2021; 22(Suppl 4):e13256. https://doi.org/10.1111/obr.13256.
Article37. Lopez P, Taaffe DR, Galvão DA, Newton RU, Nonemacher ER, Wendt VM, et al. Resistance training effectiveness on body composition and body weight outcomes in individuals with overweight and obesity across the lifespan: a systematic review and meta-analysis. Obes Rev. 2022; 23(5):e13428. https://doi.org/10.1111/obr.13428.
Article38. Strain T, Fitzsimons C, Kelly P, Mutrie N. The forgotten guidelines: cross-sectional analysis of participation in muscle strengthening and balance & co-ordination activities by adults and older adults in Scotland. BMC Public Health. 2016; 16(1):1108. https://doi.org/10.1186/s12889-016-3774-6.
Article39. Milton K, Varela AR, Strain T, Cavill N, Foster C, Mutrie N. A review of global surveillance on the muscle strengthening and balance elements of physical activity recommendations. J Frailty Sarcopenia Falls. 2018; 3(2):114–124. https://doi.org/10.22540/JFSF-03-114.
Article40. Huang X, Xu W, Chen R, Jiang Y, Li J, Xu S. Association between sleep duration and weight gain and incident overweight/obesity: longitudinal analyses from the China Health and Nutrition Survey. Sleep Breath. 2021; 25(2):1187–1194. https://doi.org/10.1007/s11325-020-02194-y.
Article41. Li Q. The association between sleep duration and excess body weight of the American adult population: a cross-sectional study of the national health and nutrition examination survey 2015-2016. BMC Public Health. 2021; 21(1):335. https://doi.org/10.1186/s12889-021-10369-9.
Article42. Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 2017; 32:246–256. https://doi.org/10.1016/j.sleep.2016.08.006.
Article43. Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017; 3(5):383–388. https://doi.org/10.1016/j.sleh.2017.07.013.
Article44. Broussard JL, Klein S. Insufficient sleep and obesity: cause or consequence. Obesity (Silver Spring). 2022; 30(10):1914–1916. https://doi.org/10.1002/oby.23539.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forecasting obesity prevalence in Korean adults for the years 2020 and 2030 by the analysis of contributing factors
- Association of pre-diabetes with increased obesity and depression in older male and female: A secondary analysis of the Korea National Health and Nutrition Examination Survey 2020
- Prevalence of Hyperuricemia and Its Association with Obesity in Korean Adults: Analysis Based on 2018 Korea National Health and Nutrition Examination Survey
- Obesity, hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: a special report of the 2020 Korea National Health and Nutrition Examination Survey
- Trends in Obesity Prevalence by Occupation Based on Korean National Health and Nutrition Examination Survey From 1998 to 2015